17 June 2021 - Case of the Month #504
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Gary Tozbikian, Ohio State University, Columbus, Ohio (USA), for contributing this case and writing the discussion and to Dr. Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin (USA), for reviewing the discussion.
Advertisement
Case of the Month #504
Clinical history:
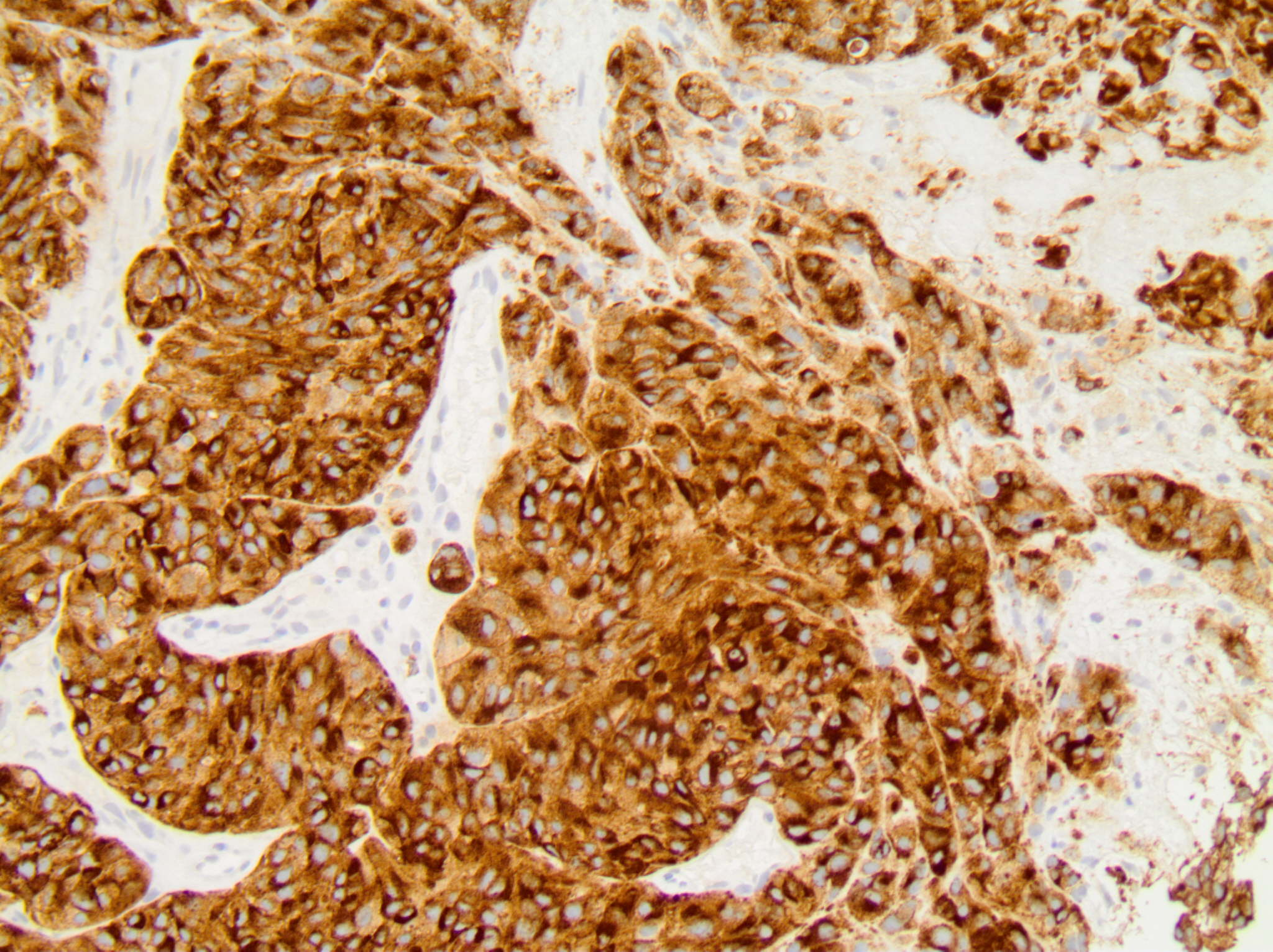
A 67 year old woman had an ultrasound guided core needle biopsy of a solitary, rapidly enlarging, 2.2 cm right breast mass. The patient previously had a wide local excision of a melanoma from the shoulder 20 years ago.
