18 May 2023 - Case of the Month #527
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Raul Gonzalez, Emory University School of Medicine, Atlanta, Georgia, USA for contributing this case and discussion and to Dr. Naziheh Assarzadegan, University of Florida, Gainesville, Florida, USA for reviewing the discussion.
Case of the Month #527
Clinical history:
A 45 year old man presents to a gastroenterologist complaining of constipation and rectal bleeding. A single ulcerated rectal lesion is found on colonoscopy and is biopsied.
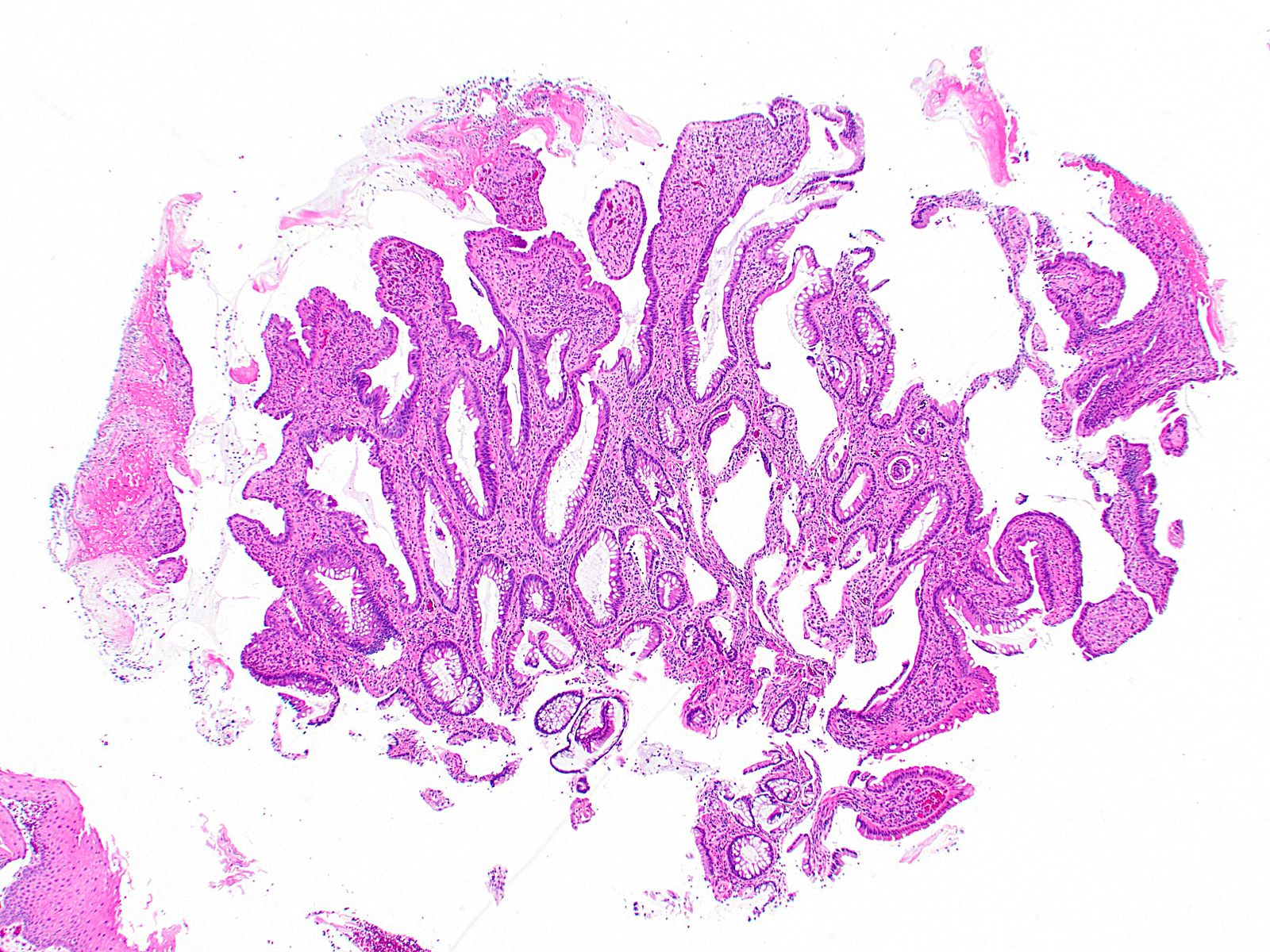
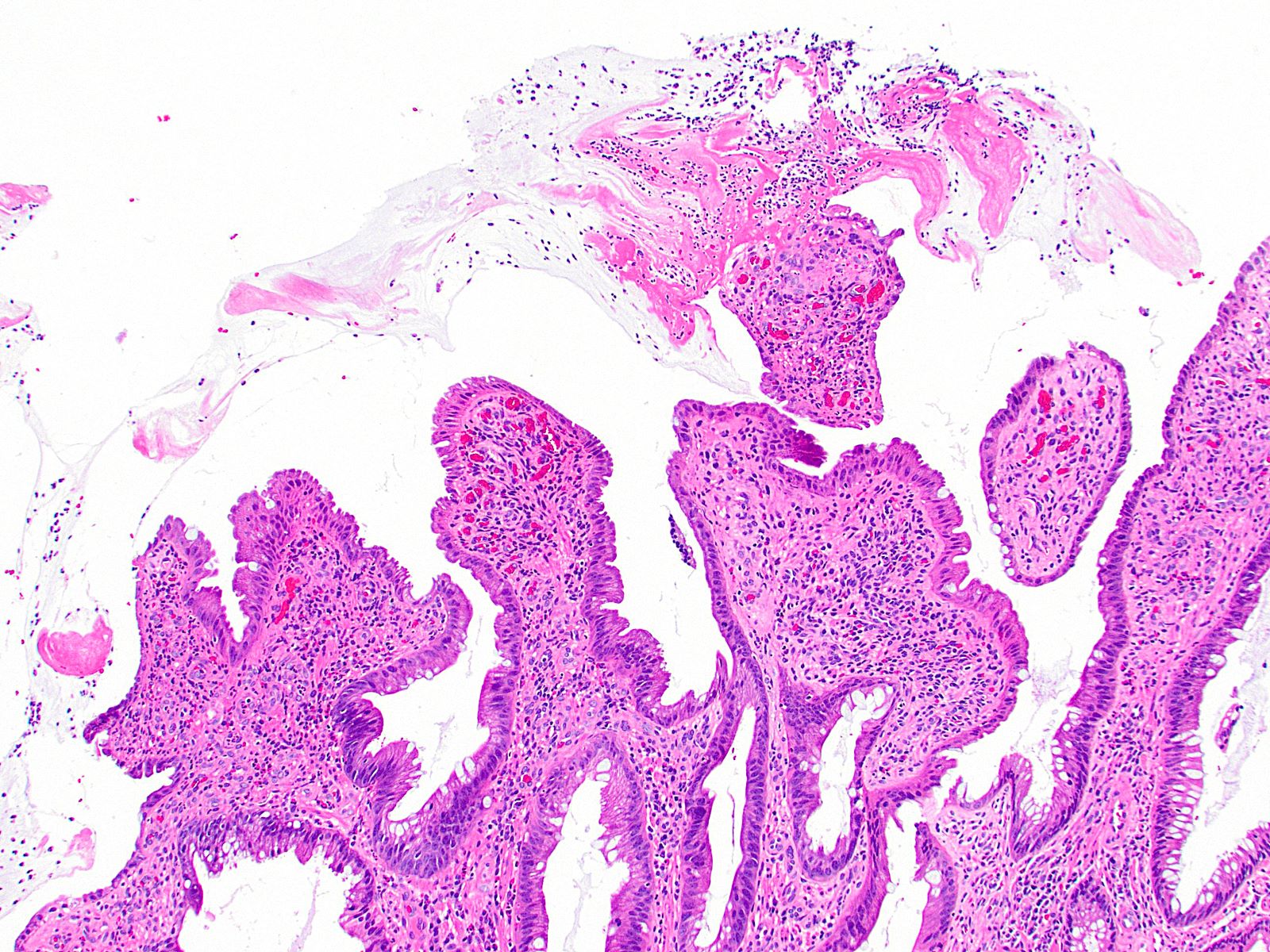
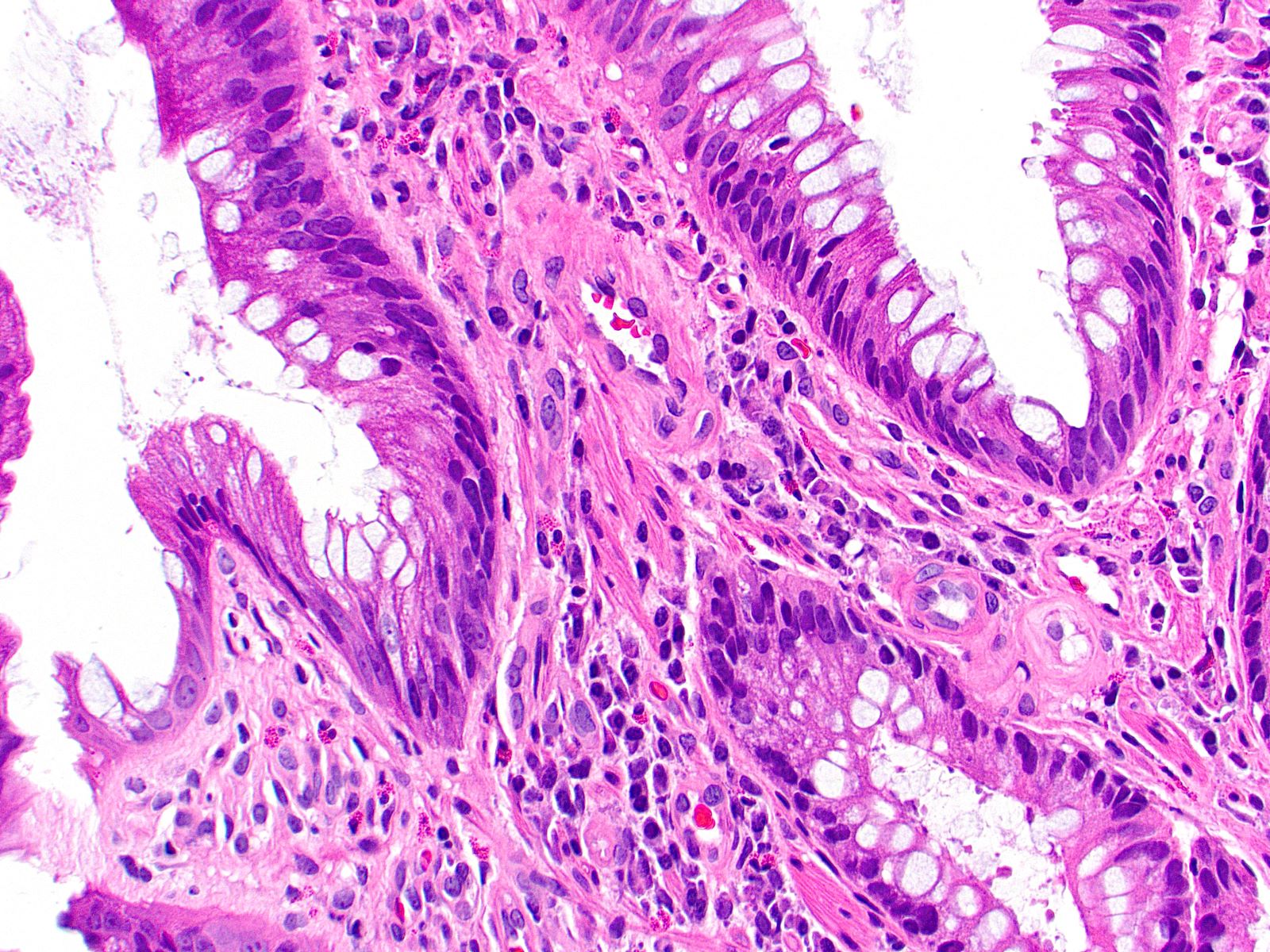
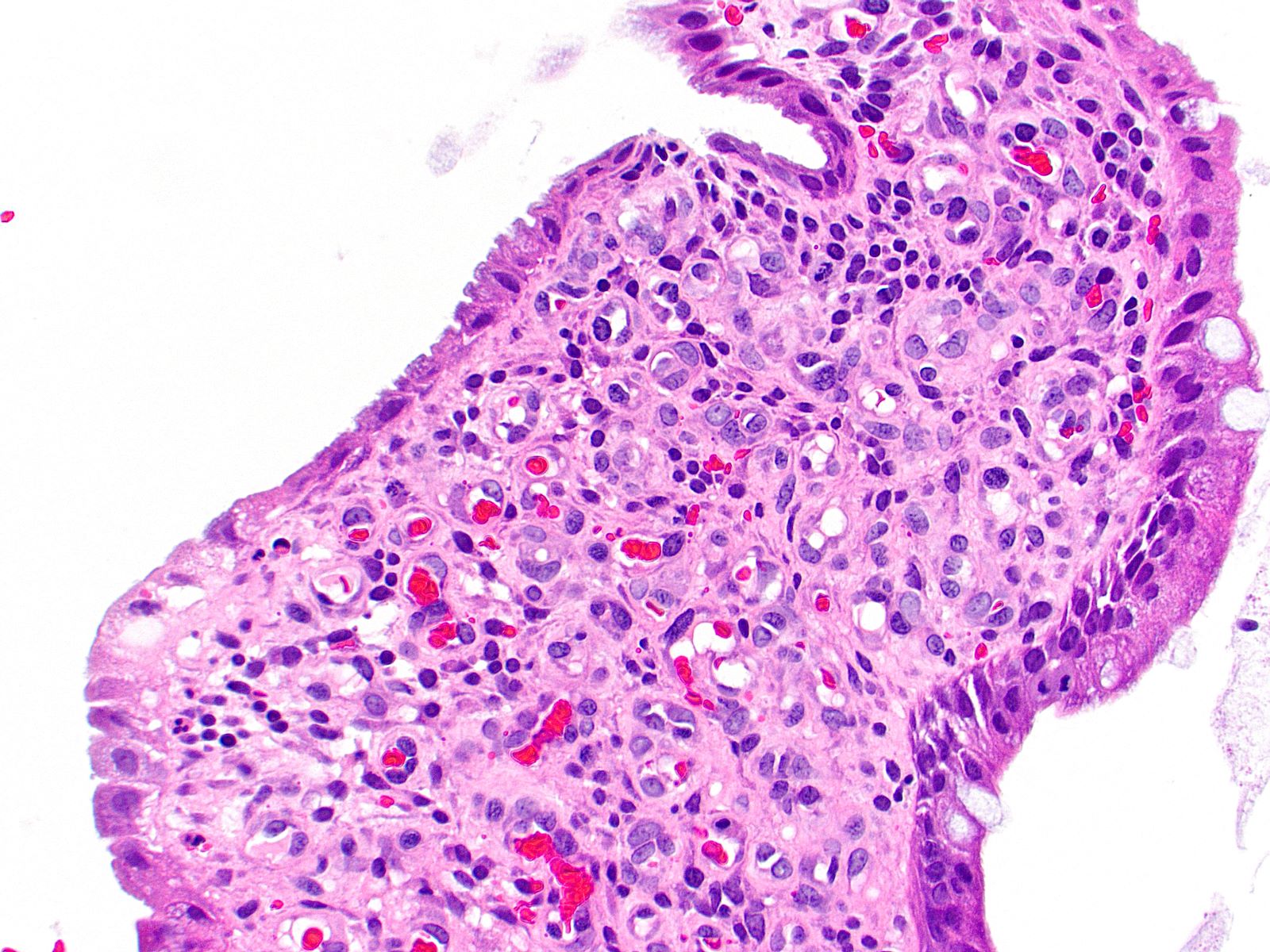
Histopathology images:
What is your diagnosis?
Diagnosis: Solitary rectal ulcer syndrome
Test question (answer at the end):
Which of the following is true about solitary rectal ulcer syndrome?
A. Patients demonstrate typical associated systemic symptoms
B. Prolapse of intestinal mucosa is specific to this disease entity
C. Roughly 30% of patients have multiple lesions
D. The diagnosis cannot be made without microscopic ulceration
Discussion:
Solitary rectal ulcer syndrome is the name given to the uncommon finding of locally prolapsed mucosa in the anterior rectum, which can lead to ulceration. Patients are most often in the fourth or fifth decade of life; pediatric involvement was originally considered uncommon but is increasingly being reported (J Pediatr Gastroenterol Nutr 2020;71:29). It is generally believed that the process occurs in patients who strain during defecation and many also have pelvic floor disorders (World J Gastroenterol 2014;20:738). While the finding is often solitary / unifocal, ~30% of patients are reported to have multiple lesions (BMC Gastroenterol 2012;12:72). Additionally, calling the process a "syndrome" is somewhat tenuous; patients often have a history of constipation and can experience rectal bleeding and pain upon defecation but do not experience other local or systemic symptoms. The mainstay of treatment is patient education and change in diet, though resection may be necessary in some cases (World J Gastroenterol 2014;20:738).
