12 October 2022 - Case of the Month #520
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Debra Zynger, Ohio State University, Columbus, Ohio, USA, for contributing this case and discussion and to Dr. Bonnie Choy, Northwestern University, Chicago, Illinois, USA, for reviewing the discussion.

Case of the Month #520
Clinical history:
A 61 year old man with a flaky rash in the penoscrotal region for 9 month with no cancer history had negative CT scans of the abdomen and pelvis. He underwent a scrotal excision and partial penectomy.
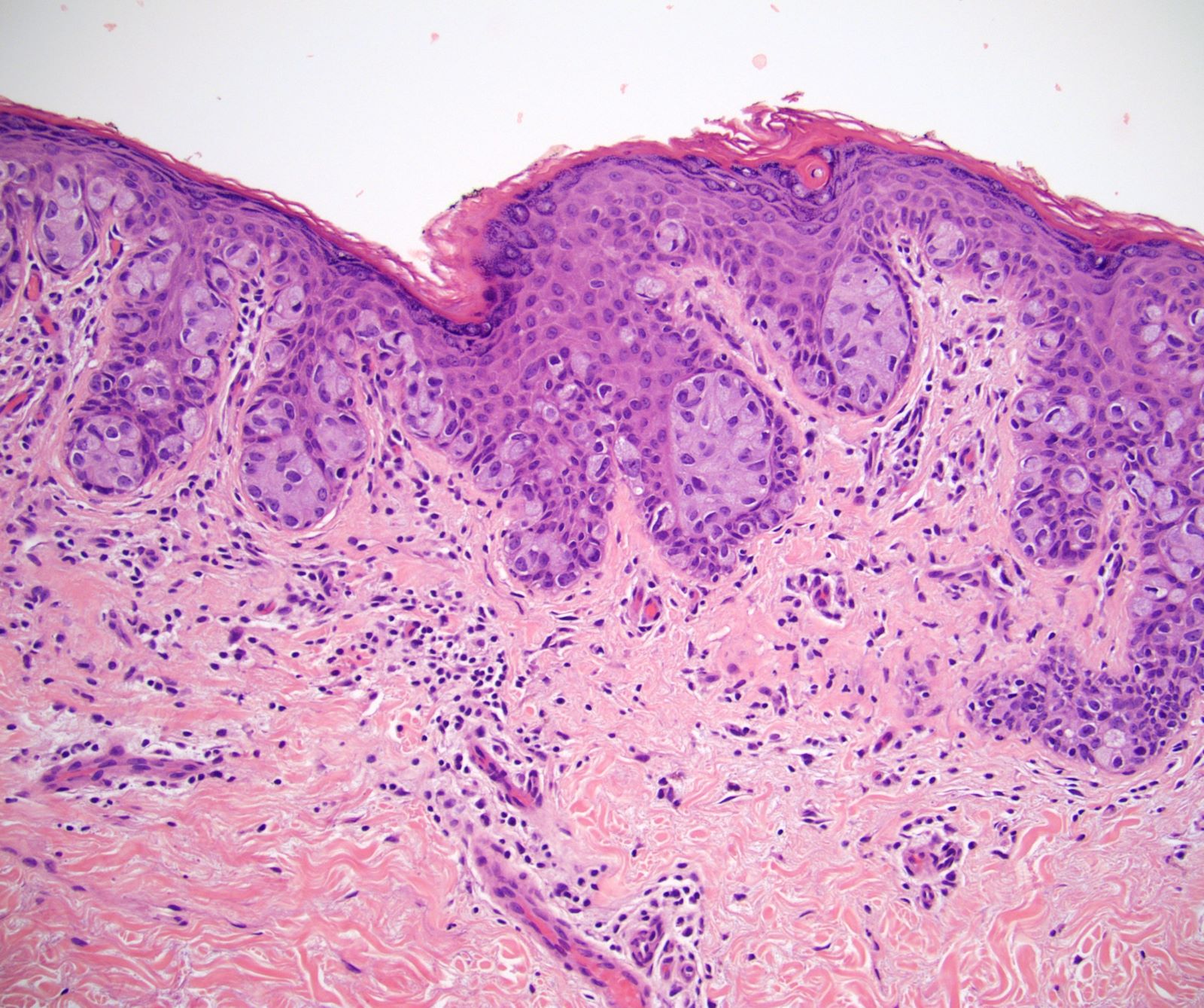
