23 October 2024 - Case of the Month #543
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Vidya Arole and Dr. Wei Chen, Ohio State University Wexner Medical Center, Columbus, Ohio, USA for contributing this case and discussion and to Dr. Claudio Luchini, University and Hospital Trust of Verona, Verona, Italy for reviewing the discussion.
Paid advertisement
Case of the Month #543
Clinical history:
A 70 year old man underwent upper endoscopic ultrasound (EUS) for evaluation of a pancreatic cyst. An incidental finding of mucosal discoloration in the entire duodenum was noted.
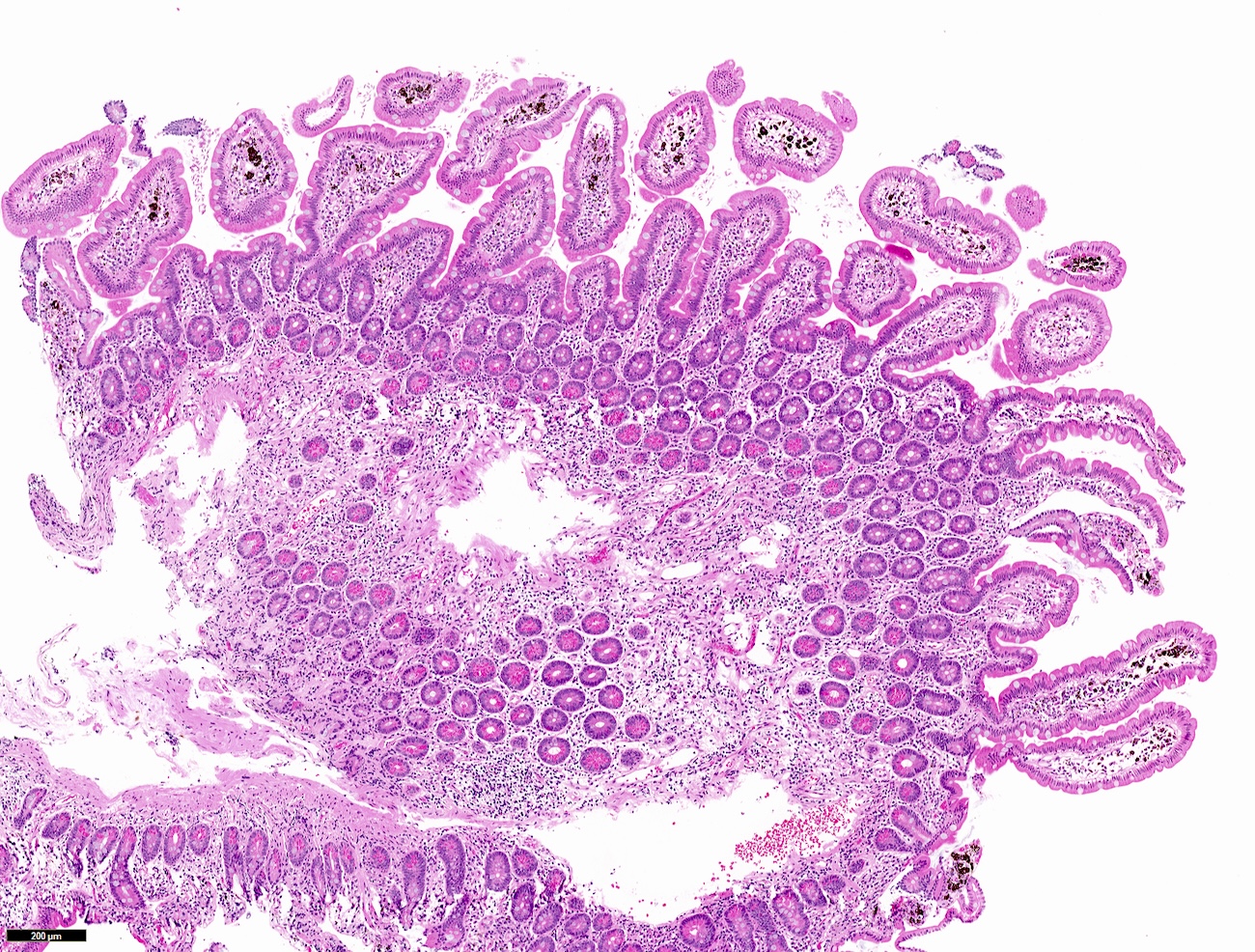
