21 June 2023 - Case of the Month #528
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Bin Xu, Memorial Sloan Kettering Cancer Center, New York, New York, USA for contributing this case and discussion and to Dr. Marc Pusztaszeri, McGill University, Montreal, Quebec, Canada for reviewing the discussion.

Advertisement
Case of the Month #528
Clinical history:
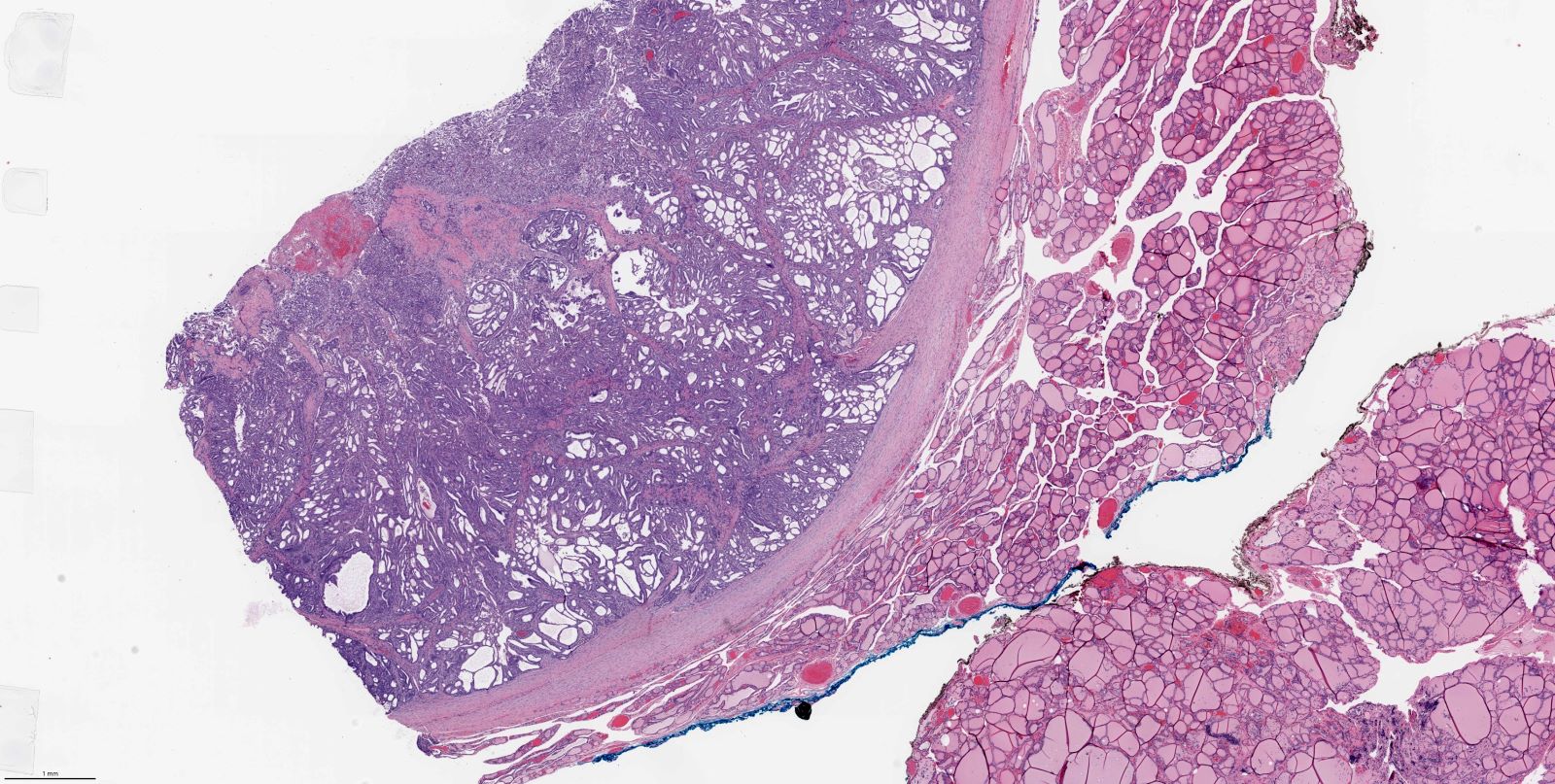
A 19 year old woman presented with a 3.7 cm thyroid mass.