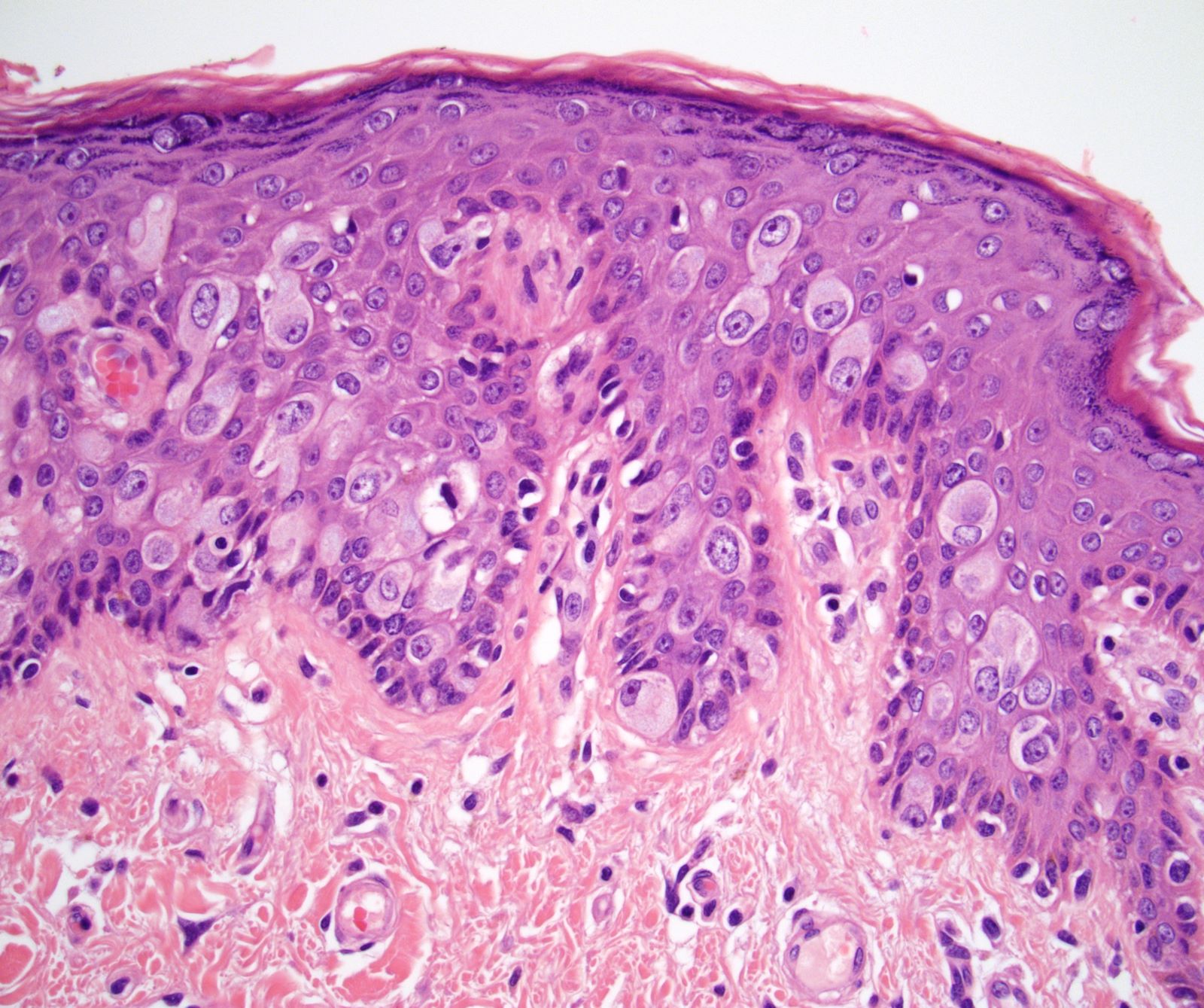
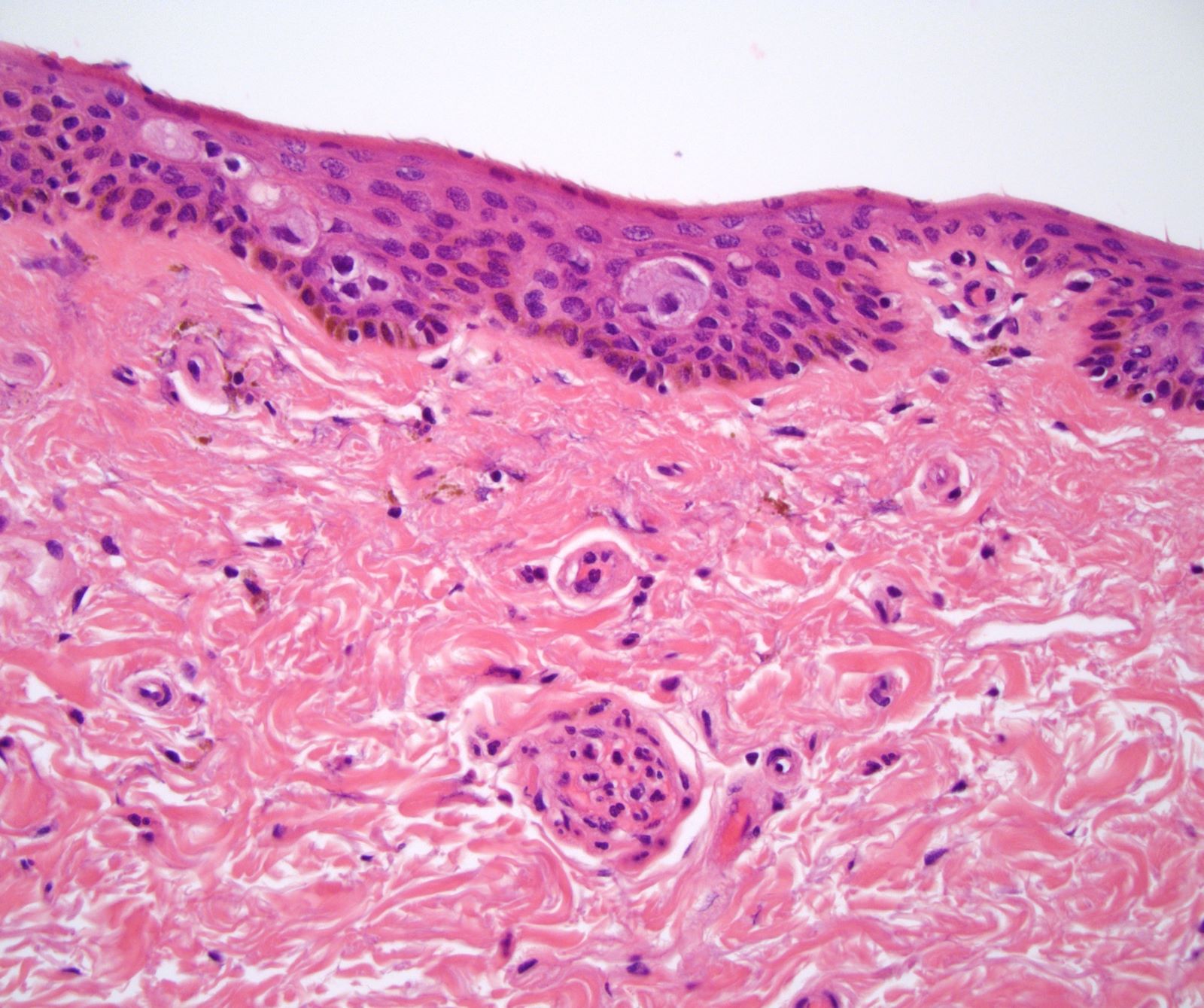
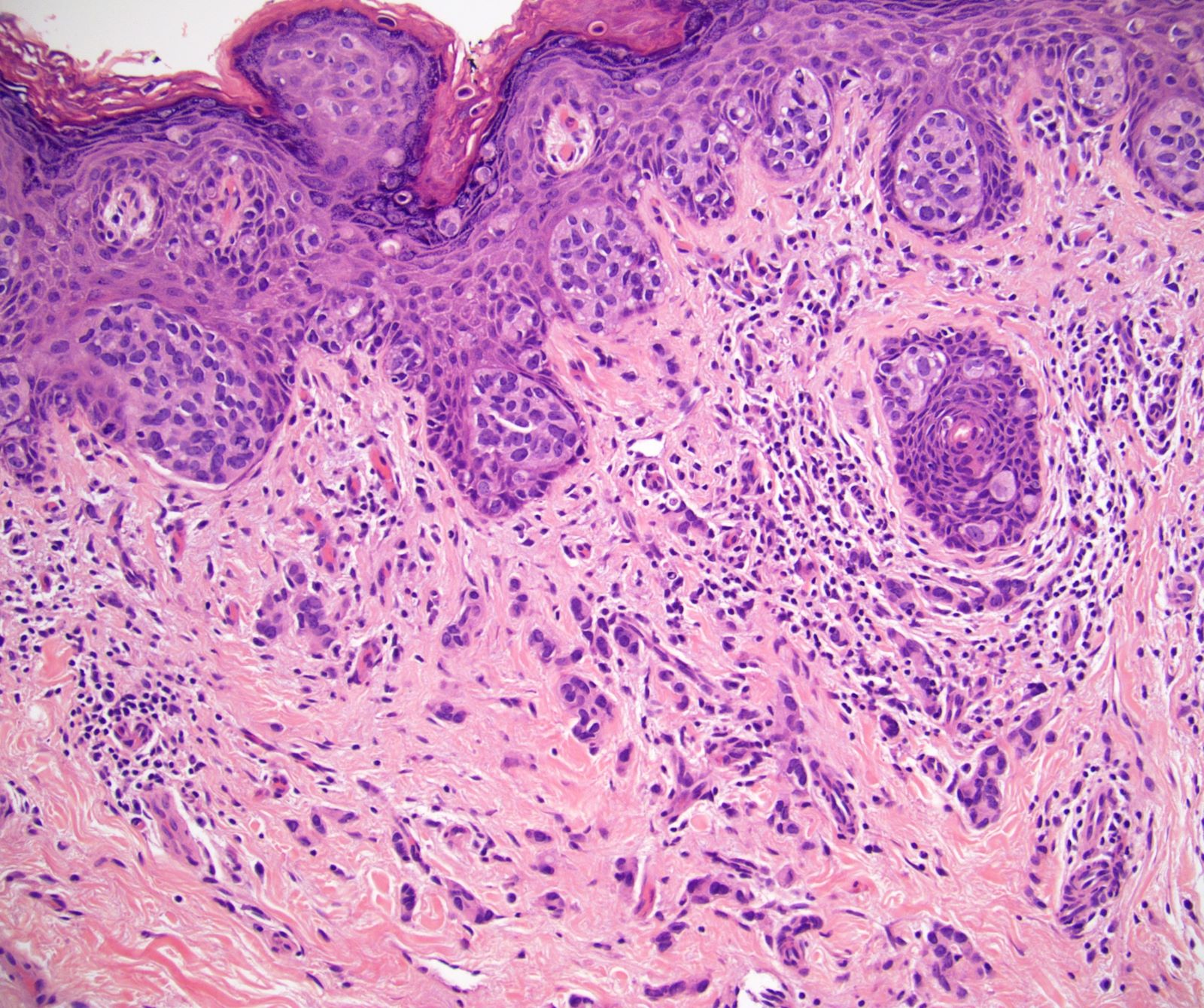
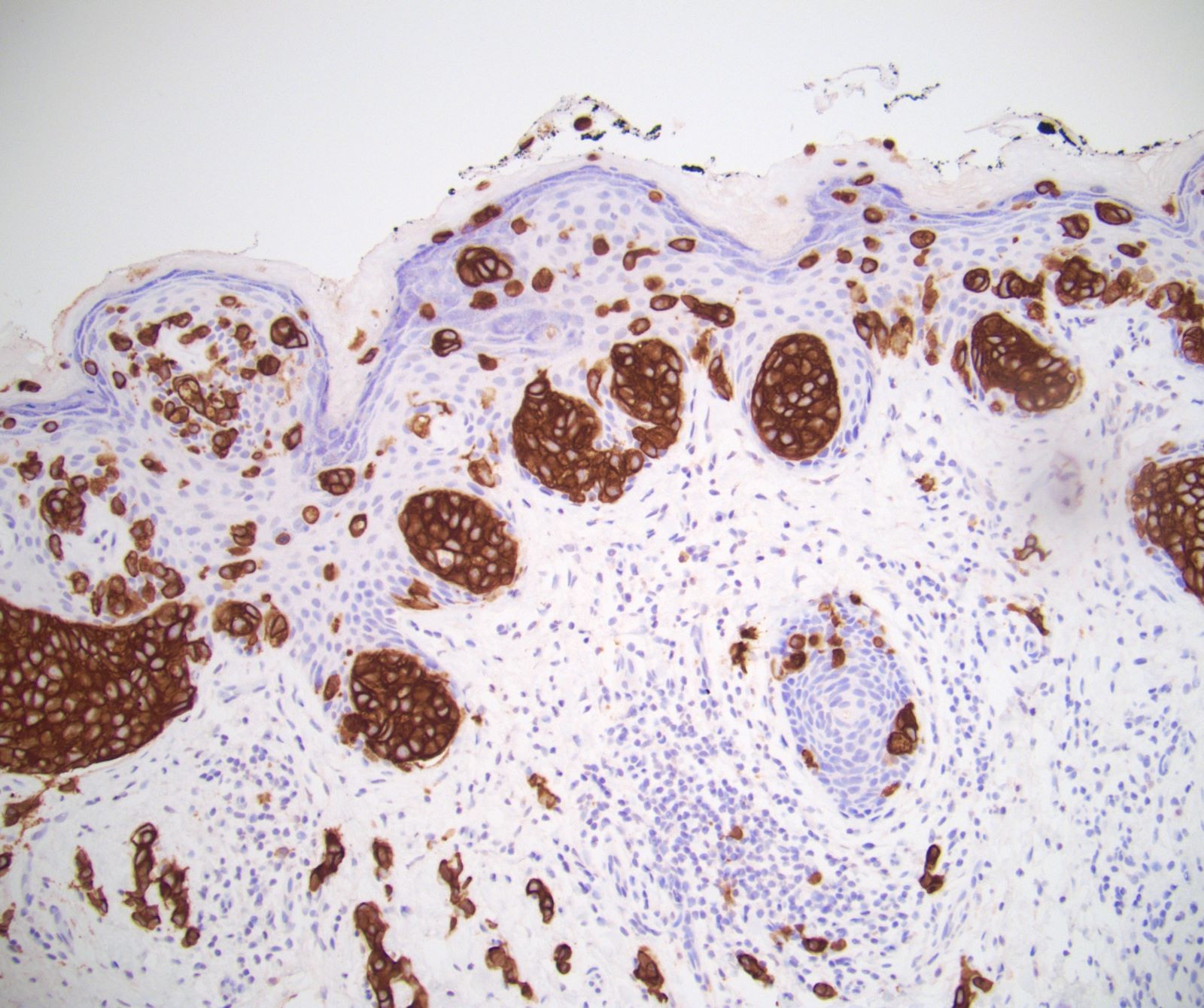
Histopathology images:
What is your diagnosis?
Diagnosis: Extramammary Paget disease with microinvasion
Test questions (answer at the end):
Which immunoprofile is compatible with primary penoscrotal extramammary Paget disease?
