14 February 2018 - Case of the Week #449
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Sajna VM Kutty, Aster MIMS, Kerala (India) for contributing this case and part of the discussion and Dr. Belinda Lategan, St. Boniface Hospital, Winnipeg, Manitoba (Canada) for editing the discussion. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
Advertisement
Website news:
(1) We welcome Michael Clay, M.D., to our Editorial Board. Dr. Clay is on staff at St. Jude Children's Research Hospital in Tennessee. He will be our editor for soft tissue, molecular and pediatric pathology topics.
(2) We now have a separate Payment page, distinct from the Advertise page (they were together). The Advertise page will give more information about banner and email advertising. Also, the Amazon link on the top line of the banner was removed (it is still in the footer), and we moved Contact us from the bottom of the header to the top of the header (to make room for the payment link).
(3) January 2018 was busy at PathologyOutlines.com with a record 90 job postings and 31 fellowship ads. We also had record page views for our Jobs page (57,077) and website (2,061,665).
We appreciate our advertisers, who enable us to provide this labor intensive resource to the pathology community.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #449
Clinical history:
A 33 year old man presented with post traumatic pain and a large mass in his right upper thigh. The overlying skin was normal and there was no regional adenopathy or distal neurovascular deficits. A wide local excision revealed an 8x6 cm mass arising from the adductor longus muscle. Vessels were uninvolved.
Gross image:
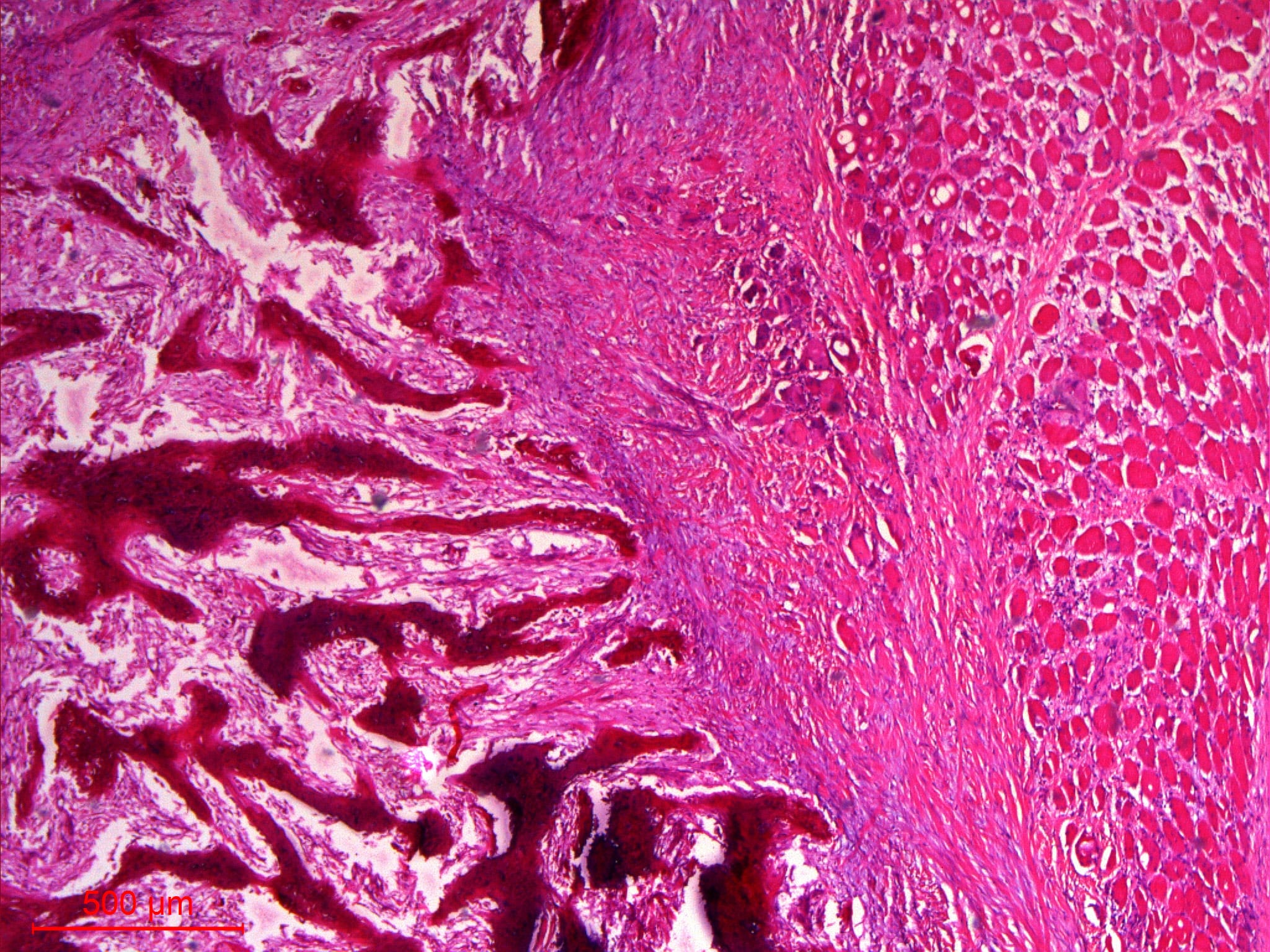
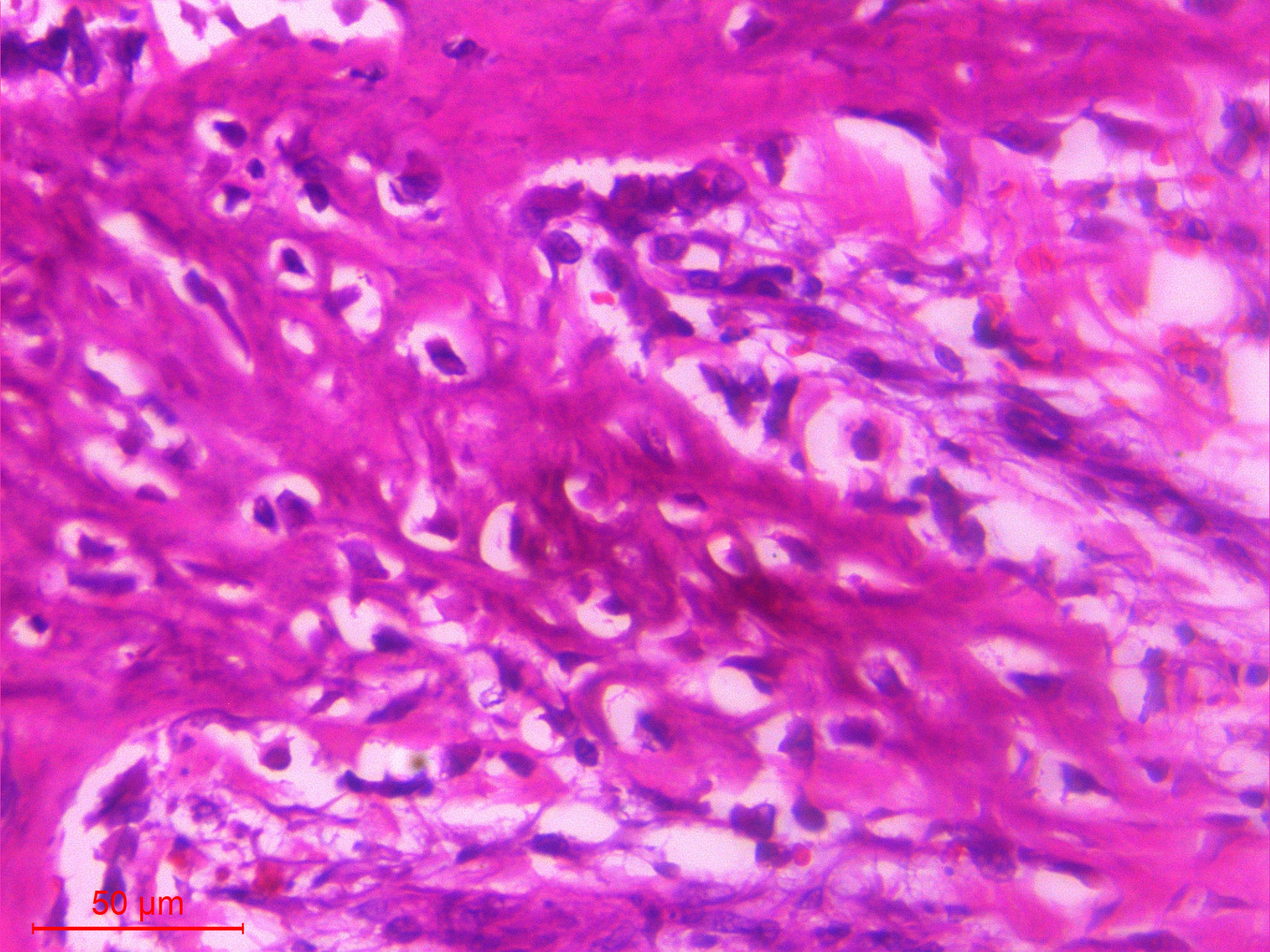
Histopathology images:
What is your diagnosis?
