Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Afzal S, Minhas MK. Aspergillosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/CNSnontumoraspergillosis.html. Accessed April 3rd, 2025.
Definition / general
- Cerebral aspergillosis is an aggressive, rare form of invasive aspergillosis characterized by brain parenchymal or meningeal invasion by Aspergillus species
Essential features
- Invasion of either brain parenchyma or meninges by septate, branching fungal hyphae of Aspergillus spp. with associated inflammatory reaction
Terminology
- Neuroaspergillosis
- CNS aspergillosis
ICD coding
- ICD-10: B44.9 - aspergillosis, unspecified
Epidemiology
- Cerebral aspergillosis is a rare disease with poor prognosis and a high fatality rate
- Aspergillus fumigatus is the most common organism; however, Aspergillus flavus, Aspergillus niger and Aspergillus terreus are also known to cause infection of the central nervous system
- Aspergillus fumigatus mostly causes infection in immunocompromised individuals, while Aspergillus flavus, Aspergillus niger and Aspergillus terreus are mostly seen in immunocompetent hosts (Infect Dis Now 2021;51:654)
- Incidence, morbidity and mortality are on the rise, especially in patients with malignancies being treated with immunosuppressive drugs and in patients undergoing organ transplantation (Drugs 2007;67:1567)
- Post COVID-19 cases of cerebral aspergillosis have also been noted (Ann Med Surg (Lond) 2022;80:104122)
Sites