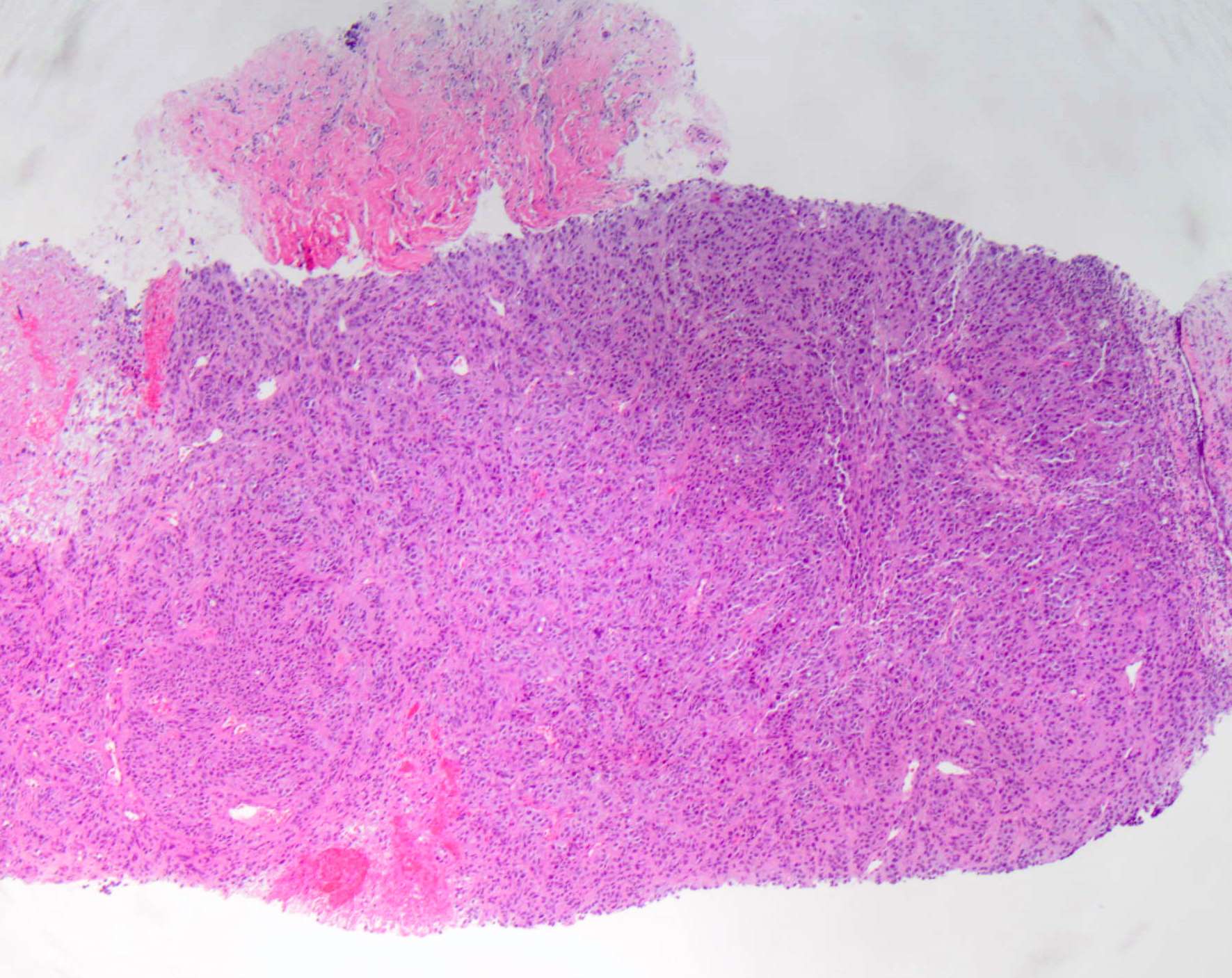
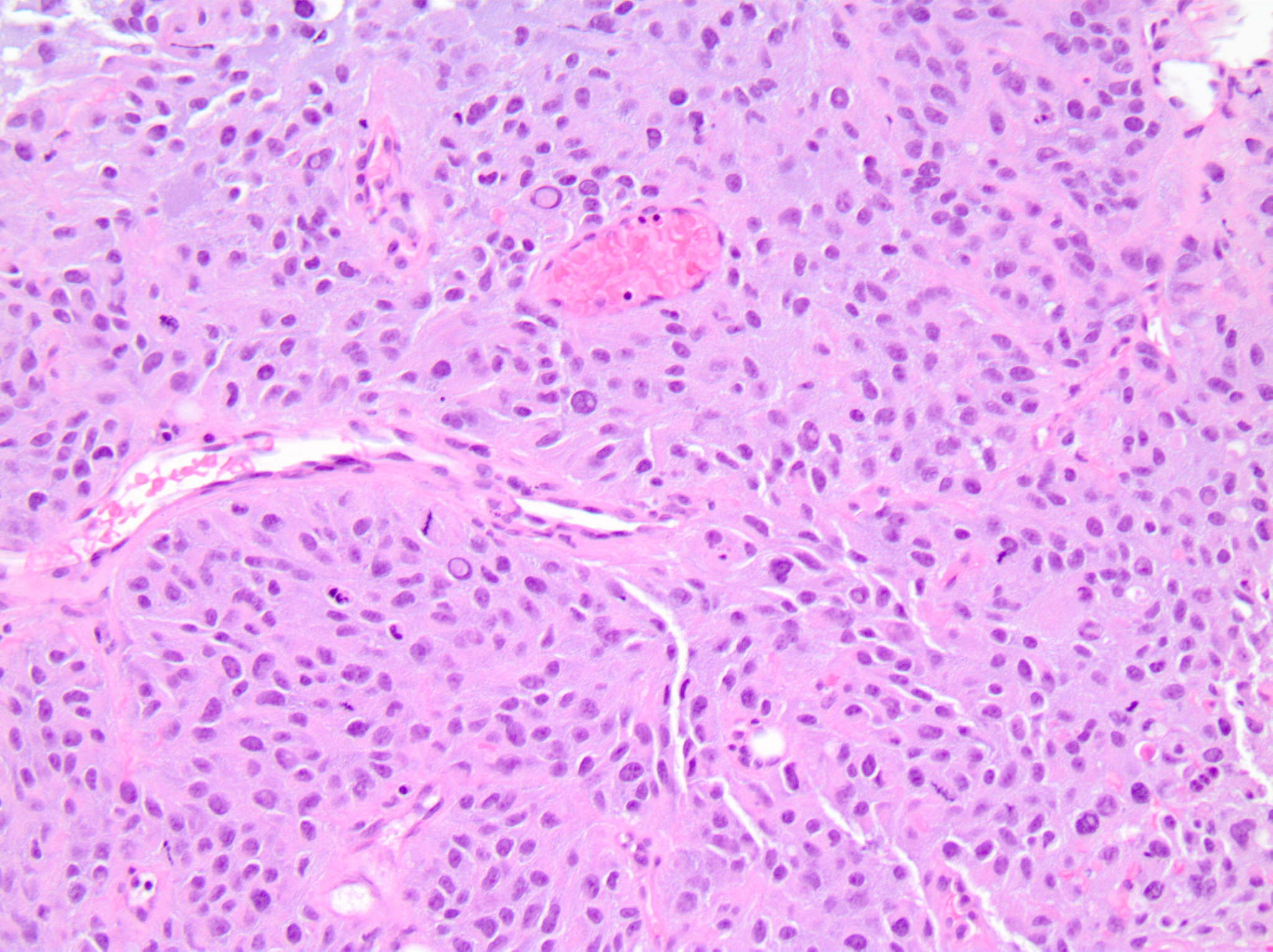
Histopathology images:
What is your diagnosis?