Diagnosis:
Myositis Ossificans
Test question (answer at the end):
Myositis ossificans is exclusively seen following blunt force trauma to the extremities in young, physically active males, and the diagnosis should not be rendered in cases lacking this history.
A. True
B. False
Discussion (from author):
Myositis ossificans is a self-limiting, nonneoplastic, heterotopic ossifying lesion predominantly affecting the extremities. The thigh is a common site. Analogous lesions occur in the subcutis (panniculitis ossificans), fascia or tendons (fasciitis ossificans) and in the fingers of older manual laborers (fibro-osseous pseudotumor of digits). The terminology "myositis ossificans traumatica" may be used if trauma precedes the swelling (60-75% of cases) or "myositis ossificans circumscripta" if localized, regardless of preceding trauma history. Myositis ossificans progressiva (pediatric fibrodysplasia ossificans progressica) is a rare and disabling form of progressive heterotopic ossification presenting in childhood.
In the early stages, myositis ossificans lesions are cellular and composed mainly of haphazardly arranged fibroblasts lacking atypia. In the intermediate stage, the fibroblasts differentiate into osteoblasts which lay down osteoid at the periphery, progressing centripetally. Mature bone is seen in late stage lesions. Cartilage is rare. This progression imparts the appearance of variably well defined zonation, with a central fibroblastic zone surrounded by ossification. The entire process takes around 8 weeks and may regress entirely in some patients (BMJ Case Rep 2013;2013, Int J Surg Case Rep 2016;26:84).
A clinical history of trauma may precede the onset of symptoms, especially in young, active males. A circumscribed lesion with periosteal reaction and peripheral "eggshell" calcification is seen on imaging, particularly in more mature lesions.
The clinical differential diagnosis includes soft tissue sarcoma, extraosseous osteosarcoma and osseous metastasis, particularly when there is no history of trauma and significant ossification leads to a hard mass on palpation. The absence of atypia or outright malignant features in addition to relevant clinical history allows for differentiating myositis ossificans from malignant entities (Pol J Radiol 2014;79:228). Immunohistochemistry is generally not helpful in diagnosis. As expected, fibroblasts and myofibroblasts are highlighted by vimentin and have more variable expression of actin and desmin. Myositis ossificans traumatica is a polyclonal process, although clonal USP6 rearrangements have also been demonstrated (these lesions are likely better characterized as aneurysmal bone cysts). Myositis ossificans progressiva is due to a recurrent missense mutation in the GS activation domain of ACVR1/ALK2 (Bone 2013;57:386). Noggin mutations have also been reported (Genet Couns 2005;16:149).
Additional references:
Gokkus A, Sagtas E, Suslu FE and Aydin AT. Myositis ossificans circumscripta, secondary to high-velocity gunshot and fragment wound that causes sciatica (BMJ Case Rep 2013 Oct 17;2013)
Spinelli MS, et al. A case of parosteal osteosarcoma with a rare complication of myositis ossificans (World J Surg Oncol 2012;10:260)
Weiss S.W., Goldblum J.R., Folpe A.L.: Enzinger and Weiss’s Soft tissue Tumors, 5th ed.
Test Question Answer:
B. False.
A history of preceding trauma can be elicited in up to 60-75% of cases. Although an extremity is the most common site, these lesions can occur in any muscle in the body, as illustrated in numerous case reports in the literature. Lesions with identical histologic features are also seen in the subcutis, digits, fascia and tendons.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. Sajna VM Kutty, Aster MIMS, Kerala (India) for contributing this case and part of the discussion and Dr. Belinda Lategan, St. Boniface Hospital, Winnipeg, Manitoba (Canada) for editing the discussion. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
Sign up to receive our What's New in Pathology Email Newsletter
Written by our Editorial Board, it is sent out every 3-4 months.
Subscribe by clicking here.
Visit our booth #711 at USCAP to receive
a folder with all seven What's New newsletters.