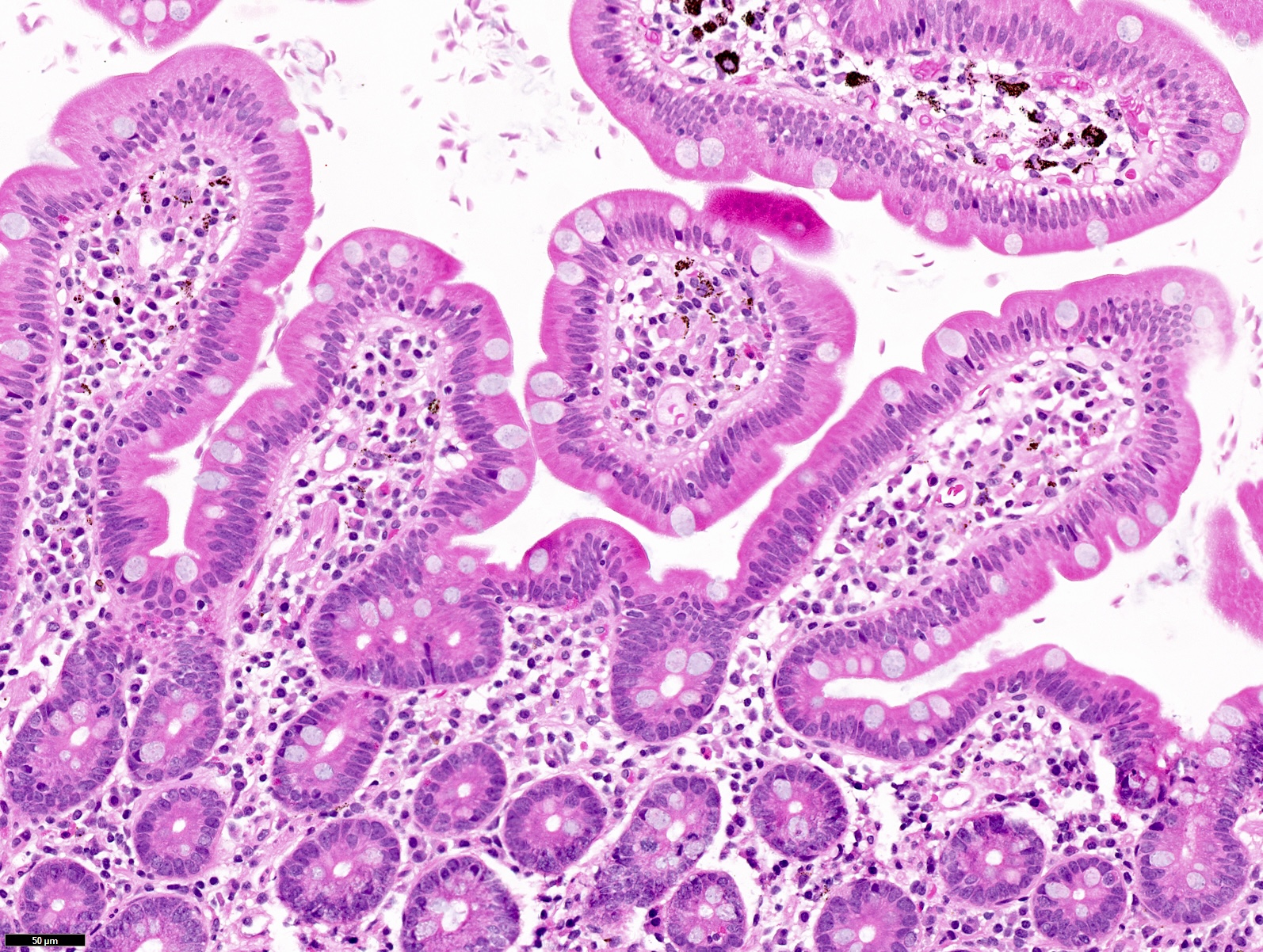
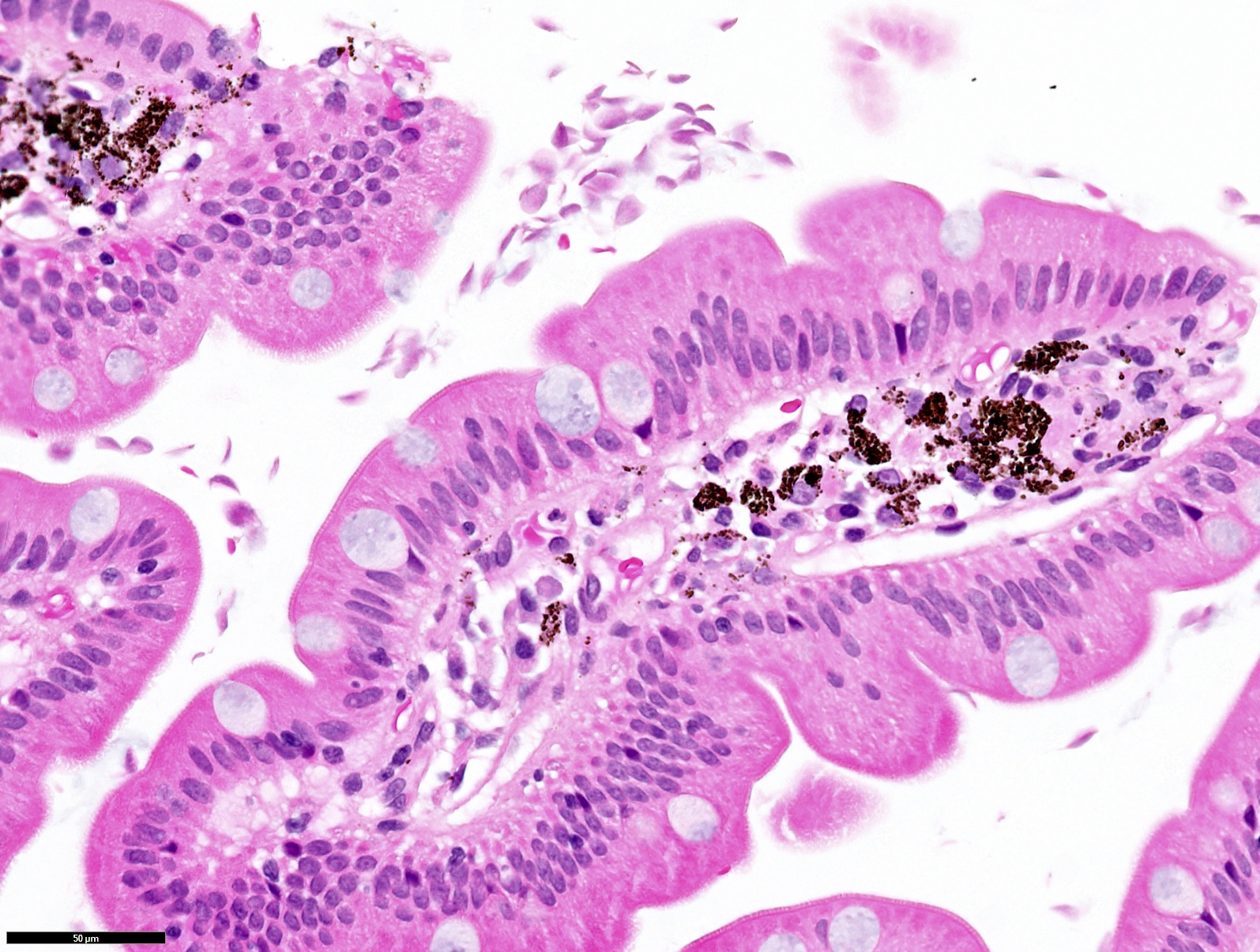
Microscopic images:
What is your diagnosis?
Diagnosis: Pseudomelanosis duodeni; giardiasis
Test questions (answer at the end):
1. The brown, black pigment shown in these samples would be positive for which of the following stains?
2. In these patients, it is necessary to evaluate for which of the following additional diseases / pathologies?
Discussion:
Pseudomelanosis duodenei
Pseudomelanosis duodenei, also known as duodenal pseudomelanosis, is characterized by the accumulation of brownish black pigment in the lamina propria confined to duodenal villous tips. Endoscopically, the duodenal mucosa shows black dots. It is an incidental finding without any clinical consequences. The pigment is thought to be iron and sulfur and has been shown to be positive for Prussian blue and Fontana-Masson stains. The mechanism / underlying pathogenesis is not fully understood but it is commonly associated with certain medical conditions such as hypertension, diabetes mellitus, chronic renal disease and related medical treatment with sulfur containing diuretics. Together these medical conditions and associated therapies are thought to play a role in pigment deposition and accumulation (Diagnostics (Basel) 2021;11:1974).