Diagnosis: Metastatic melanoma
Test question (answer at the end):
What panel of immunohistochemical stains would be most useful in distinguishing metastatic melanoma versus a primary breast malignancy?
A. AE1 / AE3, CK7, and estrogen receptor
B. AE1 / AE3, estrogen receptor and GATA3
C. CK7, mammaglobin and GCDFP-15
D. S100, HMB45 and AE1 / AE3
E. SOX10, GATA3 and estrogen receptor
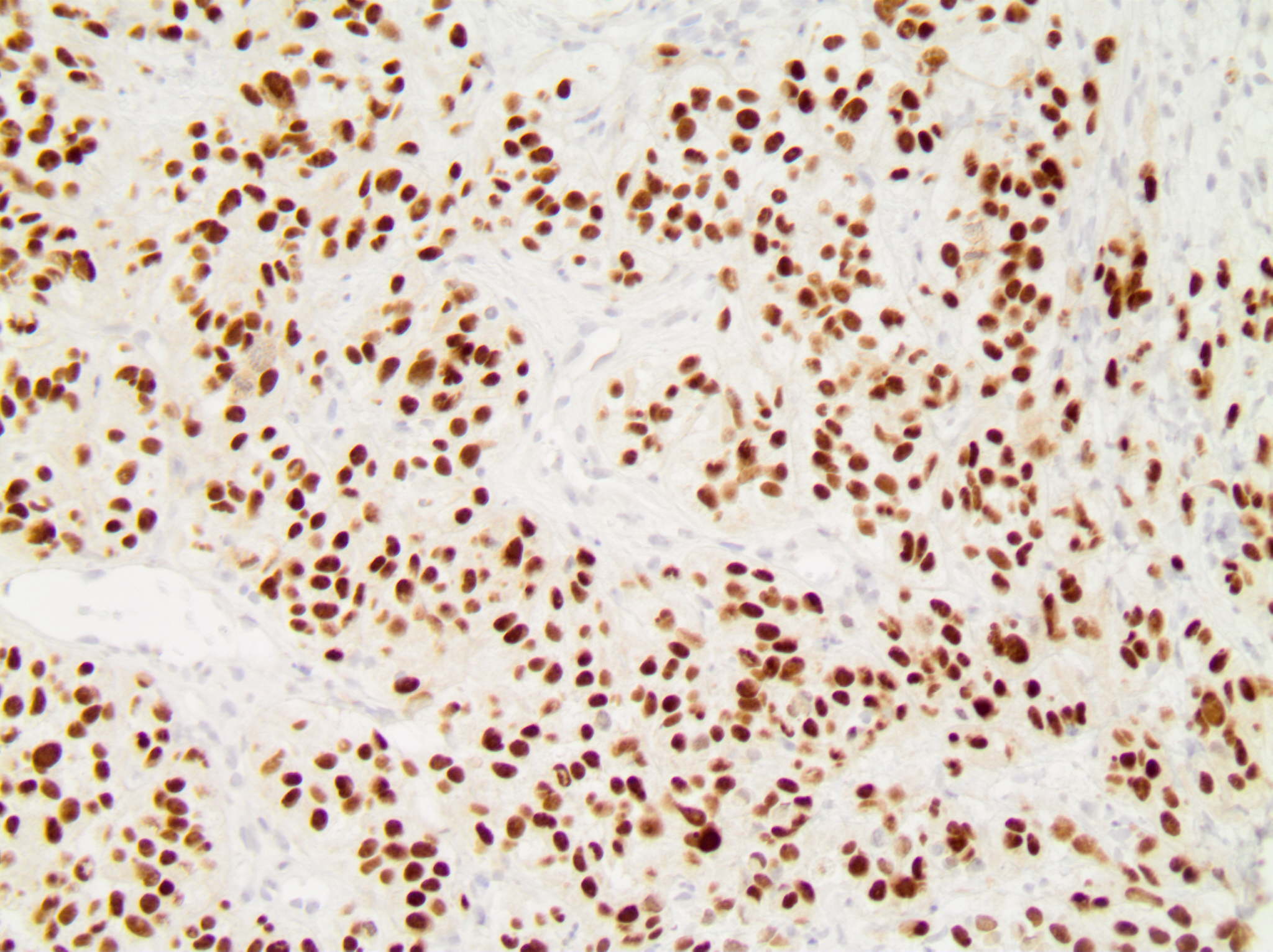
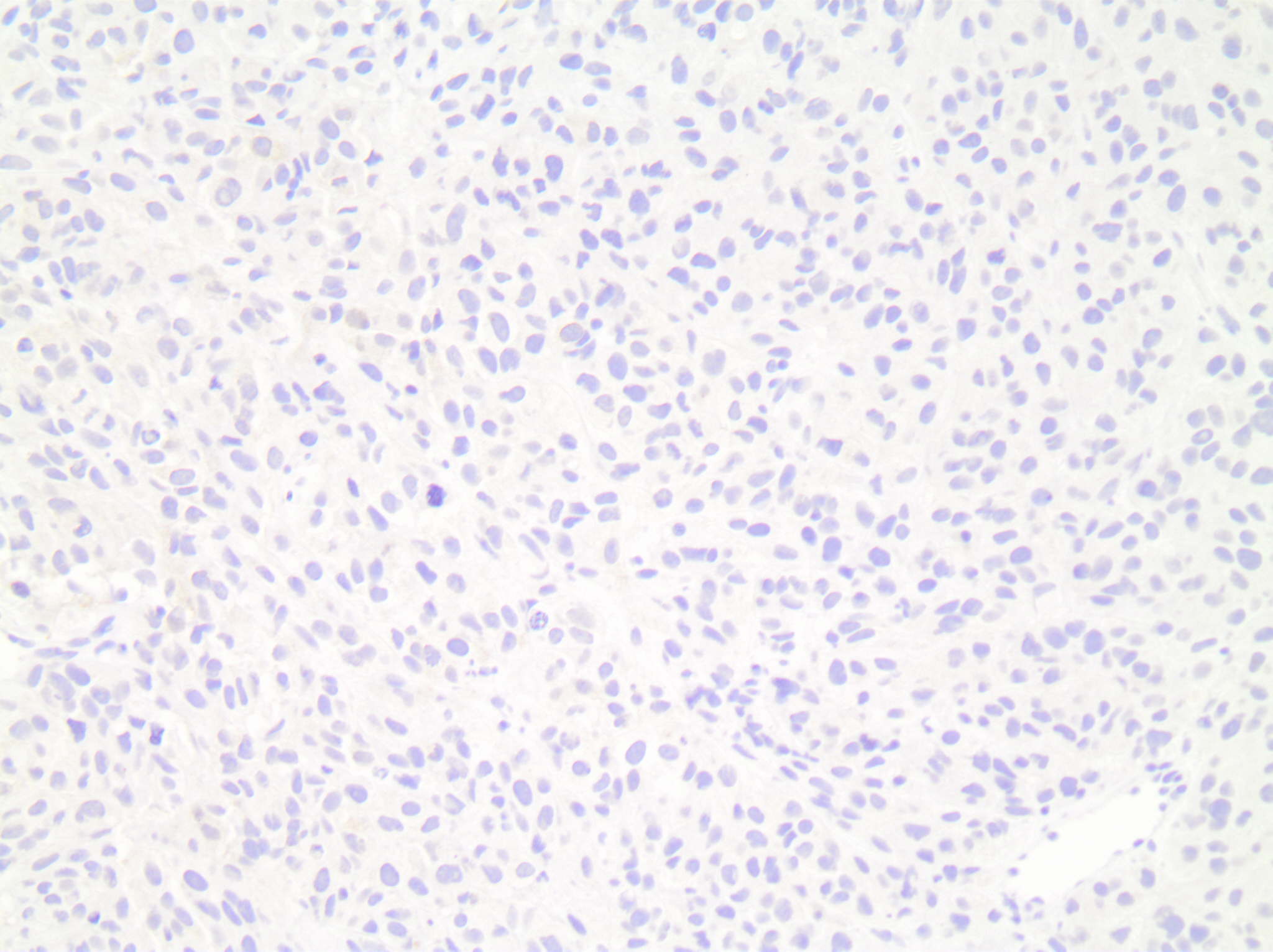
Stains:
Discussion:
A wide range of extramammary malignancies can metastasize to the breast. The most common nonmammary metastases to the breast are cutaneous malignant melanoma, lung and ovarian carcinomas. Most patients with nonmammary metastases to the breast have an established history of a previous malignancy. However, a long time interval between the primary malignancy and metastasis is frequently observed in melanoma.