- Cavernous sinus, meninges, frontal lobe most common (Int J Neurosci 2017;127:339, Ann Med Surg (Lond) 2022;80:104122)
- Aspergillosis with brainstem and cerebellar involvement are extremely fatal (Neurosurg Clin N Am 1992;3:435)
Pathophysiology
- Hematogenous spread is more common in immunocompromised individuals
- Direct spread from infection of adjacent areas (paranasal sinuses, ear) can also occur
- Aspergillus spp. produce blood brain barrier altering toxins that ultimately damage neurons and astrocytes (Mycotoxin Res 2018;34:257)
- Aspergillus spp. are angiotropic and have the propensity to cause angioinvasion, leading to thrombosis, infarcts, aneurysms and meningitis (Front Med (Lausanne) 2017;4:113)
- Immunocompetent hosts may develop granulomas, brain abscesses and meningitis
Etiology
- Mostly affects immunocompromised individuals (transplant recipients)
- Patients with neutropenia associated with acute leukemia and its therapy (Med Mycol Case Rep 2019;27:17)
- Patients on prolonged corticosteroid therapy
- Can occur due to cranial trauma or neurosurgery in immunocompetent hosts
Clinical features
- Clinical features vary depending upon site and extent of infection
- Patients may present with fever, headache, focal neurological deficit, cranial nerve deficit, features of meningitis or intracranial bleed
- CNS infection is often associated with hemorrhage or infarcts (Medicine (Baltimore) 2020;99:e22911)
- Disease can be slowly progressive and with symptoms present for weeks to months
