18 May 2022 - Case of the Month #515
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Ayesha Farooq, Mayo Clinic, Rochester, Minnesota, USA and Dr. Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin, USA for contributing this case and discussion and to Dr. Gary Tozbikian, Ohio State University, Columbus, Ohio, USA for reviewing the discussion.

Create or update your Directory profile so Pathologists can learn about you and contact you if
needed. When you write a paper, apply for a job or fellowship position or give a talk, pathologists
will want to look you up - make it easy for them by completing and updating your profile.
Email Directory@PathologyOutlines.com with any questions.
Case of the Month #515
Clinical history:
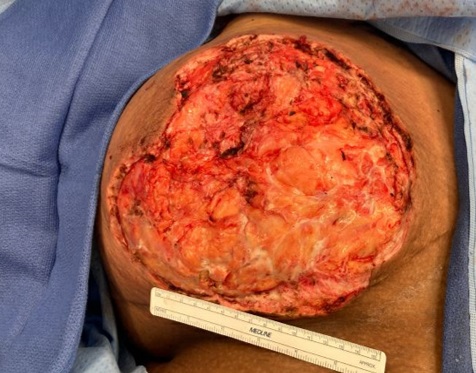
A young woman presented to the emergency department with right breast pain, erythema and drainage. She recently had her bilateral nipples pierced and developed a small sore near the border of her right nipple that progressed to an open wound. She developed fevers, chills and nausea. She had a prior history of breast reduction complicated by skin infection but no personal or family history of breast disease.
Clinical and histopathology images:
What is your diagnosis?
Diagnosis: Necrotizing bacterial infection with skin ulceration and abscess (cultures grew Streptococcus pyogenes, or group A Streptococcus)
Test question (answer at the end):
What is a common causative microorganism associated with nipple piercing related infection?
A. Salmonella
B. Shigella
C. Staphylococcus
D. Stenotrophomonas
Discussion:
The post nipple piercing infection rate is estimated to be 10 - 20% (Bland: The Breast, 5th Edition, 2018). Infection can be localized as an abscess or cellulitis. Complications such as endocarditis in high risk patients may occur.
Infections typically present in two peaks: patients may present acutely (days to weeks after procedure) or have delayed onset (months later). Acute infections are often due to poor hygiene at piercing or negligent post procedure care. Infections occurring months after piercing may be due to delayed healing, which predisposes patients to infection. Causative pathogens include Staphylococcus and Streptococcus species (from skin flora), Mycobacterium species, Neisseria gonorrhoeae, Prevotella intermedia, Pseudomonas and anaerobes.
For successful treatment, the ornament (nidus of infection) must be removed. While tissue Gram stain may highlight bacteria, cultures with sensitivities should be obtained to identify the causative pathogen and guide therapy. For breast abscess, incision and drainage is performed; however, for more severe infection, as in this case, aggressive surgical debridement of necrotic tissue is indicated (Dermatol Online J 2018;24:13030, IDCases 2019;18:e00620).
Test question answer:
C. Staphylococcus
Acknowledgment:
Thanks to Danielle Wilson, M.D. (Department of Surgery, Medical College of Wisconsin) for providing clinical images
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Ayesha Farooq, Mayo Clinic, Rochester, Minnesota, USA and Dr. Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin, USA for contributing this case and discussion and to Dr. Gary Tozbikian, Ohio State University, Columbus, Ohio, USA for reviewing the discussion.

Create or update your Directory profile so Pathologists can learn about you and contact you if
needed. When you write a paper, apply for a job or fellowship position or give a talk, pathologists
will want to look you up - make it easy for them by completing and updating your profile.
Email Directory@PathologyOutlines.com with any questions.
Case of the Month #515
Clinical history:
A young woman presented to the emergency department with right breast pain, erythema and drainage. She recently had her bilateral nipples pierced and developed a small sore near the border of her right nipple that progressed to an open wound. She developed fevers, chills and nausea. She had a prior history of breast reduction complicated by skin infection but no personal or family history of breast disease.
Clinical and histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Necrotizing bacterial infection with skin ulceration and abscess (cultures grew Streptococcus pyogenes, or group A Streptococcus)
Test question (answer at the end):
What is a common causative microorganism associated with nipple piercing related infection?
A. Salmonella
B. Shigella
C. Staphylococcus
D. Stenotrophomonas
Discussion:
The post nipple piercing infection rate is estimated to be 10 - 20% (Bland: The Breast, 5th Edition, 2018). Infection can be localized as an abscess or cellulitis. Complications such as endocarditis in high risk patients may occur.
Infections typically present in two peaks: patients may present acutely (days to weeks after procedure) or have delayed onset (months later). Acute infections are often due to poor hygiene at piercing or negligent post procedure care. Infections occurring months after piercing may be due to delayed healing, which predisposes patients to infection. Causative pathogens include Staphylococcus and Streptococcus species (from skin flora), Mycobacterium species, Neisseria gonorrhoeae, Prevotella intermedia, Pseudomonas and anaerobes.
For successful treatment, the ornament (nidus of infection) must be removed. While tissue Gram stain may highlight bacteria, cultures with sensitivities should be obtained to identify the causative pathogen and guide therapy. For breast abscess, incision and drainage is performed; however, for more severe infection, as in this case, aggressive surgical debridement of necrotic tissue is indicated (Dermatol Online J 2018;24:13030, IDCases 2019;18:e00620).
Test question answer:
C. Staphylococcus
Acknowledgment:
Thanks to Danielle Wilson, M.D. (Department of Surgery, Medical College of Wisconsin) for providing clinical images