Metastatic melanoma can mimic primary high grade invasive breast carcinoma, NST, particularly triple negative breast cancer (TNBC). The morphologic distinction with a TNBC may be difficult. Identification of an in situ component is a strong indication of a primary breast tumor. The presence of pigment, spindle cell morphology and intranuclear inclusions can suggest melanoma. There can be immunophenotype overlap between a TNBC and metastatic melanoma. Both lack expression of estrogen receptor, progesterone receptor and HER2. Breast lineage markers such as mammaglobin and GCDFP-15 have low sensitivity in TNBC. The breast lineage marker GATA3 is positive in only 41 - 66% of TNBC. The melanoma marker SOX10 can be positive in approximately 66% of TNBC. An immunohistochemical panel that includes a combination of cytokeratin stains and melanoma markers (e.g. AE1 / AE3, S100, HMB45) is most helpful in distinguishing a primary malignancy from metastatic melanoma.
References:
Hum Pathol 2019;85:221, Hum Pathol 2013;44:959, J Clin Pathol 2007;60:1333, Clin Oncol 1976;2:393, Hum Pathol 2014;45:2225, Hum Pathol 2015;46:1829
Test question answer:
D. S100, HMB45 and AE1 / AE3
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Gary Tozbikian, Ohio State University, Columbus, Ohio (USA), for contributing this case and writing the discussion and to Dr. Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin (USA), for reviewing the discussion.
Advertisement
Case of the Month #504
Clinical history:
A 67 year old woman had an ultrasound guided core needle biopsy of a solitary, rapidly enlarging, 2.2 cm right breast mass. The patient previously had a wide local excision of a melanoma from the shoulder 20 years ago.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Metastatic melanoma
Test question (answer at the end):
What panel of immunohistochemical stains would be most useful in distinguishing metastatic melanoma versus a primary breast malignancy?
A. AE1 / AE3, CK7, and estrogen receptor
B. AE1 / AE3, estrogen receptor and GATA3
C. CK7, mammaglobin and GCDFP-15
D. S100, HMB45 and AE1 / AE3
E. SOX10, GATA3 and estrogen receptor
Stains:
Discussion:
A wide range of extramammary malignancies can metastasize to the breast. The most common nonmammary metastases to the breast are cutaneous malignant melanoma, lung and ovarian carcinomas. Most patients with nonmammary metastases to the breast have an established history of a previous malignancy. However, a long time interval between the primary malignancy and metastasis is frequently observed in melanoma.
Metastatic melanoma can mimic primary high grade invasive breast carcinoma, NST, particularly triple negative breast cancer (TNBC). The morphologic distinction with a TNBC may be difficult. Identification of an in situ component is a strong indication of a primary breast tumor. The presence of pigment, spindle cell morphology and intranuclear inclusions can suggest melanoma. There can be immunophenotype overlap between a TNBC and metastatic melanoma. Both lack expression of estrogen receptor, progesterone receptor and HER2. Breast lineage markers such as mammaglobin and GCDFP-15 have low sensitivity in TNBC. The breast lineage marker GATA3 is positive in only 41 - 66% of TNBC. The melanoma marker SOX10 can be positive in approximately 66% of TNBC. An immunohistochemical panel that includes a combination of cytokeratin stains and melanoma markers (e.g. AE1 / AE3, S100, HMB45) is most helpful in distinguishing a primary malignancy from metastatic melanoma.
References:
Hum Pathol 2019;85:221, Hum Pathol 2013;44:959, J Clin Pathol 2007;60:1333, Clin Oncol 1976;2:393, Hum Pathol 2014;45:2225, Hum Pathol 2015;46:1829
Test question answer:
D. S100, HMB45 and AE1 / AE3