18 March 2021 - Case of the Month #501
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Constantina Petraki, Metropolitan Hospital, Athens (Greece) and the Genitourinary Pathology Society (GUPS) for contributing this case and discussion and to Dr. Nicole Andeen, Oregon Health and Science University, Portland, Oregon (USA), for reviewing the discussion.
Advertisement
Case of the Month #501
Clinical history:
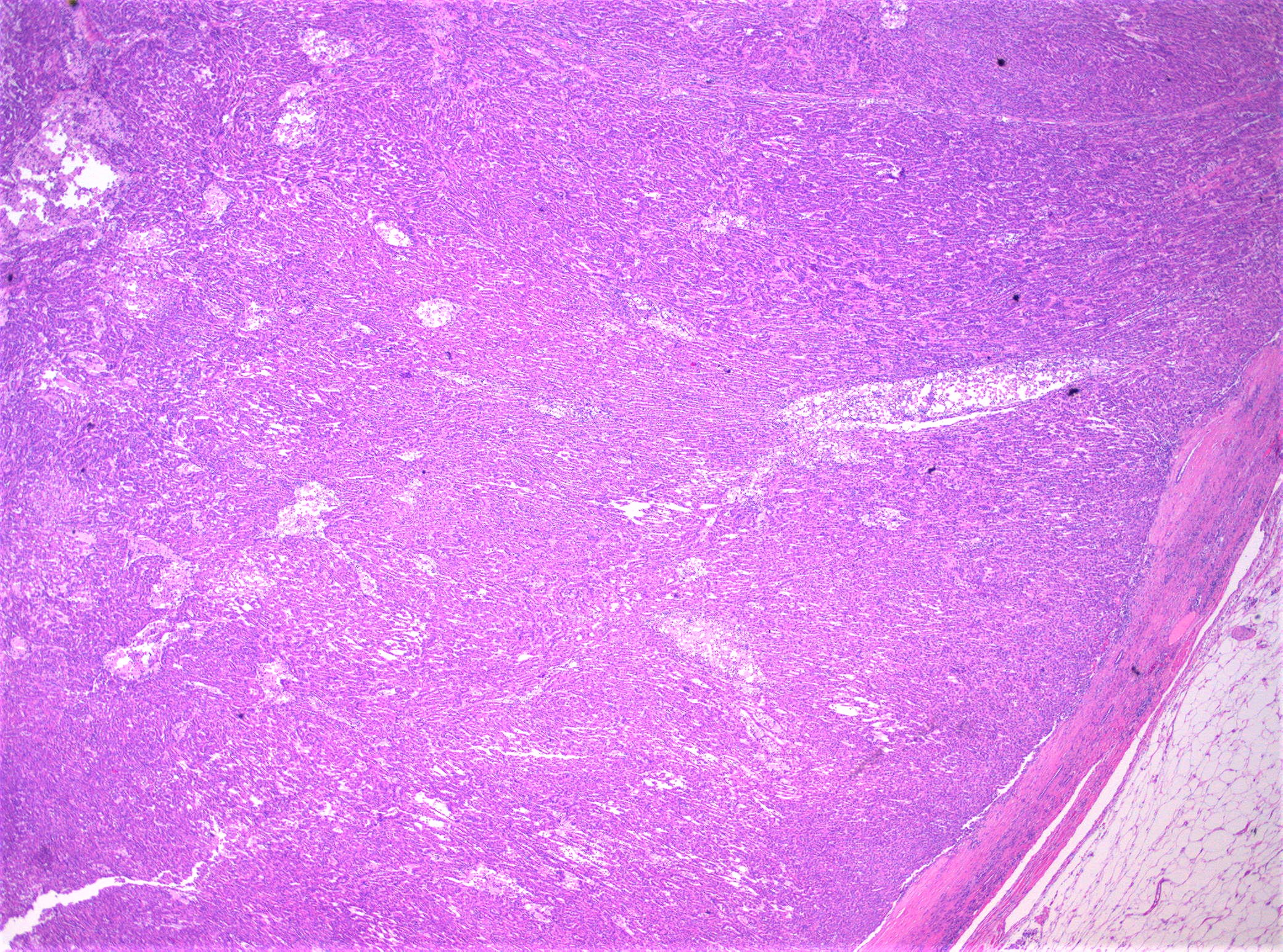
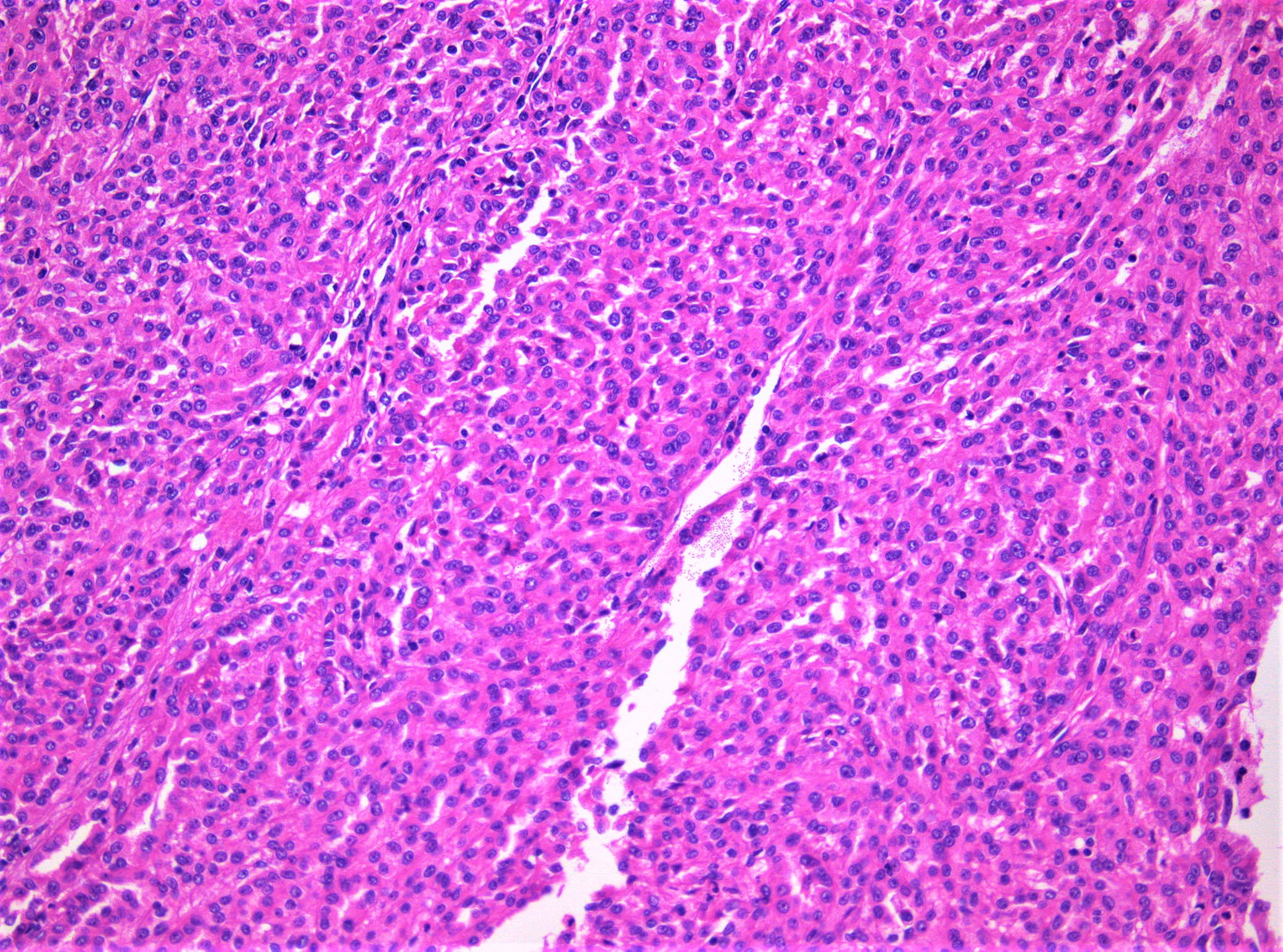
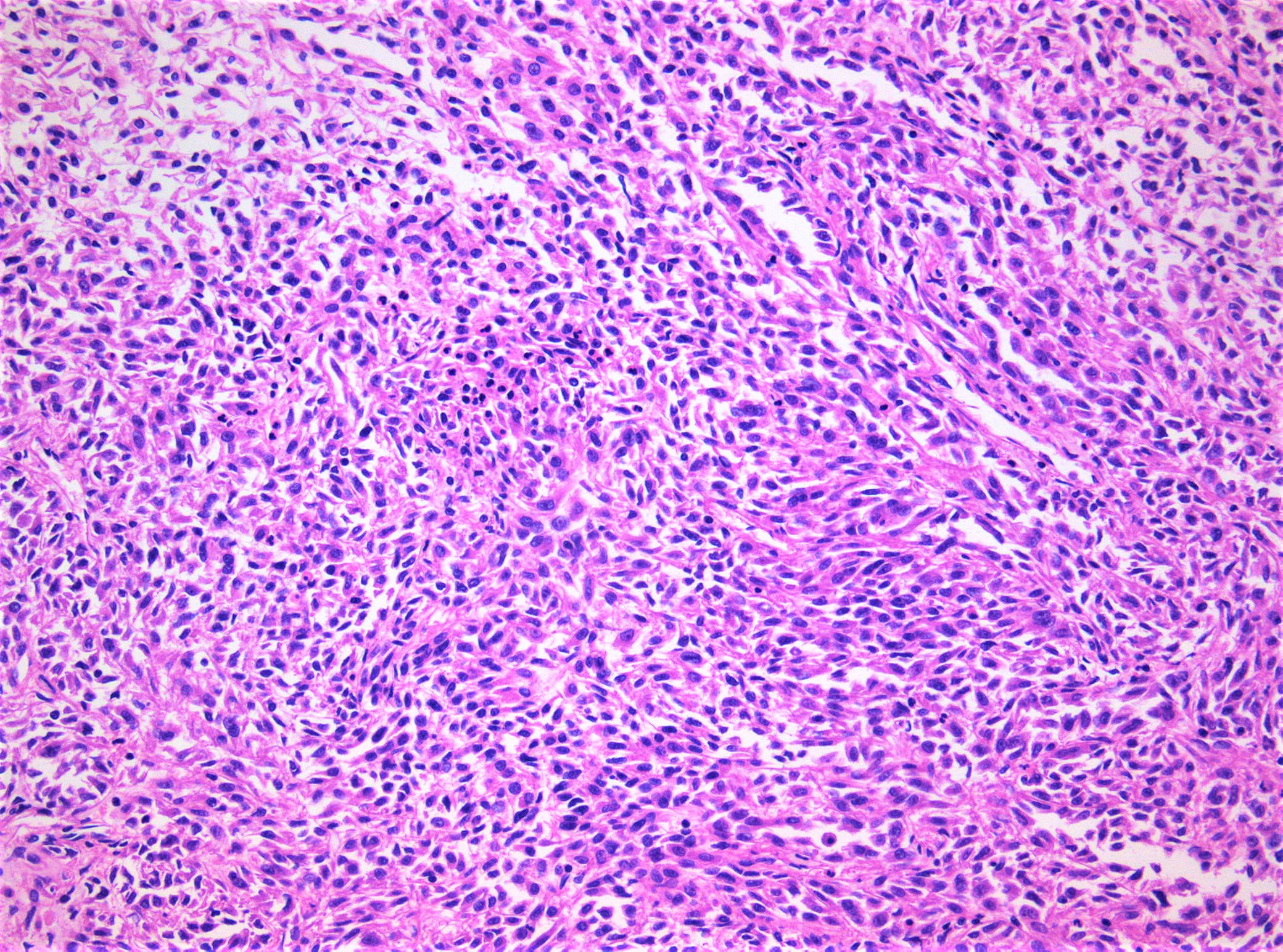
A woman in her 50s underwent nephrectomy for an incidentally identified 5.1 cm renal mass.
Histopathology images:
What is your diagnosis?
Diagnosis: Mucinous tubular and spindle cell carcinoma of the kidney
Test question (answer at the end):
If necessary, one reliable feature to distinguish mucinous tubular and spindle cell carcinoma from papillary renal cell carcinoma in a challenging case is
A. Clinical and radiographic evaluation
B. Genomic evaluation
C. Immunohistochemistry
D. Morphologic features of papillary growth and foam cells
Stains:
Discussion:
The tumor was circumscribed, tan-brown / yellow. Microscopic examination revealed a pT1b biphasic tumor with tubular and spindle cell morphology and focally mucinous stroma and foamy cells. The tumor cells were positive for PAX8, PAX2, AMACR and CK8/18. CK7, KSP-Cadherin, CAIX, CD15 and vimentin were focally positive. CD10 was mainly negative (shown). CD117, ALK1, CKHMW, CK20 and cathepsin K were negative. SDHB and fumarate hydratase were retained. The Ki67 / MIB1 index was low (≤ 5%).