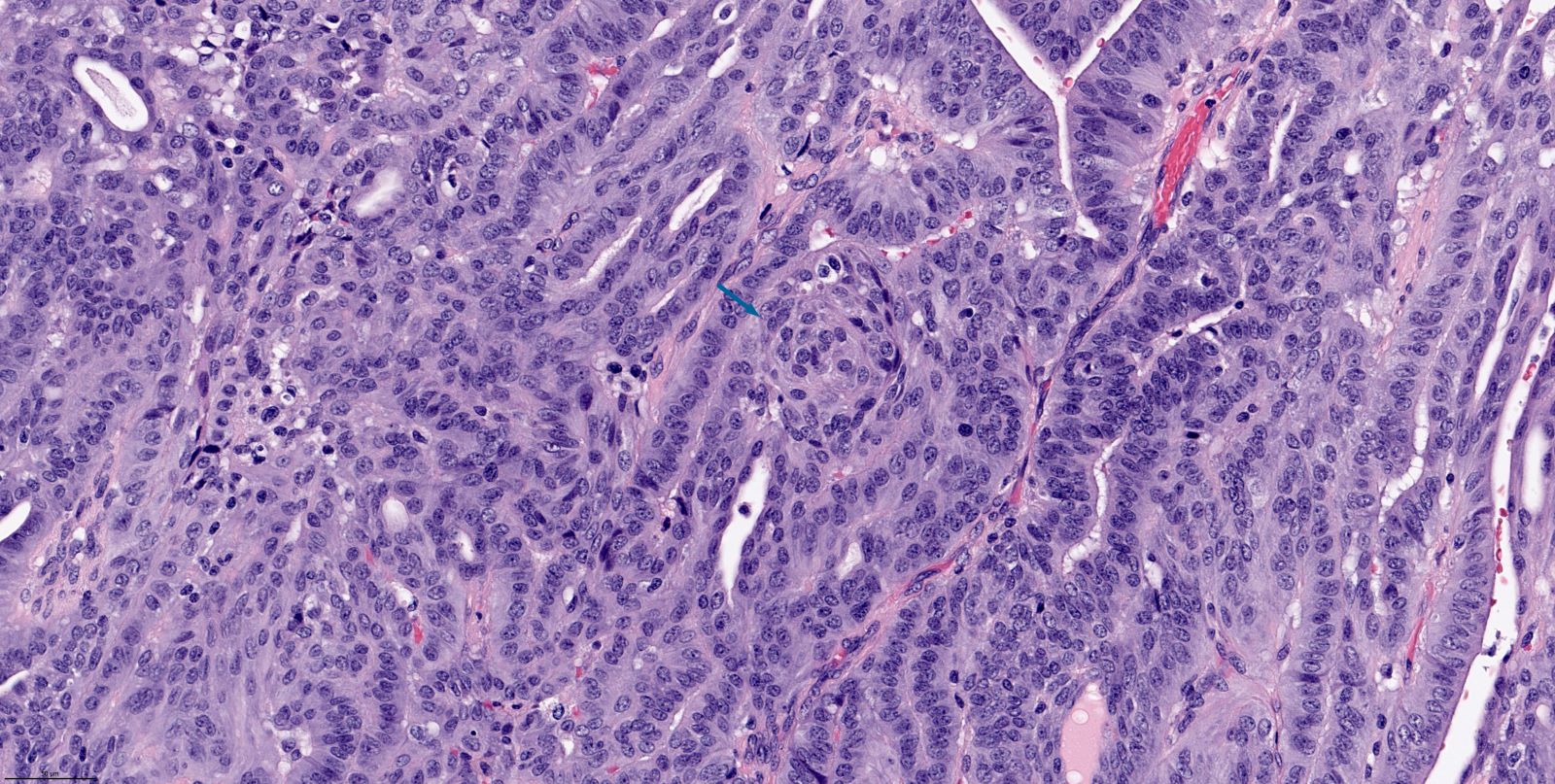
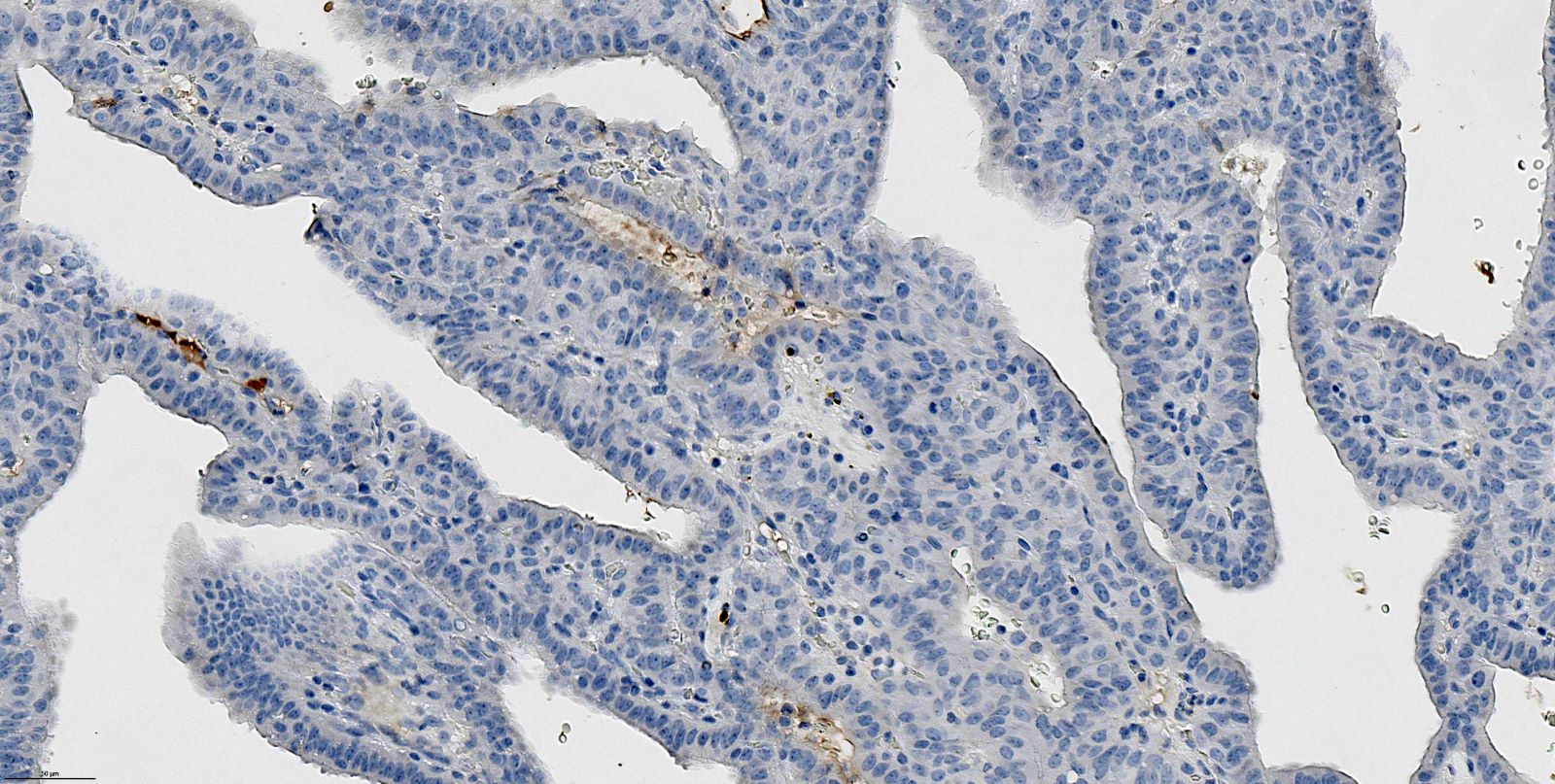
