Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gibbons K, Perry AM. Intravascular. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomadiffuseintra.html. Accessed December 22nd, 2024.
Definition / general
- Extranodal large B cell lymphoma characterized by lymphoma cells, predominantly within lumina of blood vessels, especially capillaries, with the exclusion of larger arteries and veins
- Few to no circulating lymphoma cells in peripheral blood
Essential features
- Rare, mature B cell lymphoma limited to intravascular spaces
- Most common in skin and central nervous system
- Classical variant most common clinical presentation (neurological and cutaneous manifestations)
- Neoplastic cells are located in lumina of small to intermediate sized vessels
- Lymphoma cells are large with prominent nucleoli and vesicular chromatin
- Pan B cell markers positive, as well as BCL2 and MUM1
- Aggressive behavior with short overall survival
Terminology
- Intravascular large B cell lymphoma (ILBCL)
- Malignant angioendotheliomatosis, angioendotheliomatosis proliferans syndrome, intravascular lymphomatosis, angioendothelilotropic lymphoma (all obsolete)
ICD coding
- ICD-O: 9712/3 - intravascular large B cell lymphoma
Epidemiology
- Rare; accounts for 1% of B cell lymphomas (Cancer Sci 2021;112:3953)
- Older patients; median age 70 years (Blood 2018;132:1561)
- Slightly more common in males
Sites
- Selective growth within lumina of small blood vessels, particularly capillaries
- Extranodal sites, including bone marrow, with sinusoidal or perivascular involvement
- Most common sites of involvement: skin, nervous system, kidneys, lungs, endocrine glands
- Lymph node involvement rare (Blood 2018;132:1561)
Pathophysiology
- Localization to blood vessel lumens partially explained by lack of CD29 (β1 integrin) and CD54 (ICAM1), both of which are important for transvascular lymphocyte migration (Blood 2018;132:1561)
Etiology
- Unknown
Clinical features
- Classic / western form:
- Clinical presentation ranges from a few mild symptoms (fever of unknown origin, pain, organ specific local symptoms) to severe symptoms (B symptoms and signs of multiorgan failure) (Cancer Sci 2021;112:3953)
