21 October 2021 - Case of the Month #508
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Kristina Doytcheva and Jennifer A. Bennett, University of Chicago Medical Center, Chicago, Illinois (USA) for contributing this case and the discussion and to Dr. Blake Gilks, University of British Columbia, Vancouver, British Columbia (Canada), for reviewing the discussion.

Advertisement
Case of the Month #508
Clinical history:
The patient is a 32 year old G7P7007 woman with a history of symptomatic uterine fibroids who presented for a total abdominal hysterectomy and bilateral salpingectomy. CT of the upper abdomen and pelvis revealed an enlarged uterus, 17.1 cm in greatest dimension with hypervascular lesions likely representing fibroids.
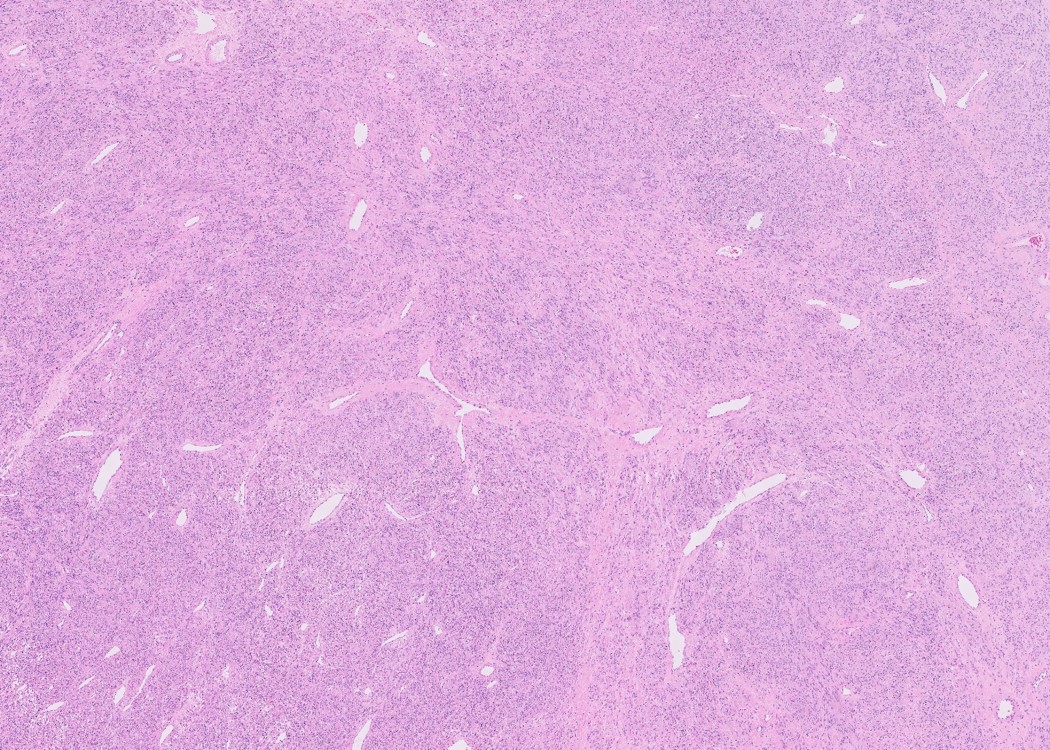
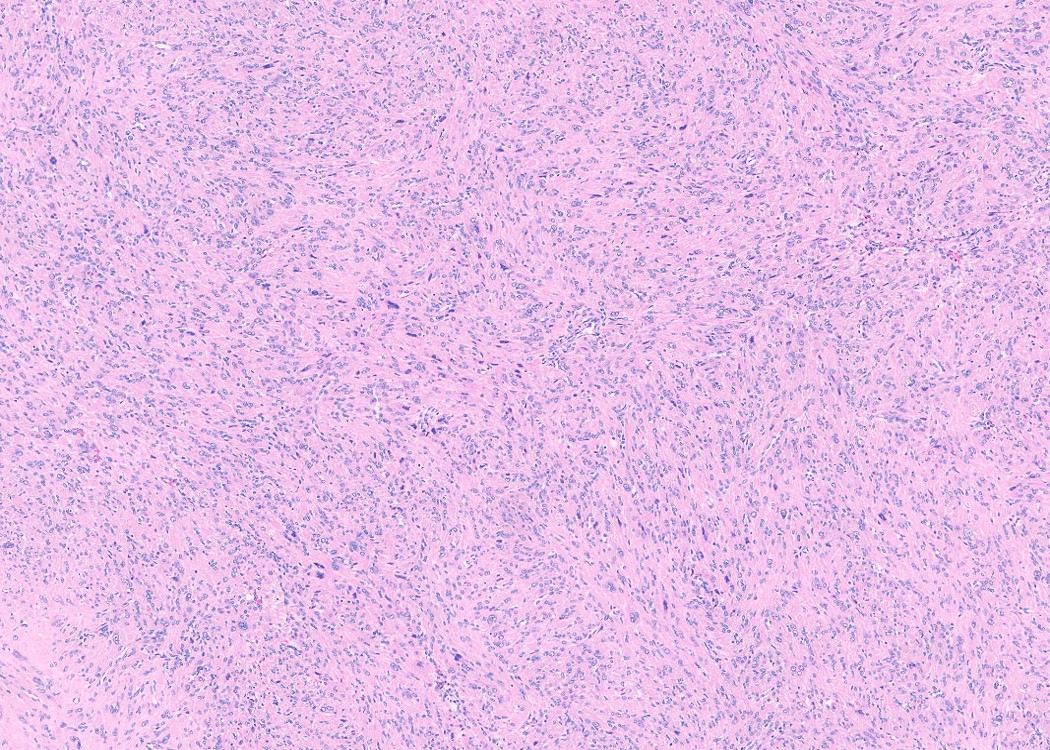
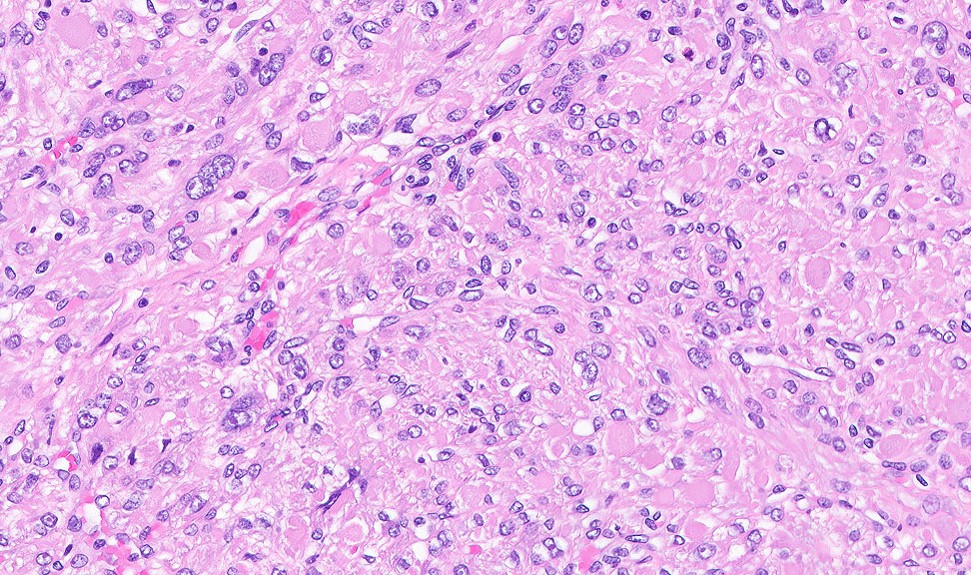
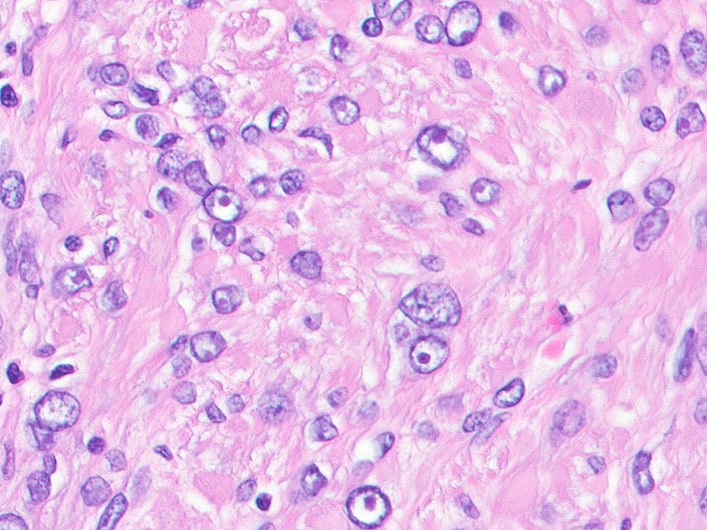
Histopathology images:
What is your diagnosis?
Diagnosis: Fumarate hydratase deficient (FH-d) leiomyoma
Test question (answer at the end):
What morphologic feature is suggestive of a FH-d leiomyoma?