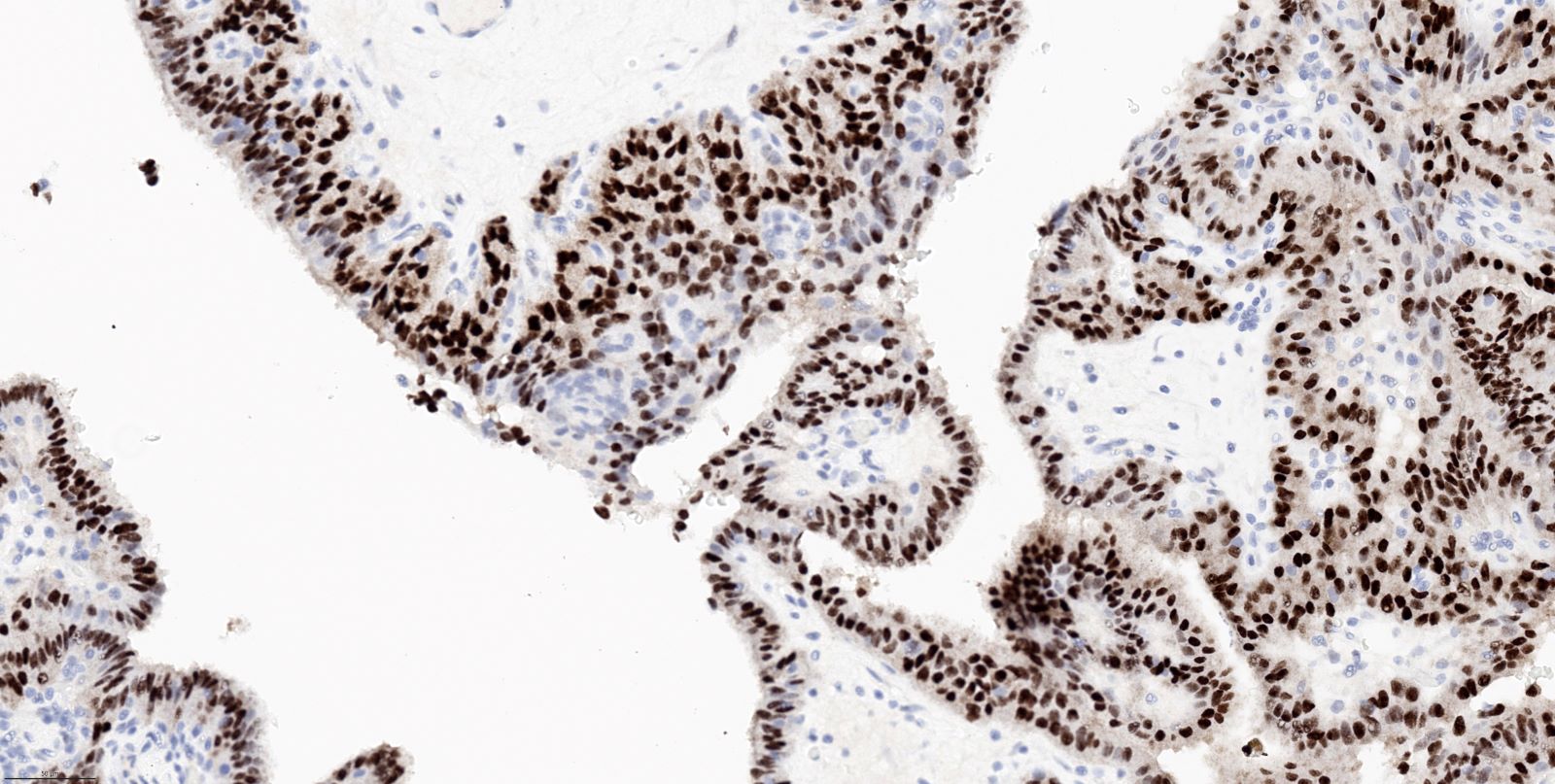