- CNS involvement (present in 35%) with heterogeneous symptoms, including sensory and motor deficits or neuropathies, meningoradiculitis, paresthesias, hemiparesis, seizures and altered mental state
- Skin lesions (present in 40%) are heterogeneous, including painful indurated erythematous eruptions, cellulitis, peau d’orange, small red palpable spots, nodules with or without ulceration, tumors and erythematous and desquamated plaques (Blood 2018;132:1561)
- Lymphadenopathy typically absent
- May present with disseminated intravascular coagulation leading to critical bleeding after biopsy (Cancer Sci 2021;112:3953)
- Cutaneous variant:
- 25% of patients
- More frequent in western countries
- Patients usually younger, with a median age of 59
- Single or multiple skin lesions; no other sites involved
- Disease progression is less aggressive and associated with better overall survival (Blood 2018;132:1561)
- Hemophagocytic syndrome associated form:
- Presents in Asian populations with multiorgan failure, hepatosplenomegaly and pancytopenia
- Bone marrow infiltration common
- Skin and CNS involvement are rare
- Rapid aggressive onset and progression with median survival of 2 - 8 months (Blood 2018;132:1561)
Diagnosis
- Biopsy of affected or enlarged organ (Blood 2018;132:1561)
- Most commonly random skin biopsy in conjunction with bone marrow biopsy (Br J Haematol 2019;187:328)
Laboratory
- Anemia, leukopenia, thrombocytopenia and unexplained hypoxemia are most frequently observed
- Low levels of serum albumin
- High LDH and ferritin (Br J Haematol 2019;187:328)
Radiology description
- Lung involvement presents with ground glass appearance and nodules (Blood 2018;132:1561)
- Organ enlargement (liver, spleen, kidney and adrenal gland) is common (Cancer Sci 2021;112:3953)
- Brain MRI shows hyperintense lesions in pons, nonspecific white matter lesions, infarct-like lesions or meningeal enhancement
- PET CT can detect bone marrow involvement (Br J Haematol 2019;187:328)
Prognostic factors
- Median overall survival of 105 months, with chemotherapy 135 months
- 5 year survival of approximately 50 - 60% (Br J Haematol 2019;187:328)
Case reports
- 52 year old woman with diffusely PET avid kidneys (Intern Med 2017;56:827)
- 63 year old woman with multiple strokes (Medicine (Baltimore) 2018;97:e12793)