A. > 10 mitoses per 10 high power fields
B. Myxoid stroma
C. Permeative (tongue-like) myometrial invasion
D. Prominent macronucleoli with perinucleolar halos
E. Tumor cell necrosis
Discussion:
Uterine leiomyomas are the most common tumor of the female reproductive tract. Fumarate hydratase deficient (FH-d) leiomyomas are characterized by staghorn blood vessels, an alveolar pattern of edema, eosinophilic cytoplasmic globules and prominent macronuclei with perinuclear halos (Am J Surg Pathol 2019;43:639, WHO Classification of Tumours Editorial Board: Female Genital Tumours, 5th Edition, 2020). Bizarre nuclei may be present. These tumors often show loss of FH staining by immunohistochemistry, however, a subset shows retained expression. Therefore, complete loss of FH is helpful in the diagnosis, while retained expression does not exclude the entity (Am J Surg Pathol 2019;43:1170).
FH is essential in the Krebs cycle, as it converts fumarate to malate. If either a somatic or germline FH mutation is present, fumarate accumulates in the cell and exerts downstream effects, such as succination of cysteine residues on proteins and activation of hypoxia inducible factor 1 (HIF-1) (Mod Pathol 2014;27:1020). It has been reported that up to 1.6% of all leiomyomas are of the FH-d variant (Am J Surg Pathol 2016;40:1661) and, if a germline mutation is present, the leiomyoma is a component of hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome. This is an autosomal dominant syndrome of patients predisposed to the development of cutaneous and uterine leiomyomas, as well as an aggressive form of renal cell carcinoma (Cancer Genet 2012;205:377). Uterine leiomyomas in these patients are diagnosed at a mean age of 28 years and most women undergo myomectomy or hysterectomy in their thirties and 15% develop aggressive renal cell carcinomas, usually diagnosed between 37 and 44 years (Am J Surg Pathol 2016;40:865). Therefore, being able to morphologically identify FH-d leiomyomas can triage a patient for genetic testing and appropriate management if needed.
The patient had germline genetic testing and was found to harbor a FH variant of uncertain clinical significance. She is currently undergoing annual renal ultrasounds.
Test question answer:
D. Prominent macronucleoli with perinucleolar halos
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Kristina Doytcheva and Jennifer A. Bennett, University of Chicago Medical Center, Chicago, Illinois (USA) for contributing this case and the discussion and to Dr. Blake Gilks, University of British Columbia, Vancouver, British Columbia (Canada), for reviewing the discussion.

Advertisement
Case of the Month #508
Clinical history:
The patient is a 32 year old G7P7007 woman with a history of symptomatic uterine fibroids who presented for a total abdominal hysterectomy and bilateral salpingectomy. CT of the upper abdomen and pelvis revealed an enlarged uterus, 17.1 cm in greatest dimension with hypervascular lesions likely representing fibroids.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Fumarate hydratase deficient (FH-d) leiomyoma
Test question (answer at the end):
What morphologic feature is suggestive of a FH-d leiomyoma?
A. > 10 mitoses per 10 high power fields
B. Myxoid stroma
C. Permeative (tongue-like) myometrial invasion
D. Prominent macronucleoli with perinucleolar halos
E. Tumor cell necrosis
Discussion:
Uterine leiomyomas are the most common tumor of the female reproductive tract. Fumarate hydratase deficient (FH-d) leiomyomas are characterized by staghorn blood vessels, an alveolar pattern of edema, eosinophilic cytoplasmic globules and prominent macronuclei with perinuclear halos (Am J Surg Pathol 2019;43:639, WHO Classification of Tumours Editorial Board: Female Genital Tumours, 5th Edition, 2020). Bizarre nuclei may be present. These tumors often show loss of FH staining by immunohistochemistry, however, a subset shows retained expression. Therefore, complete loss of FH is helpful in the diagnosis, while retained expression does not exclude the entity (Am J Surg Pathol 2019;43:1170).
FH is essential in the Krebs cycle, as it converts fumarate to malate. If either a somatic or germline FH mutation is present, fumarate accumulates in the cell and exerts downstream effects, such as succination of cysteine residues on proteins and activation of hypoxia inducible factor 1 (HIF-1) (Mod Pathol 2014;27:1020). It has been reported that up to 1.6% of all leiomyomas are of the FH-d variant (Am J Surg Pathol 2016;40:1661) and, if a germline mutation is present, the leiomyoma is a component of hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome. This is an autosomal dominant syndrome of patients predisposed to the development of cutaneous and uterine leiomyomas, as well as an aggressive form of renal cell carcinoma (Cancer Genet 2012;205:377). Uterine leiomyomas in these patients are diagnosed at a mean age of 28 years and most women undergo myomectomy or hysterectomy in their thirties and 15% develop aggressive renal cell carcinomas, usually diagnosed between 37 and 44 years (Am J Surg Pathol 2016;40:865). Therefore, being able to morphologically identify FH-d leiomyomas can triage a patient for genetic testing and appropriate management if needed.
The patient had germline genetic testing and was found to harbor a FH variant of uncertain clinical significance. She is currently undergoing annual renal ultrasounds.
Test question answer:
D. Prominent macronucleoli with perinucleolar halos