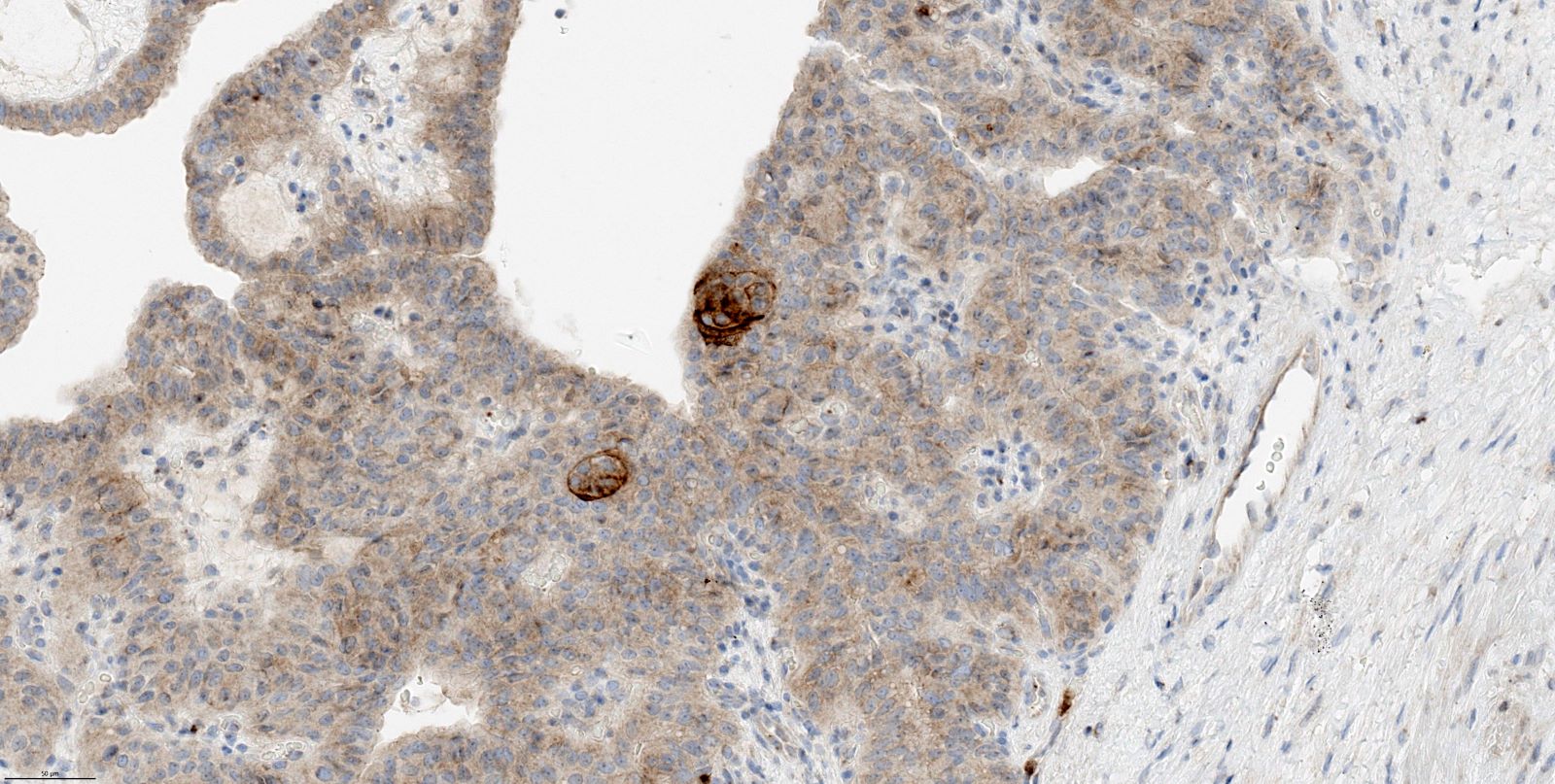
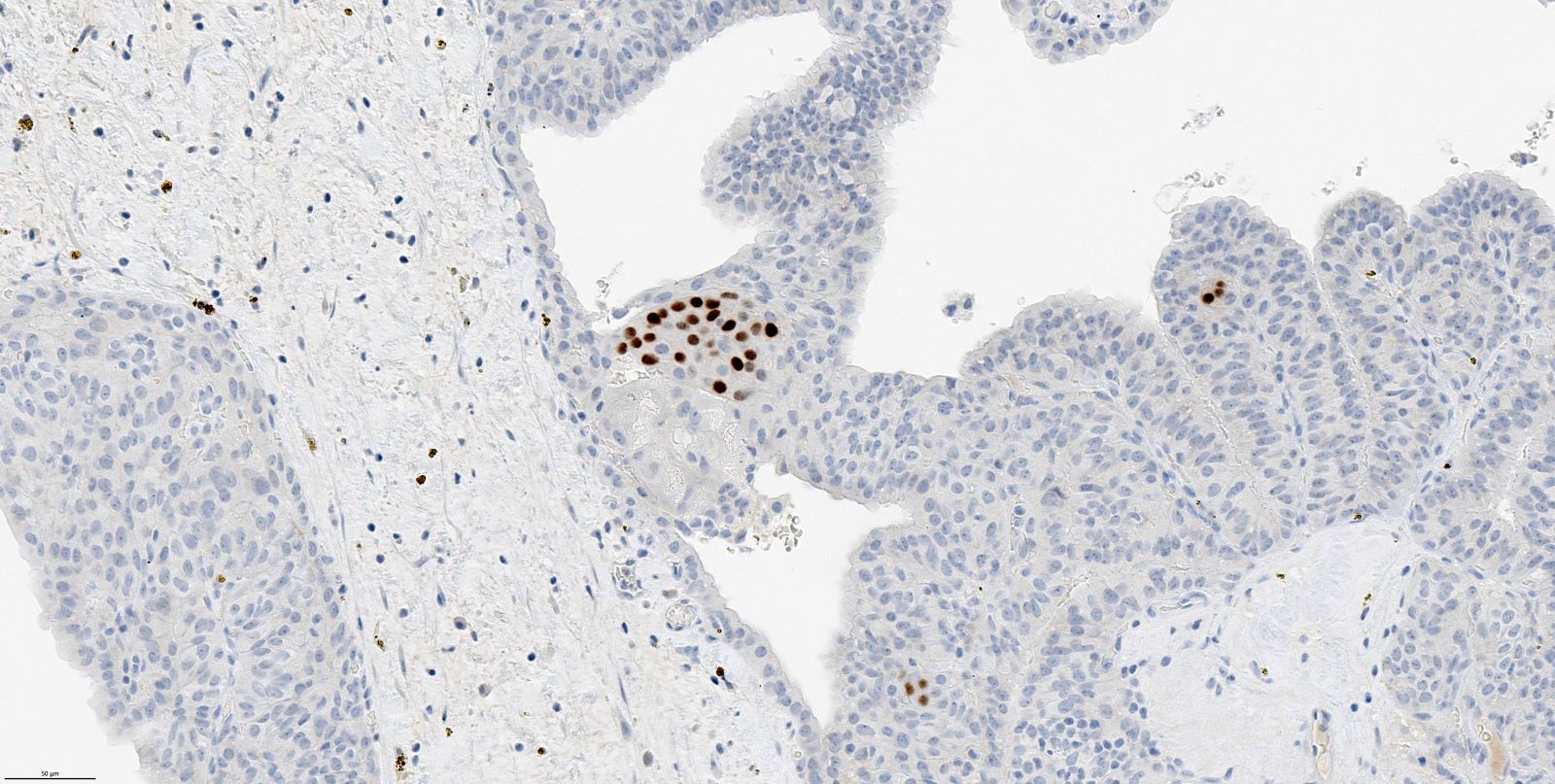
Histopathology images:
What is your diagnosis?