A. CDX2+, CK20+
B. CK7+, GATA3+
C. PSA+, NKX3.1+
D. S100+, melanA+
Stains
Discussion:
Paget disease of the penis and scrotum is a rare, intraepidermal adenocarcinoma that arises as a primary tumor or from secondary involvement of a nonpenoscrotal neoplasm from urogenital, colorectal or cutaneous origin sites (Dis Colon Rectum 2019;62:1283). It is found in older men with a median age of 65 - 72 years. Lesions present with pruritus, erythema, pain, rash, erosion and exudation. Often a large area of skin is involved (median size 20.5 cm2) (Indian J Dermatol Venereol Leprol 2020;86:134). Paget disease is frequently misdiagnosed as a nonneoplastic lesion with a median delay between initial symptoms and correct diagnosis of 3 - 4 years (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70, Urol Oncol 2010;28:28, BJU Int 2008;102:485, BJU Int 2015;115:153). Treatment is by wide local excision or Mohs micrographic surgery. Intraoperative frozen section can be used to assess margins for local wide excision but interpretation is difficult with a false negative rate of up to 40% (J Med Case Rep 2009;3:4, J Plast Reconstr Aesthet Surg 2020;73:1700, BJU Int 2007;100:1282, Urol Oncol 2009;27:483).
Microscopically, there are single and clusters of atypical intraepidermal epithelial cells. Aggregates form in the basal layers of epidermis with underlying flattened basal keratinocytes. Cells are large and round with abundant, pale eosinophilic cytoplasm, large nuclei and prominent nucleoli.10 - 20% have dermal invasion with dermal tumor seen as individual cells or forming nodules, glands or sheets, as is present in this case (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70). Deeper invasion may portend a worse prognosis (Hum Pathol 2016;47:70). Hyperkeratosis, parakeratosis and dense chronic inflammation are often present. Intracytoplasmic melanin pigment can be seen, mimicking melanoma. Lymphovascular invasion and perineural invasion are uncommon (Hum Pathol 2016;47:70).
The differential diagnosis includes secondary involvement by spread or metastases, which can be excluded based on IHC and clinical history. Primary Paget's disease expresses pankeratins (AE1/AE3, CAM5.2, LMWK), EMA, CK7, CEA, GATA3 and Androgen Receptor, has variable expression of GCDFP-15 and HER2, and is negative for p63, CK5/6, S100, HMB45, CK20, CDX2, NKX3.1, PSA and prostein (Dermatol Online J 2019;25:13030, Indian J Dermatol Venereol Leprol 2020;86:134, Hum Pathol 2016;47:70, Int J Surg Pathol 2018;26:617, Hum Pathol 2018;77:152, Appl Immunohistochem Mol Morphol 2020;28:524). The most relevant secondary sites to consider are urothelial carcinoma (p63+), prostatic adenocarcinoma (PSA+, NKX3.1+) and colorectal adenocarcinoma (CK20+, CDX2+). The differential diagnosis for other primary tumors includes melanoma in situ, which does not have a keratinocyte layer in between the tumor cells and dermis, expresses melanocytic markers (S100, HMB45, MelanA) and is negative for AE1/AE3 and CK7. Squamous cell carcinoma in situ / penile intraepithelial neoplasia (PeIN) has full thickness involvement by eosinophilic tumor cells expresses p63.
Survival for extramammary Paget disease of the penoscrotum is ~70% at the 3 - 5 year mark (Dis Colon Rectum 2019;62:1283, Hum Pathol 2016;47:70, Sci Rep 2017;7:44933, BJU Int 2015;115:153). This patient has had no evidence of disease for the past 3 years.
Test question answers:
B. CK7+, GATA3+
Primary penoscrotal extramammary Paget disease tumoral cells express AE1 / AE3, CK7, GATA3 and CEA. Colorectal adenocarcinoma is positive for CDX2 and CK20. Prostatic adenocarcinoma is positive for PSA and NKX3.1. Melanoma is positive for S100 and melanA.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Debra Zynger, Ohio State University, Columbus, Ohio, USA, for contributing this case and discussion and to Dr. Bonnie Choy, Northwestern University, Chicago, Illinois, USA, for reviewing the discussion.

Case of the Month #520
Clinical history:
A 61 year old man with a flaky rash in the penoscrotal region for 9 month with no cancer history had negative CT scans of the abdomen and pelvis. He underwent a scrotal excision and partial penectomy.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Extramammary Paget disease with microinvasion
Test questions (answer at the end):
Which immunoprofile is compatible with primary penoscrotal extramammary Paget disease?