- In immunocompetent hosts, the presentation in brain parenchyma is often a mass lesion (aspergilloma) (Medicine (Baltimore) 2020;99:e22911)
Diagnosis
- Stereotactic brain biopsy with subsequent tissue culture and histopathological examination
- Cerebrospinal fluid (CSF) galactomannan and PCR (J Clin Microbiol 2016;54:428, Clin Microbiol Infect 2017;23:889.e1)
- Brain imaging is necessary (CT and MRI) but usually have no specific features (J Fungi (Basel) 2019;5:79)
- Potassium hydroxide (KOH) preparations can highlight Aspergillus species
Laboratory
- CSF usually shows lymphocytosis, elevated CSF proteins and decreased glucose but can be normal
- CSF galactomannan is elevated with mean levels of 1.8 ng/mL; serum galactomannan is also elevated in the majority of cases (Infect Dis Now 2021;51:654, J Clin Microbiol 2016;54:428)
- Serum and CSF beta D glucan (BDG) levels are elevated (J Pediatric Infect Dis Soc 2016;5:277)
- CSF Aspergillus PCR reportedly has 75% sensitivity and 98% specificity (Clin Microbiol Infect 2017;23:889.e1)
- CSF nanopore targeted sequencing, blood enzyme linked immunoassay (ELISA) and Aspergillus specific IgG antibody (BMC Neurol 2020;20:342)
Radiology description
- CNS aspergillosis can be divided into 2 forms: parenchymal lesions and meningeal lesions
- Neuroimaging usually shows brain abscesses, meningitis, cerebral infarcts, aneurysms and intradural abscesses
- CT findings are nonspecific (Rofo 2018;190:967)