Diagnosis: Cribriform morular thyroid carcinoma (formerly known as cribriform morular variant of papillary thyroid carcinoma), high grade
Test question (answer at the end):
Which of the following statements about cribriform morular thyroid carcinoma is true?
A. It is a subtype (variant) of papillary thyroid carcinoma
B. It does not occur in a familial setting
C. No distinct mutations are commonly identified
D. It typically is negative for thyroglobulin and PAX8
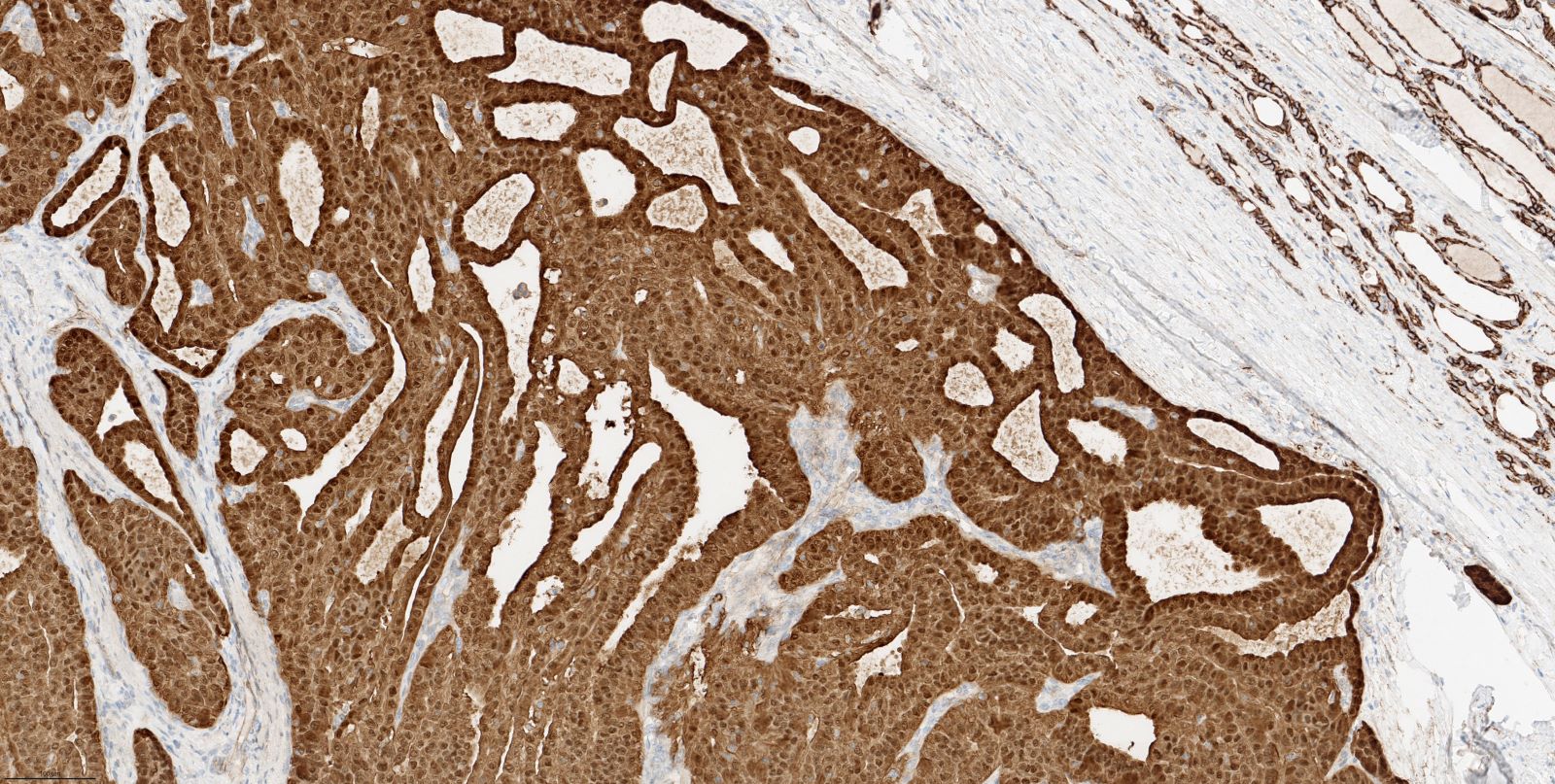
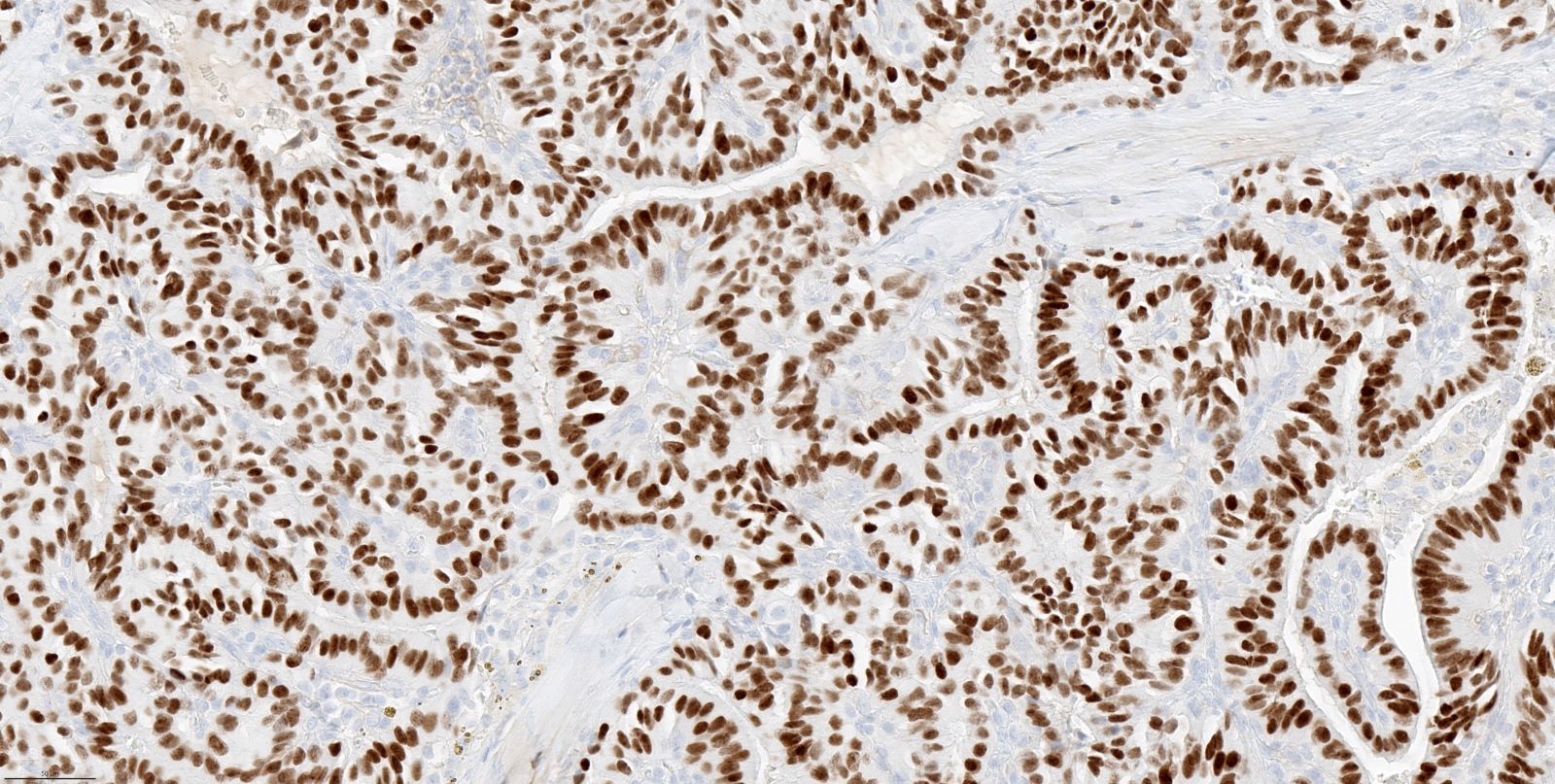
Stains:
Discussion:
Cribriform morular thyroid carcinoma was formerly classified as papillary thyroid carcinoma, cribriform morular variant (WHO 4th edition). In the WHO 5th edition (Endocr Relat Cancer 2022;30:e220293, Endocr Pathol 2022;33:27), this carcinoma becomes a separate entity under the umbrella of thyroid tumors of uncertain histogenesis. The rationale for this change is threefold: 1) the tumors are often negative for thyroglobulin and PAX8, arguing against thyroid follicular cell origin; 2) the morular component is typically positive for CD5, CK5, CD10 and CDX2, whereas negative for p40, TTF1 and PAX8, which is postulated to be of divergent thymic / ultimobranchial pouch differentiation (Endocr Pathol 2021;32:327); and 3) this tumor characteristically harbors aberrant genetic alterations of the Wnt pathway, which is different from the common alterations of MAPK pathway observed in thyroid follicular cell derived neoplasms.