Mucinous tubular and spindle cell carcinoma is a rare renal epithelial neoplasm characterized by tubular formations merging with bland spindle cells and a variably myxoid stroma. The nuclei have low grade features. Immunohistochemically, the tumor cells are generally positive for CK7, PAX8, PAX2 and AMACR and mostly negative for CD10. Most tumors have indolent behavior and recurrence is rare. Tumors with high grade transformation and metastases have been reported.
The differential diagnosis includes papillary renal cell carcinoma with solid growth pattern and papillary renal cell carcinoma with sarcomatoid transformation. The latter has high nuclear atypia in the stroma and is generally CD10 positive. The molecular genomic signature is useful - in mucinous tubular and spindle cell carcinoma, it is hypodiploid with multiple chromosomal losses (-1, -4, -6, -8, -9, -13, -14, -15, -22), some hypertriploid but no identifiable pattern, in contrast to the distinct signature of +7, +17 and loss of chromosome Y in papillary renal cell carcinoma.
References:
Clin Genitourin Cancer 2019;17:268, Indian J Cancer 2020;57:267
Test question answer:
B. Genomic evaluation. The papillary genomic signature of +7, +17 and loss of chromosome Y is not shared with mucinous tubular and spindle cell carcinoma.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Constantina Petraki, Metropolitan Hospital, Athens (Greece) and the Genitourinary Pathology Society (GUPS) for contributing this case and discussion and to Dr. Nicole Andeen, Oregon Health and Science University, Portland, Oregon (USA), for reviewing the discussion.
Advertisement
Case of the Month #501
Clinical history:
A woman in her 50s underwent nephrectomy for an incidentally identified 5.1 cm renal mass.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Mucinous tubular and spindle cell carcinoma of the kidney
Test question (answer at the end):
If necessary, one reliable feature to distinguish mucinous tubular and spindle cell carcinoma from papillary renal cell carcinoma in a challenging case is
A. Clinical and radiographic evaluation
B. Genomic evaluation
C. Immunohistochemistry
D. Morphologic features of papillary growth and foam cells
Stains:
Discussion:
The tumor was circumscribed, tan-brown / yellow. Microscopic examination revealed a pT1b biphasic tumor with tubular and spindle cell morphology and focally mucinous stroma and foamy cells. The tumor cells were positive for PAX8, PAX2, AMACR and CK8/18. CK7, KSP-Cadherin, CAIX, CD15 and vimentin were focally positive. CD10 was mainly negative (shown). CD117, ALK1, CKHMW, CK20 and cathepsin K were negative. SDHB and fumarate hydratase were retained. The Ki67 / MIB1 index was low (≤ 5%).
Mucinous tubular and spindle cell carcinoma is a rare renal epithelial neoplasm characterized by tubular formations merging with bland spindle cells and a variably myxoid stroma. The nuclei have low grade features. Immunohistochemically, the tumor cells are generally positive for CK7, PAX8, PAX2 and AMACR and mostly negative for CD10. Most tumors have indolent behavior and recurrence is rare. Tumors with high grade transformation and metastases have been reported.
The differential diagnosis includes papillary renal cell carcinoma with solid growth pattern and papillary renal cell carcinoma with sarcomatoid transformation. The latter has high nuclear atypia in the stroma and is generally CD10 positive. The molecular genomic signature is useful - in mucinous tubular and spindle cell carcinoma, it is hypodiploid with multiple chromosomal losses (-1, -4, -6, -8, -9, -13, -14, -15, -22), some hypertriploid but no identifiable pattern, in contrast to the distinct signature of +7, +17 and loss of chromosome Y in papillary renal cell carcinoma.
References:
Clin Genitourin Cancer 2019;17:268, Indian J Cancer 2020;57:267
Test question answer:
B. Genomic evaluation. The papillary genomic signature of +7, +17 and loss of chromosome Y is not shared with mucinous tubular and spindle cell carcinoma.