- 72 year old man with known right kidney tumor (Int J Surg Pathol 2021;29:653)
- 73 year old man with progressive exertional dyspnea, fever and calcified mediastinal lymphadenopathy (Respir Med Case Rep 2019;29:100989)
- 83 year old man with diffuse gallbladder wall thickening (Case Rep Radiol 2018;2018:2494207)
Treatment
- Chemoimmunotherapy usually with addition of CNS oriented therapy (Cancer Sci 2021;112:3953)
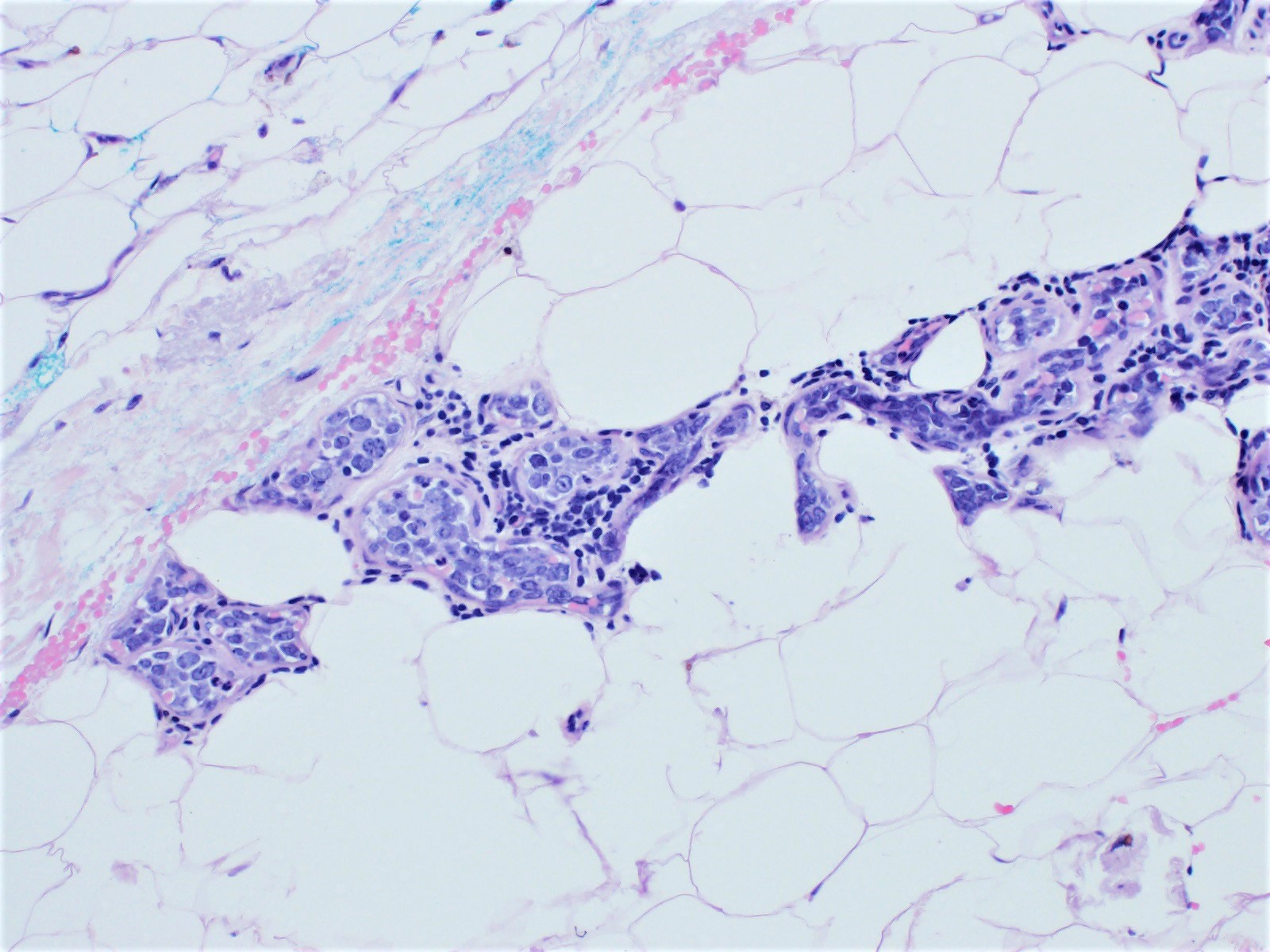
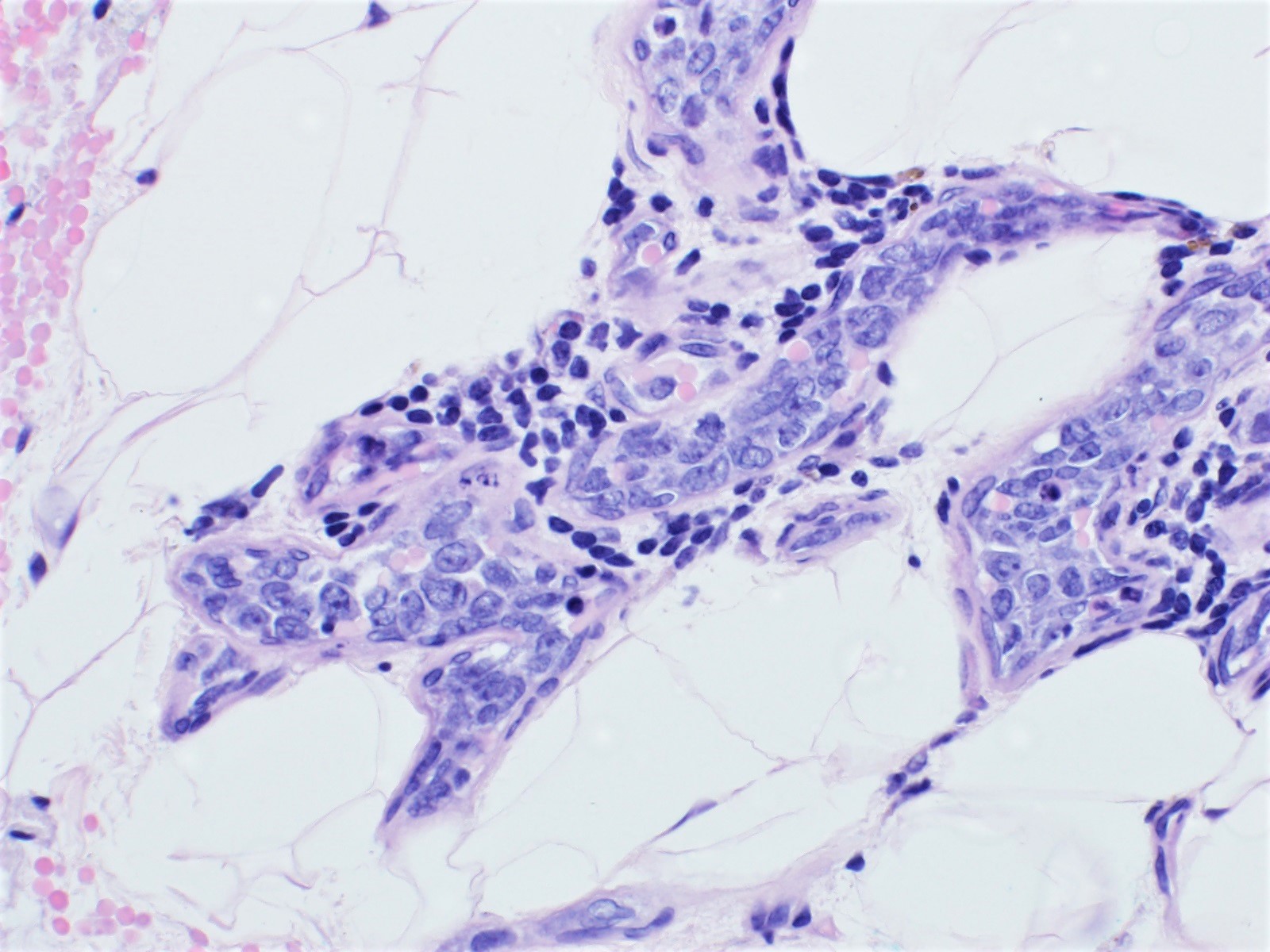
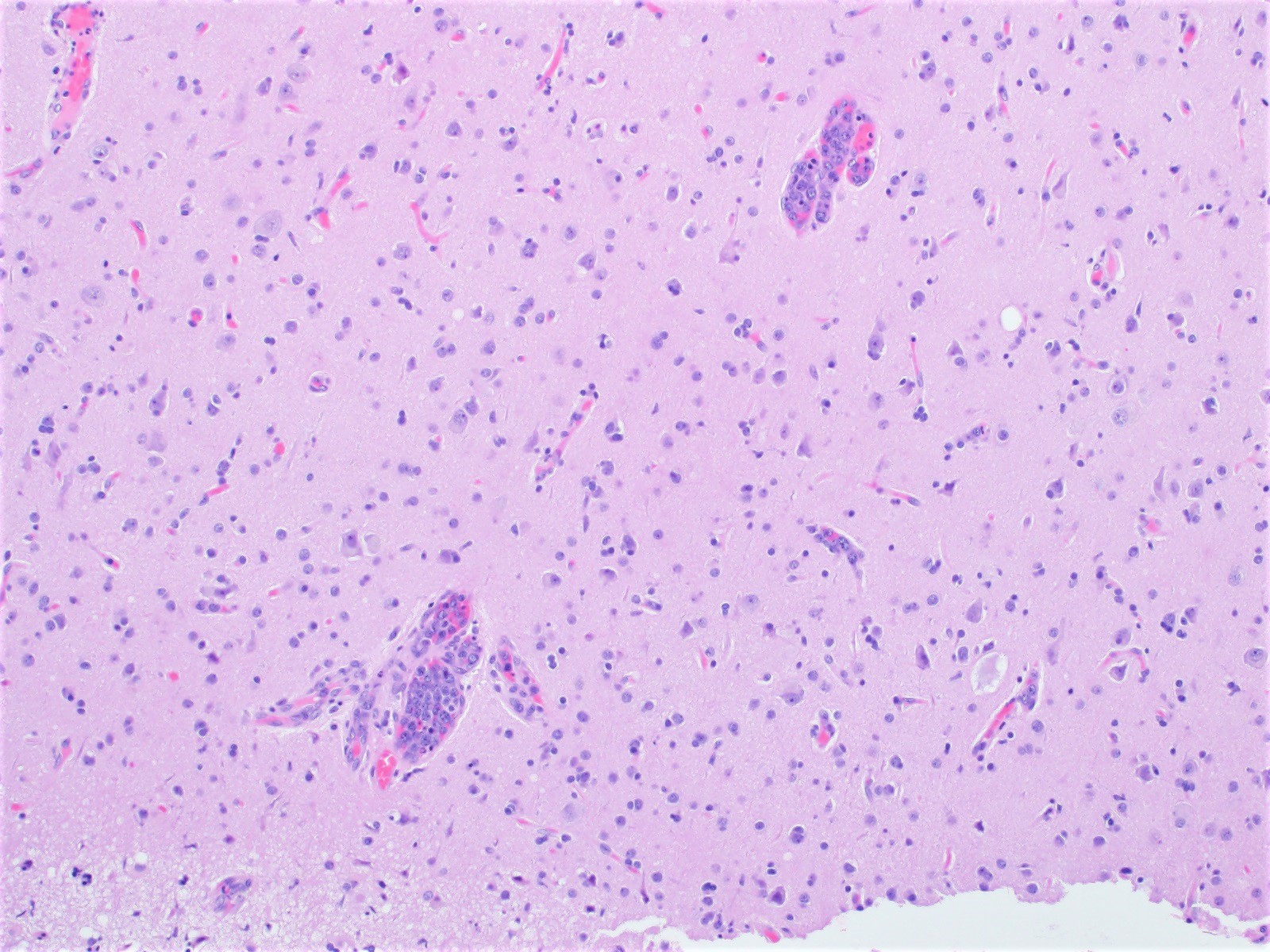
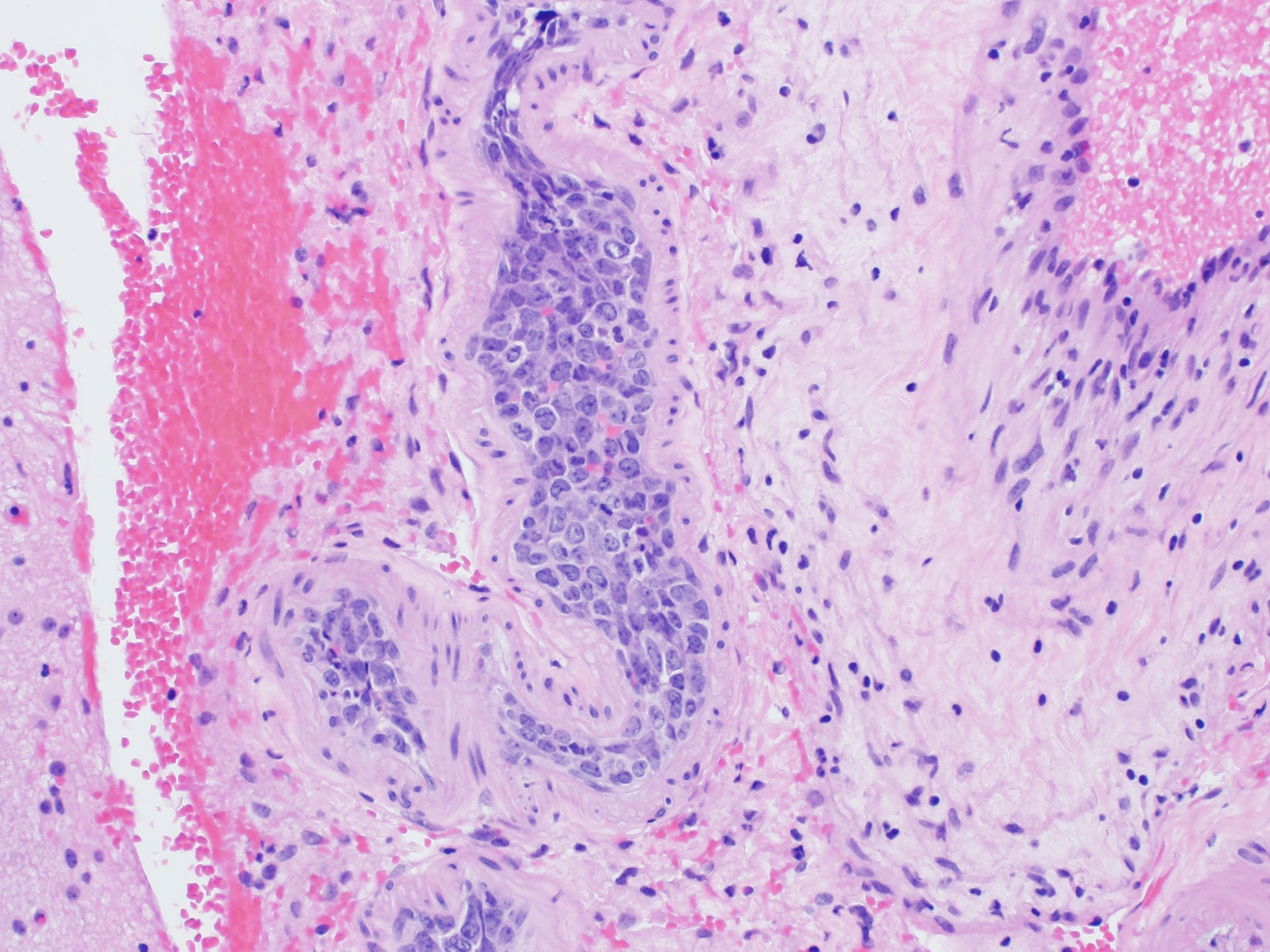
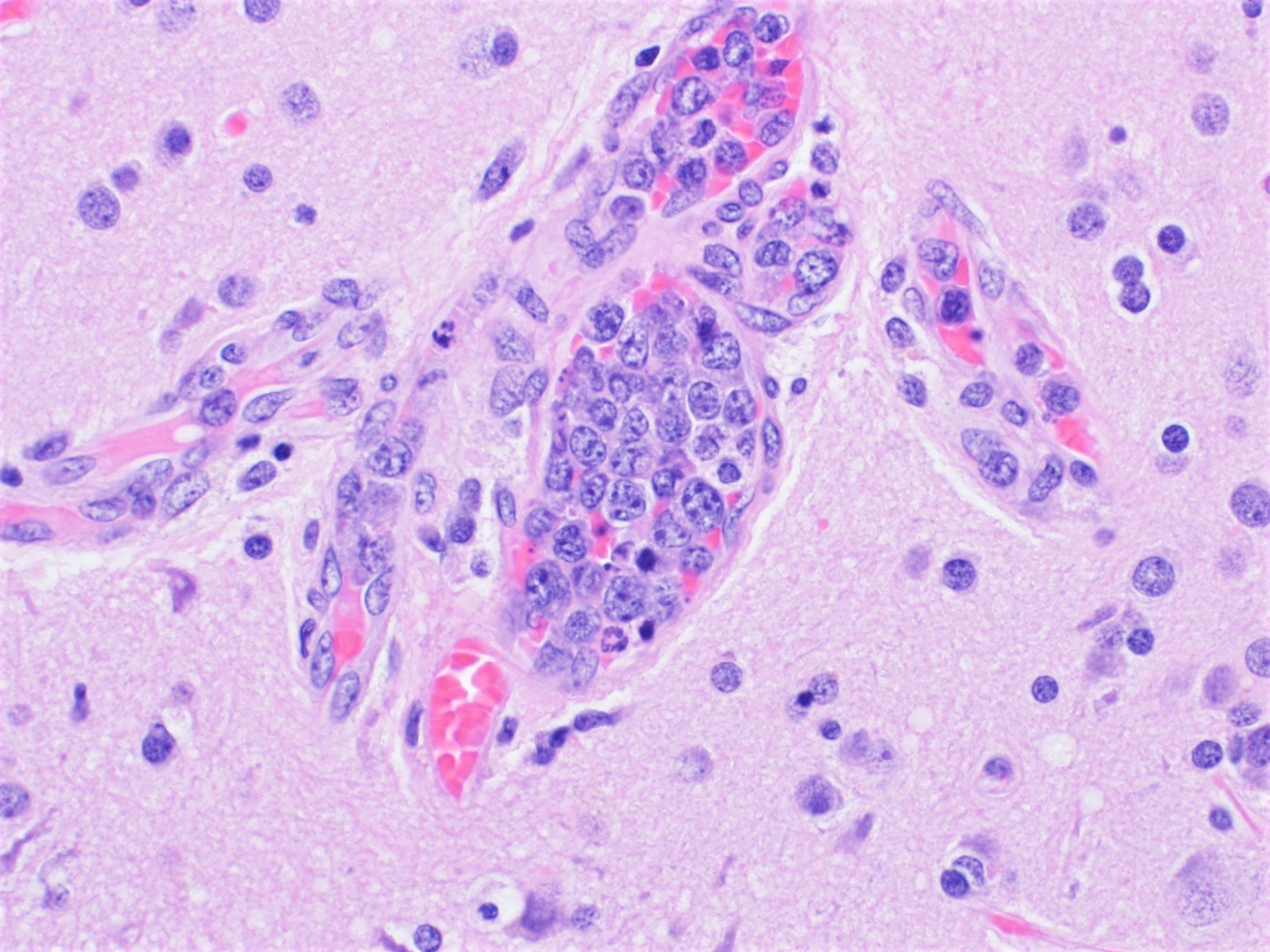
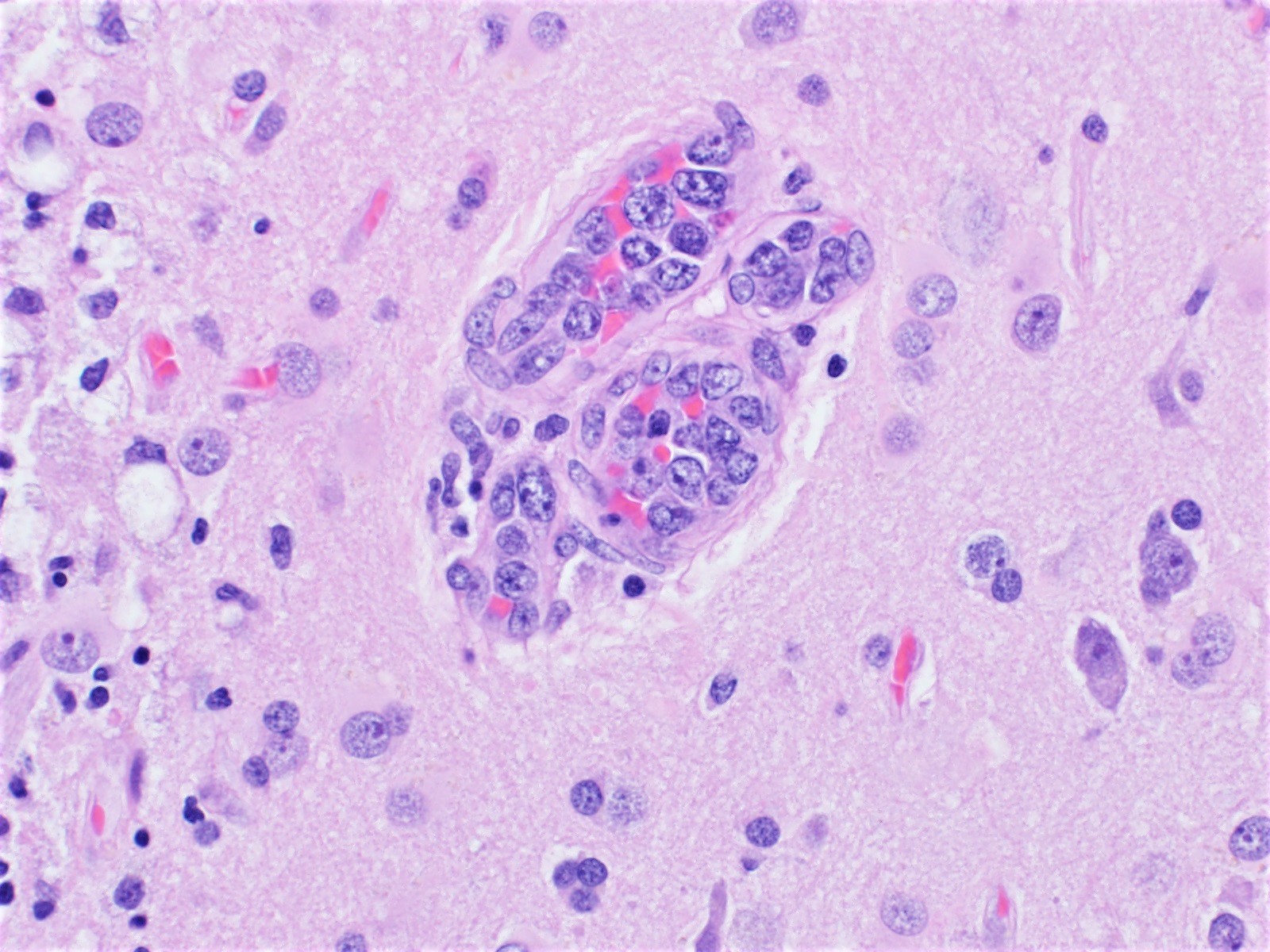
Microscopic (histologic) description
- Lymphoma cells can be found in any organ vessel lumina (Br J Haematol 2019;187:328)
- Lymphoma cells are large with high nuclear to cytoplasmic ratio with single or multiple prominent nucleoli and scant cytoplasm
- Morphologic spectrum from centroblasts to immunoblasts / plasmablasts, including rare forms with anaplastic morphology
- Different growth patterns:
- Discohesive - lymphoma cells are preferentially within the central portion of the blood vessels with a free floating appearance