Clinical features: the majority (~90%) of cribriform morular thyroid carcinoma occurs in young women < 40 years old.
Histological features of cribriform morular thyroid carcinoma
Immunohistochemistry profile
Molecular profile
Test question answer:
D. It typically is negative for thyroglobulin and PAX8. Answer A is incorrect because the tumors are no longer considered a variant of papillary thyroid carcinoma. Answer B is incorrect because they may be familial. Answer C is incorrect because up to 53% of cases occur in the setting of germline APC mutation (familial adenomatous polyposis) and sporadic cases often harbor molecular alterations of the WNT / beta catenin pathway.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Bin Xu, Memorial Sloan Kettering Cancer Center, New York, New York, USA for contributing this case and discussion and to Dr. Marc Pusztaszeri, McGill University, Montreal, Quebec, Canada for reviewing the discussion.

Advertisement
Case of the Month #528
Clinical history:
A 19 year old woman presented with a 3.7 cm thyroid mass.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Cribriform morular thyroid carcinoma (formerly known as cribriform morular variant of papillary thyroid carcinoma), high grade
Test question (answer at the end):
Which of the following statements about cribriform morular thyroid carcinoma is true?
A. It is a subtype (variant) of papillary thyroid carcinoma
B. It does not occur in a familial setting
C. No distinct mutations are commonly identified
D. It typically is negative for thyroglobulin and PAX8
Stains:
Discussion:
Cribriform morular thyroid carcinoma was formerly classified as papillary thyroid carcinoma, cribriform morular variant (WHO 4th edition). In the WHO 5th edition (Endocr Relat Cancer 2022;30:e220293, Endocr Pathol 2022;33:27), this carcinoma becomes a separate entity under the umbrella of thyroid tumors of uncertain histogenesis. The rationale for this change is threefold: 1) the tumors are often negative for thyroglobulin and PAX8, arguing against thyroid follicular cell origin; 2) the morular component is typically positive for CD5, CK5, CD10 and CDX2, whereas negative for p40, TTF1 and PAX8, which is postulated to be of divergent thymic / ultimobranchial pouch differentiation (Endocr Pathol 2021;32:327); and 3) this tumor characteristically harbors aberrant genetic alterations of the Wnt pathway, which is different from the common alterations of MAPK pathway observed in thyroid follicular cell derived neoplasms.
Clinical features: the majority (~90%) of cribriform morular thyroid carcinoma occurs in young women < 40 years old.
Histological features of cribriform morular thyroid carcinoma
- Commonly circumscribed or encapsulated.
- Variable architecture patterns, including cribriform, follicular, papillary and solid / insular / trabecular pattern. The cribriform pattern may not be seen in all cases.
- Nuclear features of papillary thyroid carcinoma are not pronounced; in the papillary area, the lining cells are usually columnar or elongated.
- Squamoid morula ranges from sparse to abundant. They are composed of morula or whirls of spindle to ovoid cells. True keratinization is absent.
- High grade tumors are characterized by increased mitotic activity or necrosis; these cases were reported as case reports and were associated with adverse outcome (Pathol Int 2018;68:700).
Immunohistochemistry profile
- Diffuse aberrant nuclear beta catenin expression is essential for the diagnosis of this tumor.
- The squamoid morula: positive for CD5, CK5, CD10 and CDX2, whereas negative for p40, ER, PR, TTF1 and PAX8.
- Background tumor: positive for estrogen receptor (ER), progesterone receptor (PR) and TTF1 (variable). Thyroglobulin is usually negative.
Molecular profile
- A proportion (up to 53%) of cribriform morular thyroid carcinoma occurs in the setting of germline APC mutation (familial adenomatous polyposis).
- Sporadic cases often harbor molecular alterations of WNT / beta catenin pathway.
Test question answer:
D. It typically is negative for thyroglobulin and PAX8. Answer A is incorrect because the tumors are no longer considered a variant of papillary thyroid carcinoma. Answer B is incorrect because they may be familial. Answer C is incorrect because up to 53% of cases occur in the setting of germline APC mutation (familial adenomatous polyposis) and sporadic cases often harbor molecular alterations of the WNT / beta catenin pathway.