Website news:
(1) We welcome Michael Clay, M.D., to our Editorial Board. Dr. Clay is on staff at St. Jude Children's Research Hospital in Tennessee. He will be our editor for soft tissue, molecular and pediatric pathology topics.
(2) We now have a separate Payment page, distinct from the Advertise page (they were together). The Advertise page will give more information about banner and email advertising. Also, the Amazon link on the top line of the banner was removed (it is still in the footer), and we moved Contact us from the bottom of the header to the top of the header (to make room for the payment link).
(3) January 2018 was busy at PathologyOutlines.com with a record 90 job postings and 31 fellowship ads. We also had record page views for our Jobs page (57,077) and website (2,061,665).
We appreciate our advertisers, who enable us to provide this labor intensive resource to the pathology community.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #449
Clinical history:
A 33 year old man presented with post traumatic pain and a large mass in his right upper thigh. The overlying skin was normal and there was no regional adenopathy or distal neurovascular deficits. A wide local excision revealed an 8x6 cm mass arising from the adductor longus muscle. Vessels were uninvolved.
Gross image:
Histopathology images:
What is your diagnosis?
Diagnosis:
Myositis Ossificans
Test question (answer at the end):
Myositis ossificans is exclusively seen following blunt force trauma to the extremities in young, physically active males, and the diagnosis should not be rendered in cases lacking this history.
A. True
B. False
Discussion (from author):
Myositis ossificans is a self-limiting, nonneoplastic, heterotopic ossifying lesion predominantly affecting the extremities. The thigh is a common site. Analogous lesions occur in the subcutis (panniculitis ossificans), fascia or tendons (fasciitis ossificans) and in the fingers of older manual laborers (fibro-osseous pseudotumor of digits). The terminology "myositis ossificans traumatica" may be used if trauma precedes the swelling (60-75% of cases) or "myositis ossificans circumscripta" if localized, regardless of preceding trauma history. Myositis ossificans progressiva (pediatric fibrodysplasia ossificans progressica) is a rare and disabling form of progressive heterotopic ossification presenting in childhood.
In the early stages, myositis ossificans lesions are cellular and composed mainly of haphazardly arranged fibroblasts lacking atypia. In the intermediate stage, the fibroblasts differentiate into osteoblasts which lay down osteoid at the periphery, progressing centripetally. Mature bone is seen in late stage lesions. Cartilage is rare. This progression imparts the appearance of variably well defined zonation, with a central fibroblastic zone surrounded by ossification. The entire process takes around 8 weeks and may regress entirely in some patients (BMJ Case Rep 2013;2013, Int J Surg Case Rep 2016;26:84).
A clinical history of trauma may precede the onset of symptoms, especially in young, active males. A circumscribed lesion with periosteal reaction and peripheral "eggshell" calcification is seen on imaging, particularly in more mature lesions.
The clinical differential diagnosis includes soft tissue sarcoma, extraosseous osteosarcoma and osseous metastasis, particularly when there is no history of trauma and significant ossification leads to a hard mass on palpation. The absence of atypia or outright malignant features in addition to relevant clinical history allows for differentiating myositis ossificans from malignant entities (Pol J Radiol 2014;79:228). Immunohistochemistry is generally not helpful in diagnosis. As expected, fibroblasts and myofibroblasts are highlighted by vimentin and have more variable expression of actin and desmin. Myositis ossificans traumatica is a polyclonal process, although clonal USP6 rearrangements have also been demonstrated (these lesions are likely better characterized as aneurysmal bone cysts). Myositis ossificans progressiva is due to a recurrent missense mutation in the GS activation domain of ACVR1/ALK2 (Bone 2013;57:386). Noggin mutations have also been reported (Genet Couns 2005;16:149).
Additional references:
Gokkus A, Sagtas E, Suslu FE and Aydin AT. Myositis ossificans circumscripta, secondary to high-velocity gunshot and fragment wound that causes sciatica (BMJ Case Rep 2013 Oct 17;2013)
Spinelli MS, et al. A case of parosteal osteosarcoma with a rare complication of myositis ossificans (World J Surg Oncol 2012;10:260)
Weiss S.W., Goldblum J.R., Folpe A.L.: Enzinger and Weiss’s Soft tissue Tumors, 5th ed.
Test Question Answer:
B. False.
A history of preceding trauma can be elicited in up to 60-75% of cases. Although an extremity is the most common site, these lesions can occur in any muscle in the body, as illustrated in numerous case reports in the literature. Lesions with identical histologic features are also seen in the subcutis, digits, fascia and tendons.