- Cohesive pattern - lymphoma cells almost completely fill the lumen to the point that assessment of vascular structure tends to be difficult
- Marginating pattern - less frequent, lymphoma cells preferentially adhere to endothelium, leaving the central portion of the lumen free (Blood 2018;132:1561)
- Infiltration patterns in bone marrow:
- Pure intrasinusoidal infiltration - neoplastic cells are confined within the intrasinusoidal spaces
- Intrasinusoidal infiltration with extravasation - neoplastic cells proliferate within intrasinusoidal space but with extravasation
- Diffuse interstitial infiltration - neoplastic cells proliferate diffusely within bone marrow (Br J Haematol 2019;187:328)
Microscopic (histologic) images
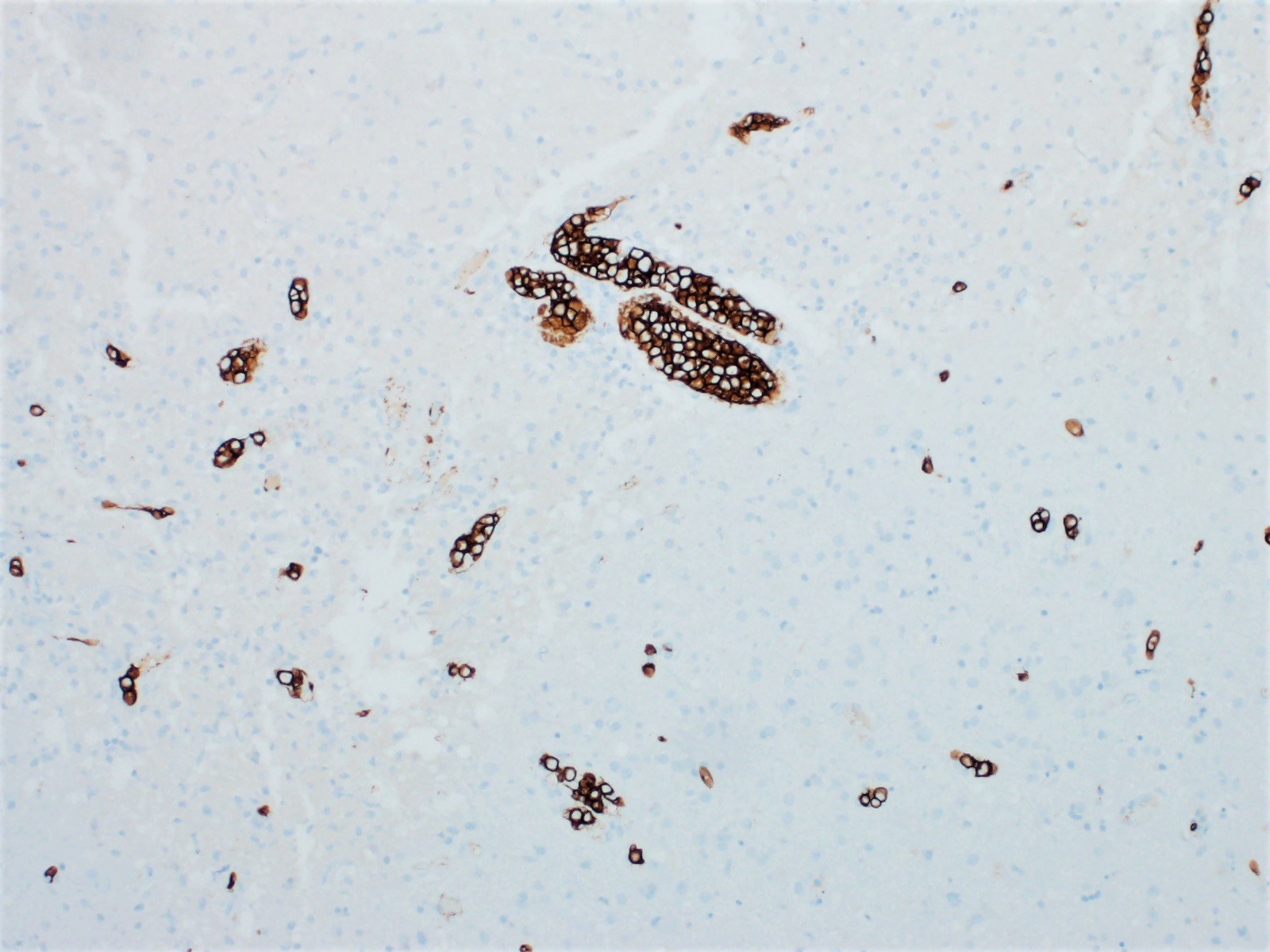
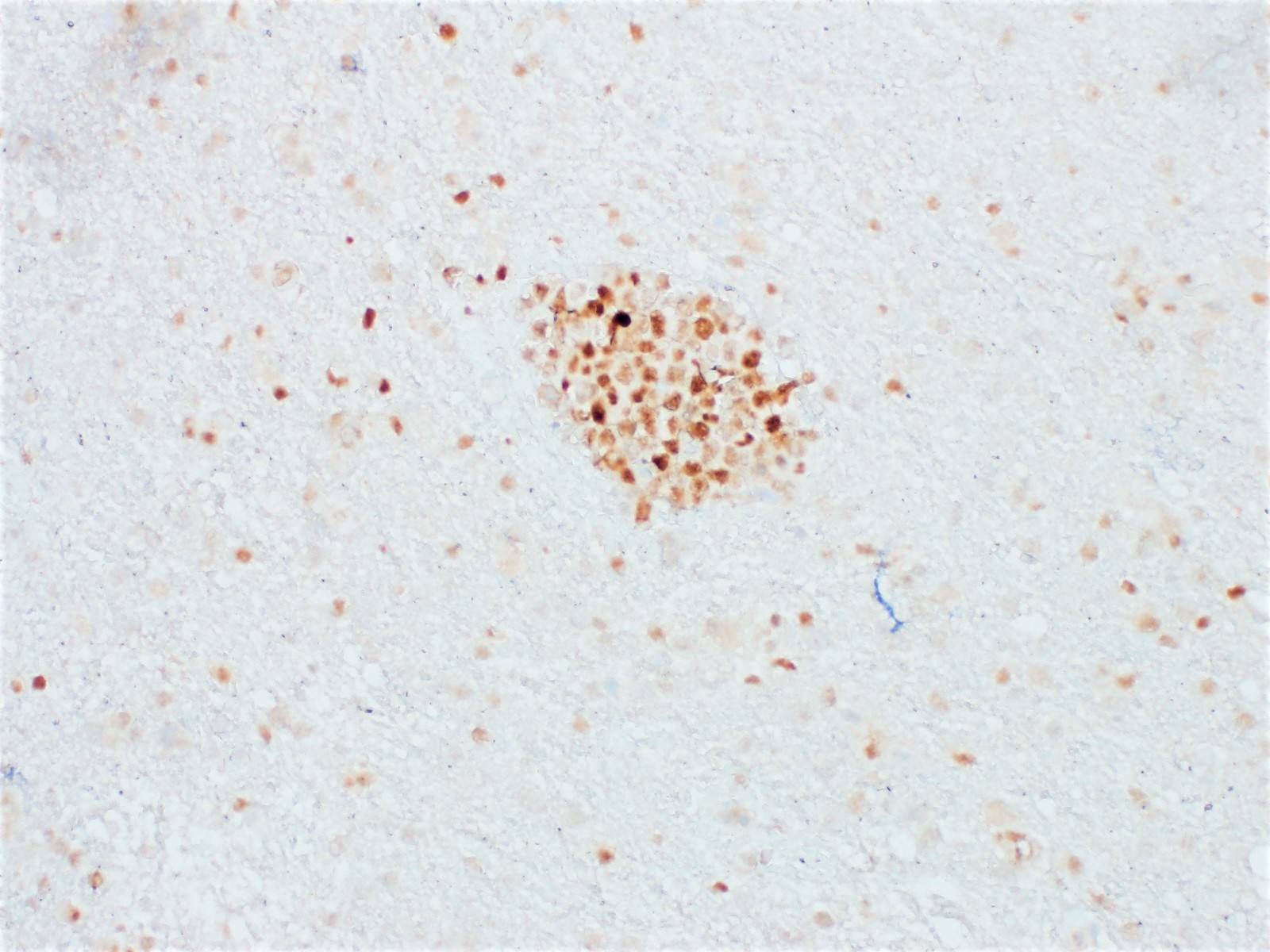
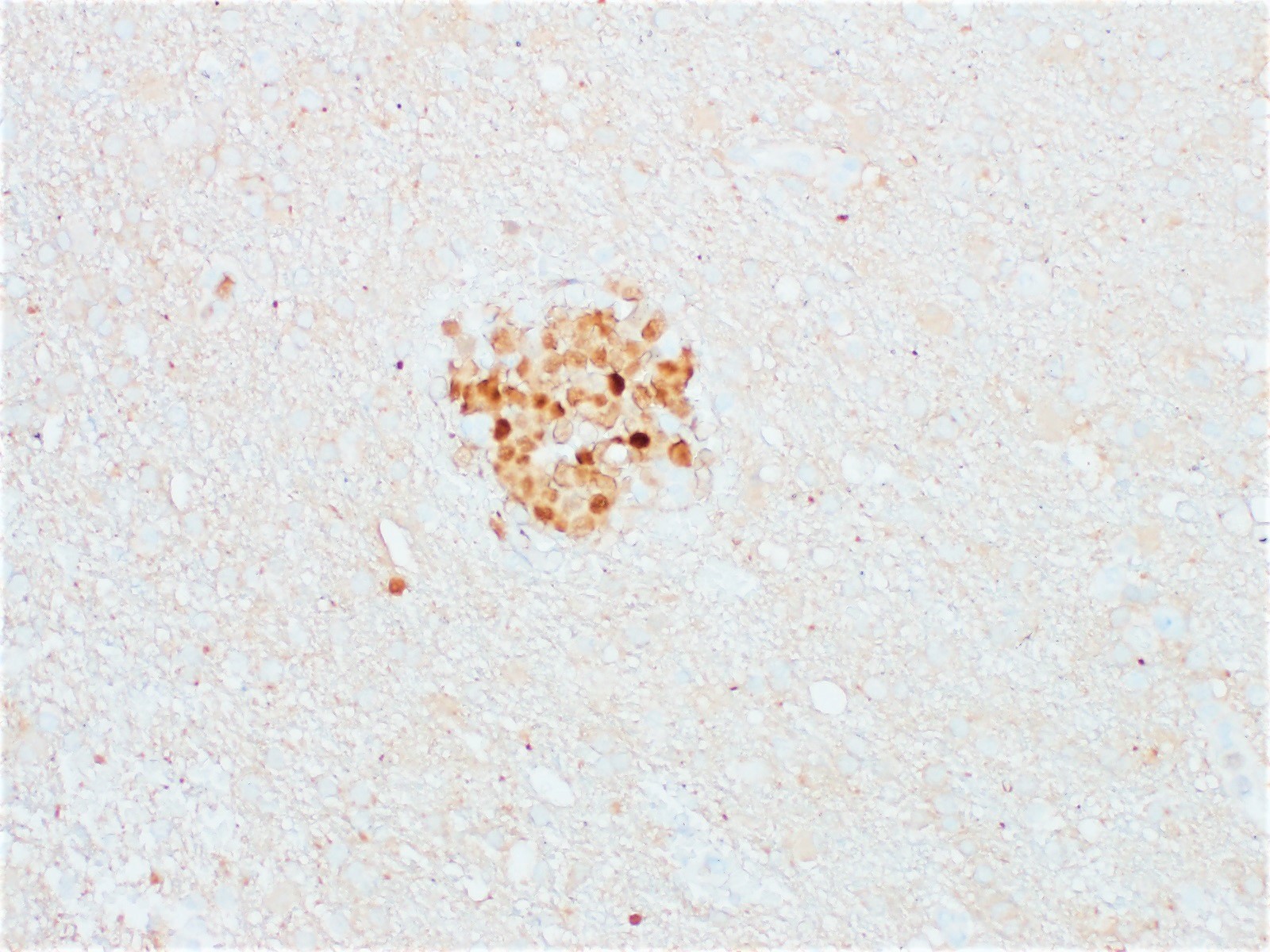
Positive stains
- Pan B cell markers: CD20, CD79a, PAX5
- BCL2 positive (Blood 2018;132:1561)
- Based on the Hans algorithm, 95% show nongerminal center phenotype with MUM1 / IRF4 expression (Cancer Sci 2021;112:3953)