- Most common MRI findings are T2W hyperintense abscess wall with onion layer-like hypointense zone; ring enhancement is noted after contrast media application (PLoS One 2016;11:e0152475)
Prognostic factors
- Cerebellar and brainstem involvement is a sign of poor prognosis (Neurosurg Clin N Am 1992;3:435)
Case reports
- 47 year old immunocompetent man with worsening headache over 2 weeks, leading to fatal subarachnoid hemorrhage (Minerva Anestesiol 2009;75:467)
- 54 year old man with persistent headache for 20 years (BMC Neurol 2020;20:342)
- 58 year old woman with intraventricular lesion, post COVID-19 (Ann Med Surg (Lond) 2022;80:104122)
- 64 year old man with diplopia, right sided hemiparesis and a mild headache (Front Med (Lausanne) 2017;4:113)
Treatment
- Antifungal therapy with voriconazole (triazoles) as first line therapy (Stud Mycol 2021;100:100115)
- In cases of azole resistant infection, monotherapy (or a combination) with amphotericin B or echinocandin can be given (Mycoses 2018;61:656)
- In cases of CNS aspergilloma, surgical resection with subsequent antifungal therapy can be sought (Surg Neurol Int 2020;11:211)
Gross description
- Usually, small biopsies are received
- Aspergilloma has an appearance of a necrotic mass
- Autopsy shows areas of hemorrhage and infarction in angioinvasive aspergillosis
Frozen section description
- Mixed inflammation, associated Aspergillus hyphae which are dichotomously branching (acute angle branching) and septate
- Associated granulomatous response may be appreciated