Histologically, solitary rectal ulcer syndrome generally displays prolapse type features, including vertical wisps of smooth muscle in the lamina propria and reactive, diamond shaped colonic crypts. Ulceration with associated inflammation may be present but is not always seen and is not a mandatory finding (BMC Gastroenterol 2012;12:72). Other potential findings include reactive epithelial changes, villiform arrangement of the superficial mucosa, vascular dilation / congestion and subepithelial collagen thickening. Similar changes can occur elsewhere in the gastrointestinal tract where prolapse occurs, such as in distal colonic prolapse type polyps and in the mucosa overlying diverticular disease.
Test question answer:
C. Roughly 30% of patients have multiple lesions. Despite the name, "solitary rectal ulcer syndrome" is not always a solitary finding. Approximately 30% of patients will demonstrate multiple rectal ulcers on colonoscopy. Answer A is incorrect because solitary rectal ulcer syndrome is not a systemic syndrome, meaning patients will not have associated systemic symptoms. Answer B is incorrect because prolapse of intestinal mucosa can be seen histologically in other diseases, such as diverticulosis. Answer D is incorrect because microscopic ulceration is often but not always encountered, meaning it is not required to establish the diagnosis.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Raul Gonzalez, Emory University School of Medicine, Atlanta, Georgia, USA for contributing this case and discussion and to Dr. Naziheh Assarzadegan, University of Florida, Gainesville, Florida, USA for reviewing the discussion.
Case of the Month #527
Clinical history:
A 45 year old man presents to a gastroenterologist complaining of constipation and rectal bleeding. A single ulcerated rectal lesion is found on colonoscopy and is biopsied.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Solitary rectal ulcer syndrome
Test question (answer at the end):
Which of the following is true about solitary rectal ulcer syndrome?
A. Patients demonstrate typical associated systemic symptoms
B. Prolapse of intestinal mucosa is specific to this disease entity
C. Roughly 30% of patients have multiple lesions
D. The diagnosis cannot be made without microscopic ulceration
Discussion:
Solitary rectal ulcer syndrome is the name given to the uncommon finding of locally prolapsed mucosa in the anterior rectum, which can lead to ulceration. Patients are most often in the fourth or fifth decade of life; pediatric involvement was originally considered uncommon but is increasingly being reported (J Pediatr Gastroenterol Nutr 2020;71:29). It is generally believed that the process occurs in patients who strain during defecation and many also have pelvic floor disorders (World J Gastroenterol 2014;20:738). While the finding is often solitary / unifocal, ~30% of patients are reported to have multiple lesions (BMC Gastroenterol 2012;12:72). Additionally, calling the process a "syndrome" is somewhat tenuous; patients often have a history of constipation and can experience rectal bleeding and pain upon defecation but do not experience other local or systemic symptoms. The mainstay of treatment is patient education and change in diet, though resection may be necessary in some cases (World J Gastroenterol 2014;20:738).
Histologically, solitary rectal ulcer syndrome generally displays prolapse type features, including vertical wisps of smooth muscle in the lamina propria and reactive, diamond shaped colonic crypts. Ulceration with associated inflammation may be present but is not always seen and is not a mandatory finding (BMC Gastroenterol 2012;12:72). Other potential findings include reactive epithelial changes, villiform arrangement of the superficial mucosa, vascular dilation / congestion and subepithelial collagen thickening. Similar changes can occur elsewhere in the gastrointestinal tract where prolapse occurs, such as in distal colonic prolapse type polyps and in the mucosa overlying diverticular disease.
Test question answer:
C. Roughly 30% of patients have multiple lesions. Despite the name, "solitary rectal ulcer syndrome" is not always a solitary finding. Approximately 30% of patients will demonstrate multiple rectal ulcers on colonoscopy. Answer A is incorrect because solitary rectal ulcer syndrome is not a systemic syndrome, meaning patients will not have associated systemic symptoms. Answer B is incorrect because prolapse of intestinal mucosa can be seen histologically in other diseases, such as diverticulosis. Answer D is incorrect because microscopic ulceration is often but not always encountered, meaning it is not required to establish the diagnosis.