Psuedomelanosis duodenei is distinct from melanosis coli. Melanosis coli is diffuse colonic lipofuscin pigment deposition in the settings of excessive laxative use.
Giardiasis
It is important to always look out for more than one diagnosis when examining the slides. In addition to duodenal pseudomelanosis, the intervillous spaces show crescent moon / pear shaped pale translucent organisms. Giardia lamblia / Giardia intestinalis is a common intestinal parasite (flagellate protozoa) that usually causes malodorous diarrhea, abdominal cramping, bloating and nausea. Transmission is fecal-oral and most infections are asymptomatic. The recommended diagnostic method is stool antigen detection or nucleic acid amplification testing (NAAT). Duodenal aspirate microscopy is the next step if stool studies are nondiagnostic with high suspicion for Giardia. Duodenal biopsy is not commonly used for diagnosis. The endoscopic appearance of duodenal infection is nonspecific with normal mucosa to blunting of villi resembling celiac sprue. Histologically, giardiasis can be sneaky without inflammatory changes in the mucosa, like in this case; however, there could be variable villous blunting with increased intraepithelial lymphocytes and inflammatory expansion of lamina propria with prominent lymphoid aggregate. The presence of crescent shaped noninvasive trophozoites that are free floating in the lumen, adherent to epithelial surface or located in the cytoplasm of epithelial cells are diagnostic. Trophozoites are shown to be positive for special stains methylene blue, Giemsa and CD117 / KIT immunostain (Hum Pathol 2009;40:323). Whenever the diagnosis of Giardiasis is made, checking for plasma cells in the lamina propria is recommended to rule out second pathology of common variable immunodeficiency (CVID).
Test question answers:
1. C. Prussian blue. The brown, black pigment in pseudomelanosis duodeni is thought to contain ferrous sulfide and has been shown to be positive on Prussian blue iron stain and Masson Fontana melanin stain. Answer A is incorrect because GMS stain is used for fungal organisms. Answer B is incorrect because PAS is used to detect glycogen deposits and lipofuscin in melanosis coli. Answer D is incorrect because Von Kossa stains calcium.
2. B. CVID - look for absence of plasma cells. Checking for plasma cells in the lamina propria is recommended in patients with giardiasis as they are often seen in patients with CVID due to chronic giardiasis. Answers A, C and D are incorrect because neither pseudomelanosis nor giardiasis is associated with any of these options.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Vidya Arole and Dr. Wei Chen, Ohio State University Wexner Medical Center, Columbus, Ohio, USA for contributing this case and discussion and to Dr. Claudio Luchini, University and Hospital Trust of Verona, Verona, Italy for reviewing the discussion.
Paid advertisement
Website news:
(1) We have posted our most recent What’s New in Neuropathology newsletter by Drs. Heather Smith and Jared Ahrendsen. This edition of our What’s New in Pathology newsletter focuses on CNS WHO 5th edition updates. You can read our past newsletters and subscribe to all of our future What’s New in Pathology newsletters on our Newsletters page.
(2) New Editorial Board appointments: Dr. Rachel Multz was recently appointed to our Resident / Fellow Advisory Board for Neuropathology. Dr. Umberto Maccio was appointed to our Board of Reviewers for Immunohistochemistry. Dr. Alexei Mikhailov was appointed to our Board of Reviewers for Medical Renal Pathology.
(3) The Q2 report for our Worldwide Directory of Pathologists is available to read at pathologyoutlines.com/directoryreport2024q2.html. It provides pathologist totals by U.S. state and Canadian province, subspecialty totals, the largest pathology institutions and the most popular pathologist profiles.
Visit and follow our Blog to see recent updates to the website.
(1) We have posted our most recent What’s New in Neuropathology newsletter by Drs. Heather Smith and Jared Ahrendsen. This edition of our What’s New in Pathology newsletter focuses on CNS WHO 5th edition updates. You can read our past newsletters and subscribe to all of our future What’s New in Pathology newsletters on our Newsletters page.
(2) New Editorial Board appointments: Dr. Rachel Multz was recently appointed to our Resident / Fellow Advisory Board for Neuropathology. Dr. Umberto Maccio was appointed to our Board of Reviewers for Immunohistochemistry. Dr. Alexei Mikhailov was appointed to our Board of Reviewers for Medical Renal Pathology.