- Usually only performed if necessary to rule out neoplasm
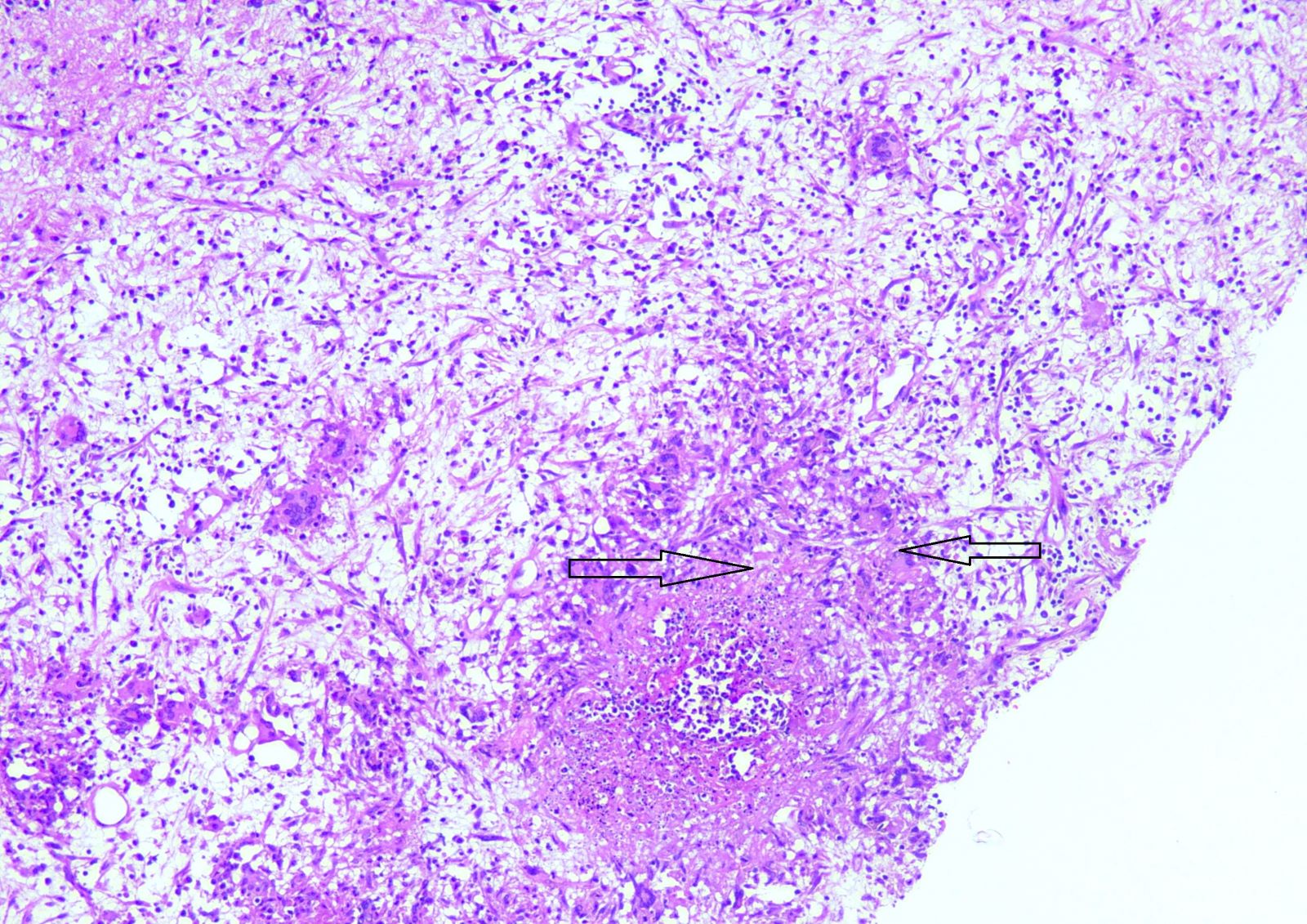
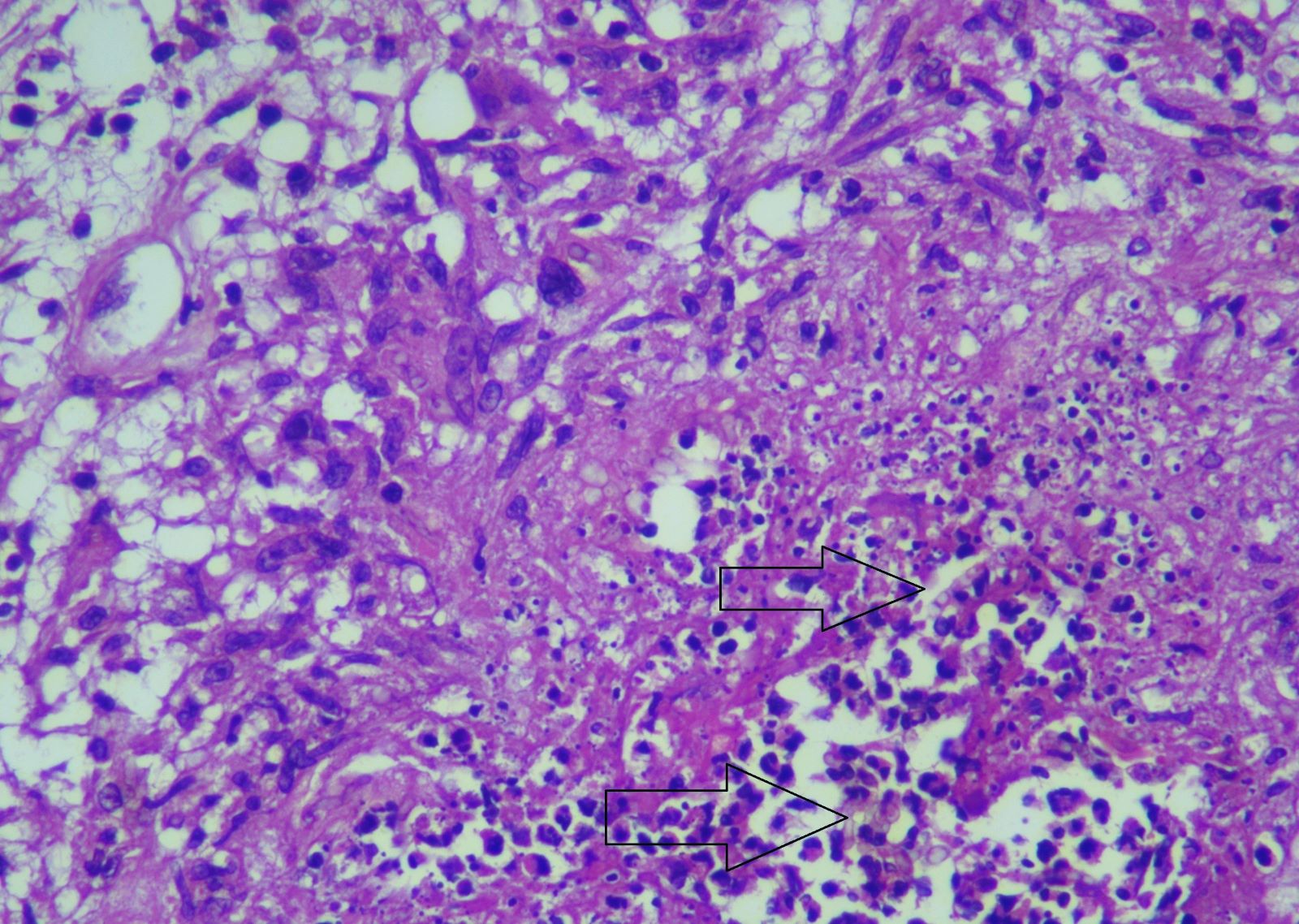
Microscopic (histologic) description
- Characteristic Aspergillus species comprising septate, branching hyphae (at acute angles) are seen
- Surrounding tissue usually shows acute on chronic inflammation
- Granulomatous response can be seen with adjacent areas of necrosis and an associated foreign body type of giant cell response
- Reference: Clin Microbiol Rev 1998;11:341
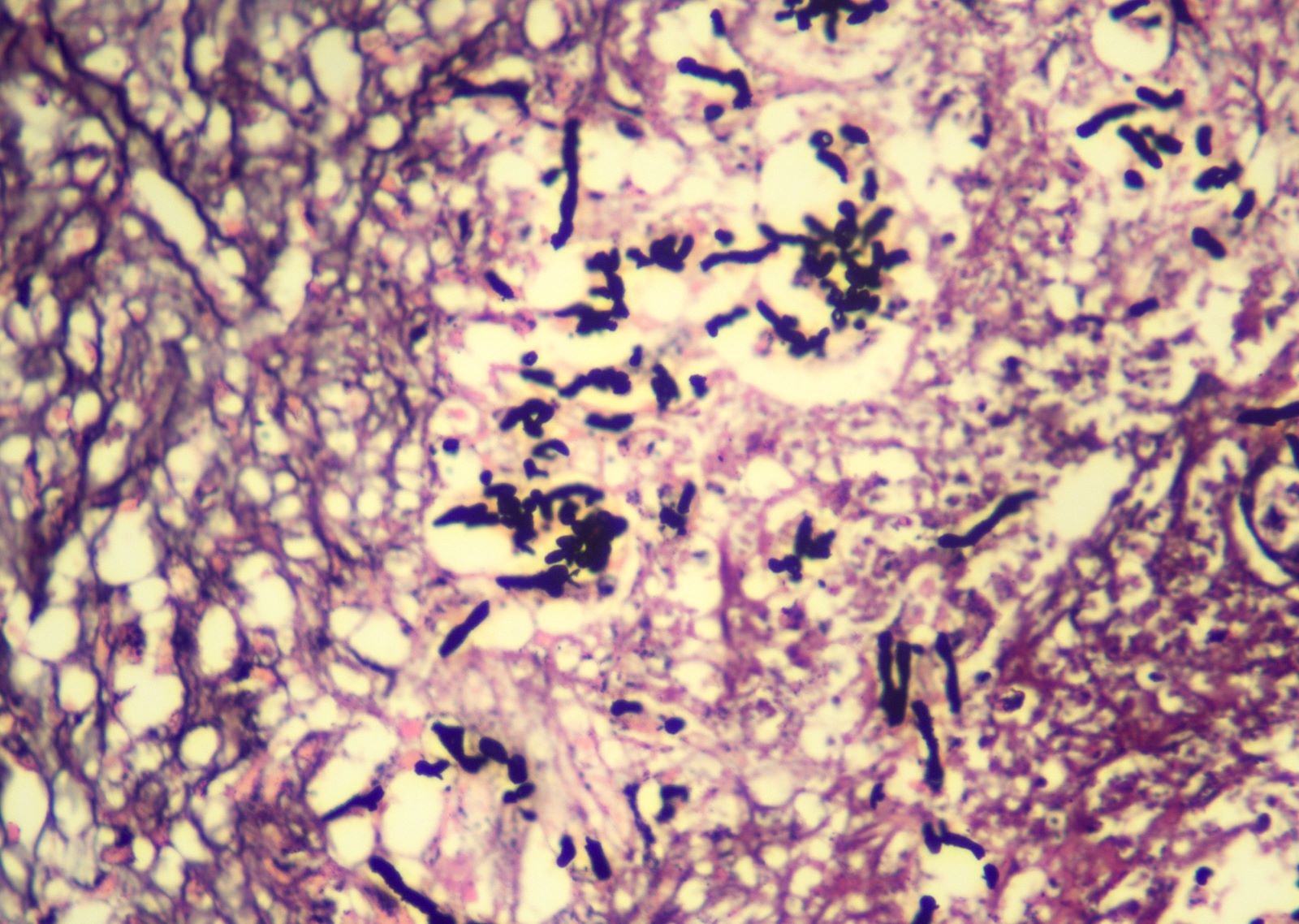
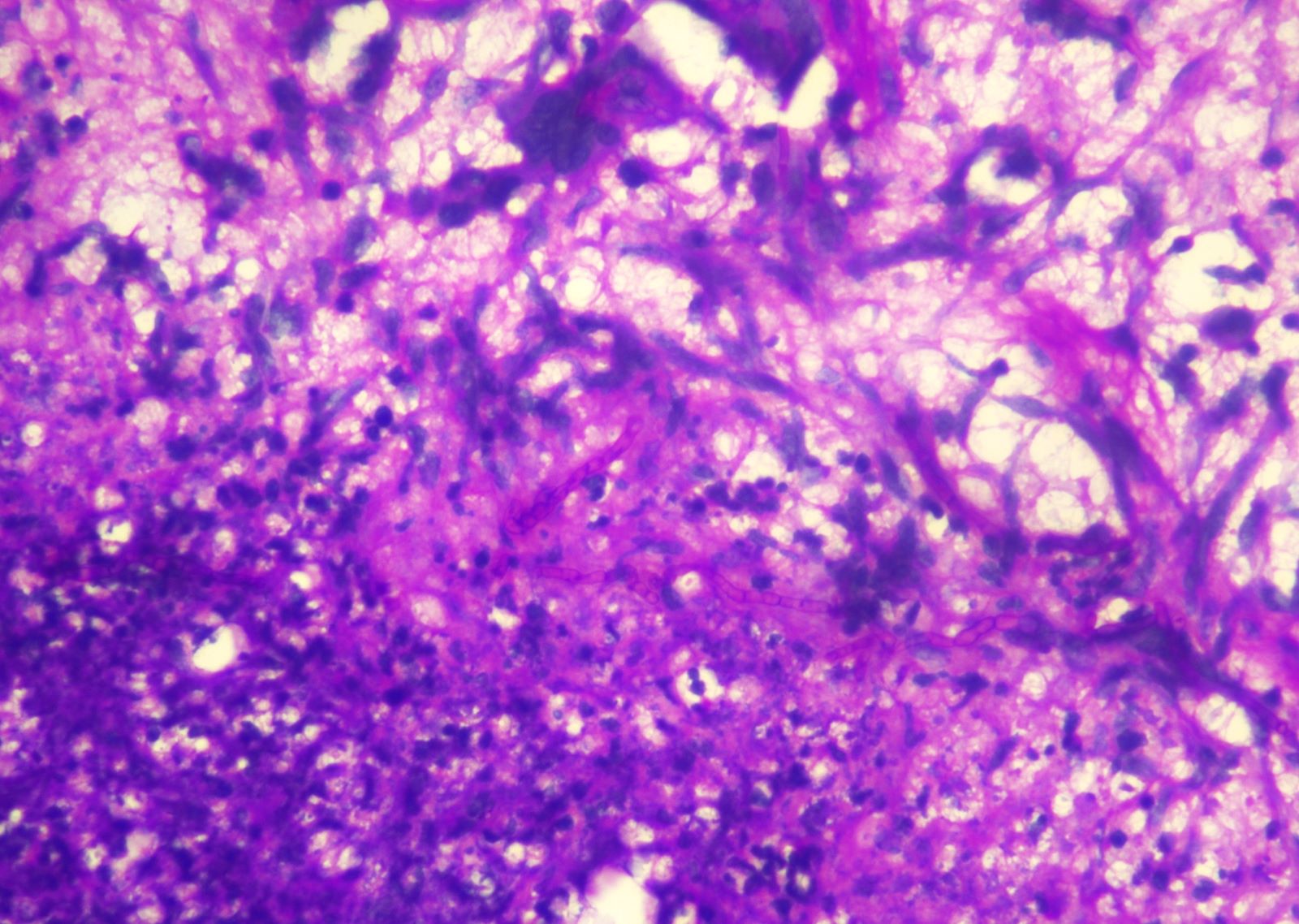
Microscopic (histologic) images
Positive stains
- PAS, PASD and GMS highlight thin branching, septate fungal hyphae
- Anti-Aspergillus antibody using immunohistochemistry (Med Mycol 2015;53:470)
Molecular / cytogenetics description
- ISH using the probe for Aspergillus species and a low viscosity hybridization buffer solution (Intern Med 1999;38:563)
Sample pathology report
- Brain mass, biopsy:
- Granulomatous inflammation with associated fungal infection, morphologically consistent with Aspergillus spp. (see comment)
- Comment: The biopsy reveals brain tissue showing numerous epithelioid granulomata with multinucleated giant cells. There are numerous septate, dichotomous, fungal hyphae, branching at acute angles. No angioinvasion is seen. PASD stain highlights the fungal hyphae.
Differential diagnosis
- Mucormycosis:
- Broad nonseptate hyphae
- Candida species:
- Spores and pseudohyphae are both present
- Thin septate branching hyphae
Board review style question #1
A 64 year old diabetic patient presented with altered sensorium and seizures. The cerebrospinal fluid (CSF) examination shows increased protein, decreased glucose and increased CSF galactomannan. These CSF findings are suggestive of an infection by which of the following?
- Aspergillus species
- Mucor species
- Neisseria meningitides
- Viral infection
Board review style answer #1
A. Aspergillus species. CSF galactomannan is raised in CSF and sometimes in serum in the patients of neuroaspergillosis.
Comment Here
Reference: Aspergillosis
Comment Here
Reference: Aspergillosis
Board review style question #2
A 40 year old woman, with a known case of systemic lupus erythematosus, presented with high grade fever and severe headache. Brain MRI showed a heterogenous appearing infiltrative lesion involving bilateral frontal lobes, with avid postcontrast enhancement. A biopsy for histopathological evaluation was performed and the microscopic features are shown above. Which of the following is the correct diagnosis?
- Cerebral aspergillosis
- Fungal meningitis secondary to Candida species
- Mucormycosis
- Tuberculous meningitis
- Viral meningitis
Board review style answer #2
A. Cerebral aspergillosis. The presence of septate fungal hyphae branching at acute angles is suggestive of cerebral aspergillosis.
Comment Here
Reference: Aspergillosis
Comment Here
Reference: Aspergillosis