- CD5 positive in 22 - 38% (Blood 2018;132:1561)
- Substantial proportion demonstrates PDL1 expression
- CD34 useful to highlight endothelium (Cancer Sci 2021;112:3953)
- Rare cases show positivity for EBV or HHV8 (Mod Pathol 2009;22:618, Diagn Pathol 2020;15:72, J Investig Med High Impact Case Rep 2014;2:2324709614526702)
Negative stains
- CD10 and BCL6 mostly negative (positive in approximately 20% of cases)
- Cyclin D1, CD30 (Blood 2018;131:2086)
Molecular / cytogenetics description
- Clonal rearrangements of immunoglobulin genes (Blood 2018;132:1561)
- MYD88 L265P in 44% (Blood 2018;131:2086)
- CD79b Y196 mutations in 26%
- Similar mutations to DLBCL, activated B cell type (Cancer Sci 2021;112:3953)
Sample pathology report
- Skin, left thigh, punch biopsy:
- Intravascular large B cell lymphoma (see comment)
- Comment: Biopsy shows large atypical CD20 positive B cells present within vascular spaces in the subcutaneous fat. These cells coexpress CD5, BCL6 and MUM1 and are negative for CD10 and CD3. Overall, these findings are consistent with intravascular large B cell lymphoma.
Differential diagnosis
- Lymphomatoid granulomatosis:
- Angiodestructive and angiocentric lesions showing a mixture of B cells, T cells, immunoblasts and histiocytes
- B cells are EBV positive
- Primary CNS lymphoma:
- Lymphoma cells infiltrate brain parenchyma
- Diffuse large B cell lymphoma:
- Cytologically and immunophenotypically identical cells but typically presents with lymphadenopathy or mass
- CNS vasculitis:
- Cells are less atypical and involve vessel walls in addition to vessel lumina (Arch Pathol Lab Med 2012;136:333)
- Other lymphomas presenting as intravascular lymphoma:
- Extracavitary primary effusion lymphoma as well as T and NK/T cell lymphomas, in rare cases, have been reported to show an intravascular pattern (Am J Surg Pathol 2014;38:426, BMC Cancer 2018;18:1115, Am J Surg Pathol 2013;37:617)
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following combinations of immunohistochemical stains is most consistent with immunophenotypic profile of intravascular large B cell lymphoma?
- CD20+, CD3-, CD5-, CD10+, BCL6+, BCL2+, c-MYC+
- CD20+, CD5+, Cyclin D1+
- CD20+, PAX5+, MUM1+, BCL2+
- CD20-, CD2+, CD3+, CD5-, CD7+, CD56+
Board review style answer #2