(3) The Q2 report for our Worldwide Directory of Pathologists is available to read at pathologyoutlines.com/directoryreport2024q2.html. It provides pathologist totals by U.S. state and Canadian province, subspecialty totals, the largest pathology institutions and the most popular pathologist profiles.
Visit and follow our Blog to see recent updates to the website.
Case of the Month #543
Clinical history:
A 70 year old man underwent upper endoscopic ultrasound (EUS) for evaluation of a pancreatic cyst. An incidental finding of mucosal discoloration in the entire duodenum was noted.
Microscopic images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Pseudomelanosis duodeni; giardiasis
Test questions (answer at the end):
1. The brown, black pigment shown in these samples would be positive for which of the following stains?
- GMS
- PAS
- Prussian blue
- Von Kossa
2. In these patients, it is necessary to evaluate for which of the following additional diseases / pathologies?
- Celiac disease - look for increased intraepithelial lymphocytes and villous blunting
- Common variable immunodeficiency (CVID) - look for absence of plasma cells
- Inflammatory bowel disease - look for granulomas
- Primary melanoma - look for atypical cells
Discussion:
Pseudomelanosis duodenei
Pseudomelanosis duodenei, also known as duodenal pseudomelanosis, is characterized by the accumulation of brownish black pigment in the lamina propria confined to duodenal villous tips. Endoscopically, the duodenal mucosa shows black dots. It is an incidental finding without any clinical consequences. The pigment is thought to be iron and sulfur and has been shown to be positive for Prussian blue and Fontana-Masson stains. The mechanism / underlying pathogenesis is not fully understood but it is commonly associated with certain medical conditions such as hypertension, diabetes mellitus, chronic renal disease and related medical treatment with sulfur containing diuretics. Together these medical conditions and associated therapies are thought to play a role in pigment deposition and accumulation (Diagnostics (Basel) 2021;11:1974).
Psuedomelanosis duodenei is distinct from melanosis coli. Melanosis coli is diffuse colonic lipofuscin pigment deposition in the settings of excessive laxative use.
Giardiasis
It is important to always look out for more than one diagnosis when examining the slides. In addition to duodenal pseudomelanosis, the intervillous spaces show crescent moon / pear shaped pale translucent organisms. Giardia lamblia / Giardia intestinalis is a common intestinal parasite (flagellate protozoa) that usually causes malodorous diarrhea, abdominal cramping, bloating and nausea. Transmission is fecal-oral and most infections are asymptomatic. The recommended diagnostic method is stool antigen detection or nucleic acid amplification testing (NAAT). Duodenal aspirate microscopy is the next step if stool studies are nondiagnostic with high suspicion for Giardia. Duodenal biopsy is not commonly used for diagnosis. The endoscopic appearance of duodenal infection is nonspecific with normal mucosa to blunting of villi resembling celiac sprue. Histologically, giardiasis can be sneaky without inflammatory changes in the mucosa, like in this case; however, there could be variable villous blunting with increased intraepithelial lymphocytes and inflammatory expansion of lamina propria with prominent lymphoid aggregate. The presence of crescent shaped noninvasive trophozoites that are free floating in the lumen, adherent to epithelial surface or located in the cytoplasm of epithelial cells are diagnostic. Trophozoites are shown to be positive for special stains methylene blue, Giemsa and CD117 / KIT immunostain (Hum Pathol 2009;40:323). Whenever the diagnosis of Giardiasis is made, checking for plasma cells in the lamina propria is recommended to rule out second pathology of common variable immunodeficiency (CVID).
Test question answers:
1. C. Prussian blue. The brown, black pigment in pseudomelanosis duodeni is thought to contain ferrous sulfide and has been shown to be positive on Prussian blue iron stain and Masson Fontana melanin stain. Answer A is incorrect because GMS stain is used for fungal organisms. Answer B is incorrect because PAS is used to detect glycogen deposits and lipofuscin in melanosis coli. Answer D is incorrect because Von Kossa stains calcium.
2. B. CVID - look for absence of plasma cells. Checking for plasma cells in the lamina propria is recommended in patients with giardiasis as they are often seen in patients with CVID due to chronic giardiasis. Answers A, C and D are incorrect because neither pseudomelanosis nor giardiasis is associated with any of these options.