A. CDX2+, CK20+
B. CK7+, GATA3+
C. PSA+, NKX3.1+
D. S100+, melanA+
Stains
Discussion:
Paget disease of the penis and scrotum is a rare, intraepidermal adenocarcinoma that arises as a primary tumor or from secondary involvement of a nonpenoscrotal neoplasm from urogenital, colorectal or cutaneous origin sites (Dis Colon Rectum 2019;62:1283). It is found in older men with a median age of 65 - 72 years. Lesions present with pruritus, erythema, pain, rash, erosion and exudation. Often a large area of skin is involved (median size 20.5 cm2) (Indian J Dermatol Venereol Leprol 2020;86:134). Paget disease is frequently misdiagnosed as a nonneoplastic lesion with a median delay between initial symptoms and correct diagnosis of 3 - 4 years (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70, Urol Oncol 2010;28:28, BJU Int 2008;102:485, BJU Int 2015;115:153). Treatment is by wide local excision or Mohs micrographic surgery. Intraoperative frozen section can be used to assess margins for local wide excision but interpretation is difficult with a false negative rate of up to 40% (J Med Case Rep 2009;3:4, J Plast Reconstr Aesthet Surg 2020;73:1700, BJU Int 2007;100:1282, Urol Oncol 2009;27:483).
Microscopically, there are single and clusters of atypical intraepidermal epithelial cells. Aggregates form in the basal layers of epidermis with underlying flattened basal keratinocytes. Cells are large and round with abundant, pale eosinophilic cytoplasm, large nuclei and prominent nucleoli.10 - 20% have dermal invasion with dermal tumor seen as individual cells or forming nodules, glands or sheets, as is present in this case (Indian J Dermatol Venereol Leprol 2020;86:134, Sci Rep 2017;7:44933, Hum Pathol 2016;47:70). Deeper invasion may portend a worse prognosis (Hum Pathol 2016;47:70). Hyperkeratosis, parakeratosis and dense chronic inflammation are often present. Intracytoplasmic melanin pigment can be seen, mimicking melanoma. Lymphovascular invasion and perineural invasion are uncommon (Hum Pathol 2016;47:70).
The differential diagnosis includes secondary involvement by spread or metastases, which can be excluded based on IHC and clinical history. Primary Paget's disease expresses pankeratins (AE1/AE3, CAM5.2, LMWK), EMA, CK7, CEA, GATA3 and Androgen Receptor, has variable expression of GCDFP-15 and HER2, and is negative for p63, CK5/6, S100, HMB45, CK20, CDX2, NKX3.1, PSA and prostein (Dermatol Online J 2019;25:13030, Indian J Dermatol Venereol Leprol 2020;86:134, Hum Pathol 2016;47:70, Int J Surg Pathol 2018;26:617, Hum Pathol 2018;77:152, Appl Immunohistochem Mol Morphol 2020;28:524). The most relevant secondary sites to consider are urothelial carcinoma (p63+), prostatic adenocarcinoma (PSA+, NKX3.1+) and colorectal adenocarcinoma (CK20+, CDX2+). The differential diagnosis for other primary tumors includes melanoma in situ, which does not have a keratinocyte layer in between the tumor cells and dermis, expresses melanocytic markers (S100, HMB45, MelanA) and is negative for AE1/AE3 and CK7. Squamous cell carcinoma in situ / penile intraepithelial neoplasia (PeIN) has full thickness involvement by eosinophilic tumor cells expresses p63.
Survival for extramammary Paget disease of the penoscrotum is ~70% at the 3 - 5 year mark (Dis Colon Rectum 2019;62:1283, Hum Pathol 2016;47:70, Sci Rep 2017;7:44933, BJU Int 2015;115:153). This patient has had no evidence of disease for the past 3 years.
Test question answers:
B. CK7+, GATA3+
Primary penoscrotal extramammary Paget disease tumoral cells express AE1 / AE3, CK7, GATA3 and CEA. Colorectal adenocarcinoma is positive for CDX2 and CK20. Prostatic adenocarcinoma is positive for PSA and NKX3.1. Melanoma is positive for S100 and melanA.