10 May 2017 - Case of the Week #424
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. R. F. Chinoy, Prince Aly Khan Hospital, Mumbai (India) for contributing this case and Dr. Belinda Lategan, St. Boniface Hospital Winnipeg, Manitoba (Canada) for writing the discussion. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
Advertisement
Website news:
(1) Our request this week is for micro images relevant to NKX3-1 in normal prostate, PIN, prostatic adenocarcinoma, other. If you own images of these entities, please email them as attachments to Dr. Nat Pernick at NatPernick@gmail.com, with any corresponding clinical history. There is no payment for image contributions, but we will acknowledge you as contributor, so please indicate how you want your name to be displayed.
(2) We have now posted versions of the Jobs, Fellowships, and Conferences pages as of March 1, 2017, April 1, 2017 and May 1, 2017. We have them posted as far back as January 2012. The format is the name of the file, plus yyyymm, where yyyy is the year and mm is the month. So, for example, jobs posted as of April 1, 2016 are at http://pathologyoutlines.com/jobs201604.html.
(3) We have now posted the Jobs Report for the first quarter of 2017, click here. It is also accessible from the Jobs page by clicking on the orange link.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #424
Clinical history:
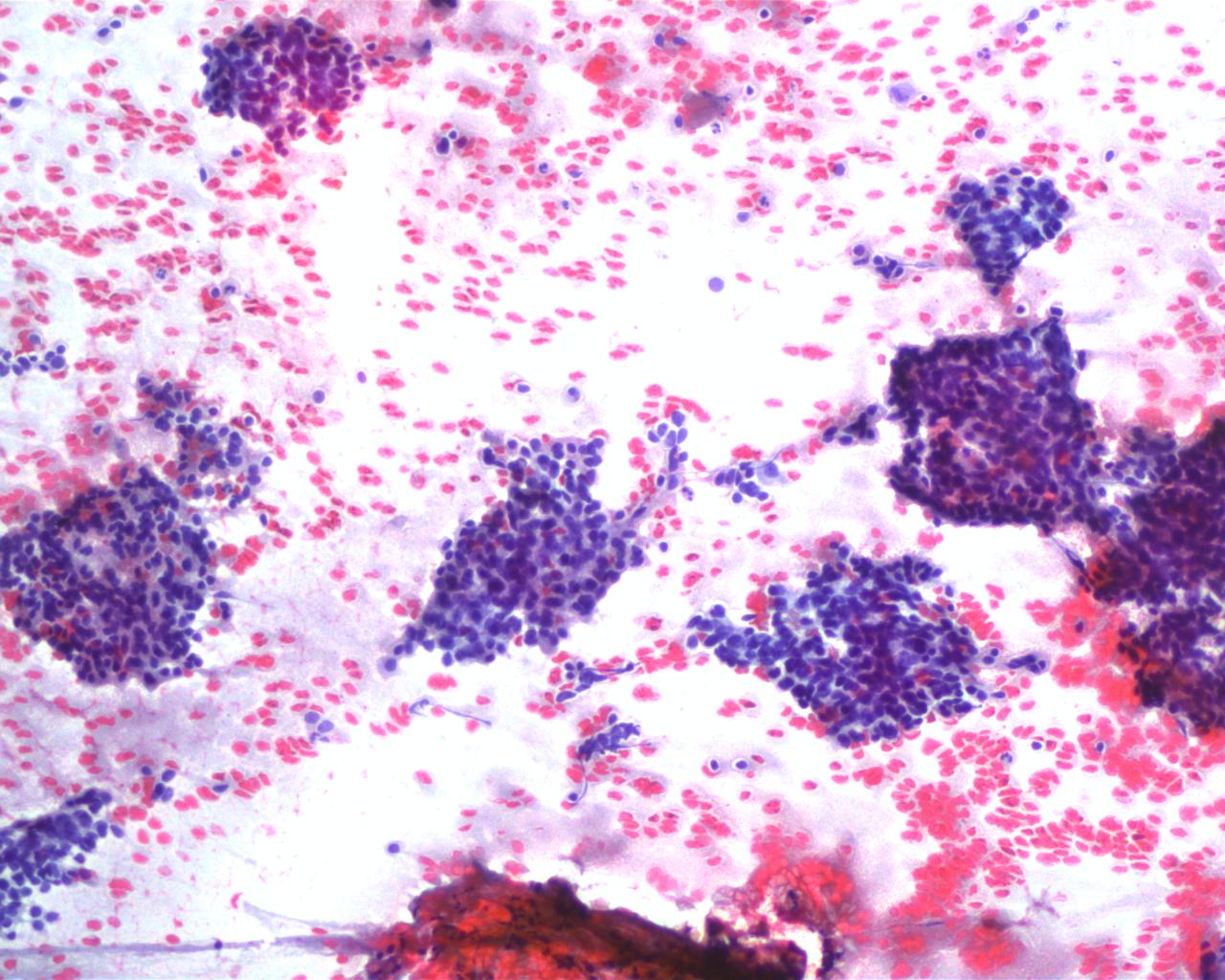
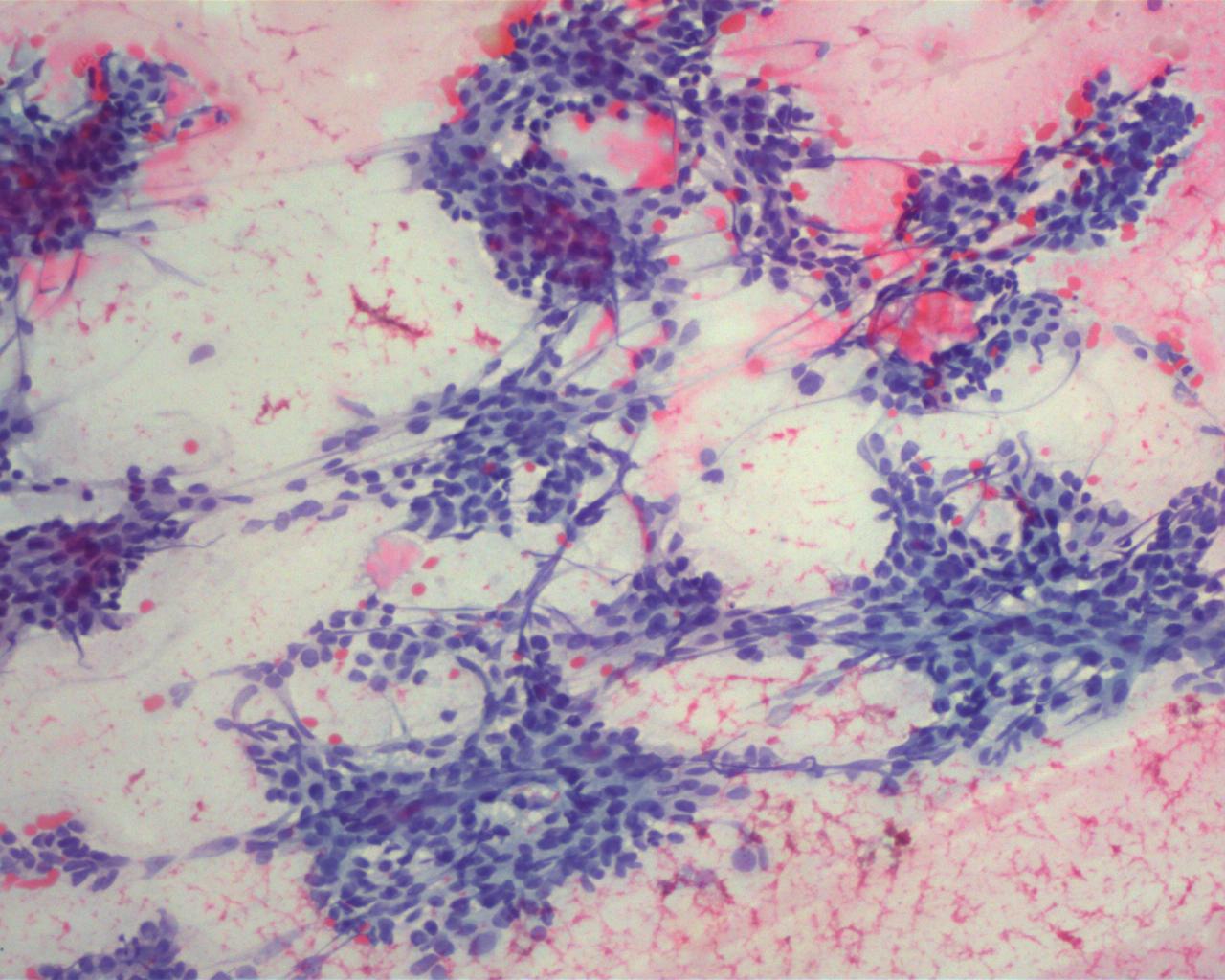
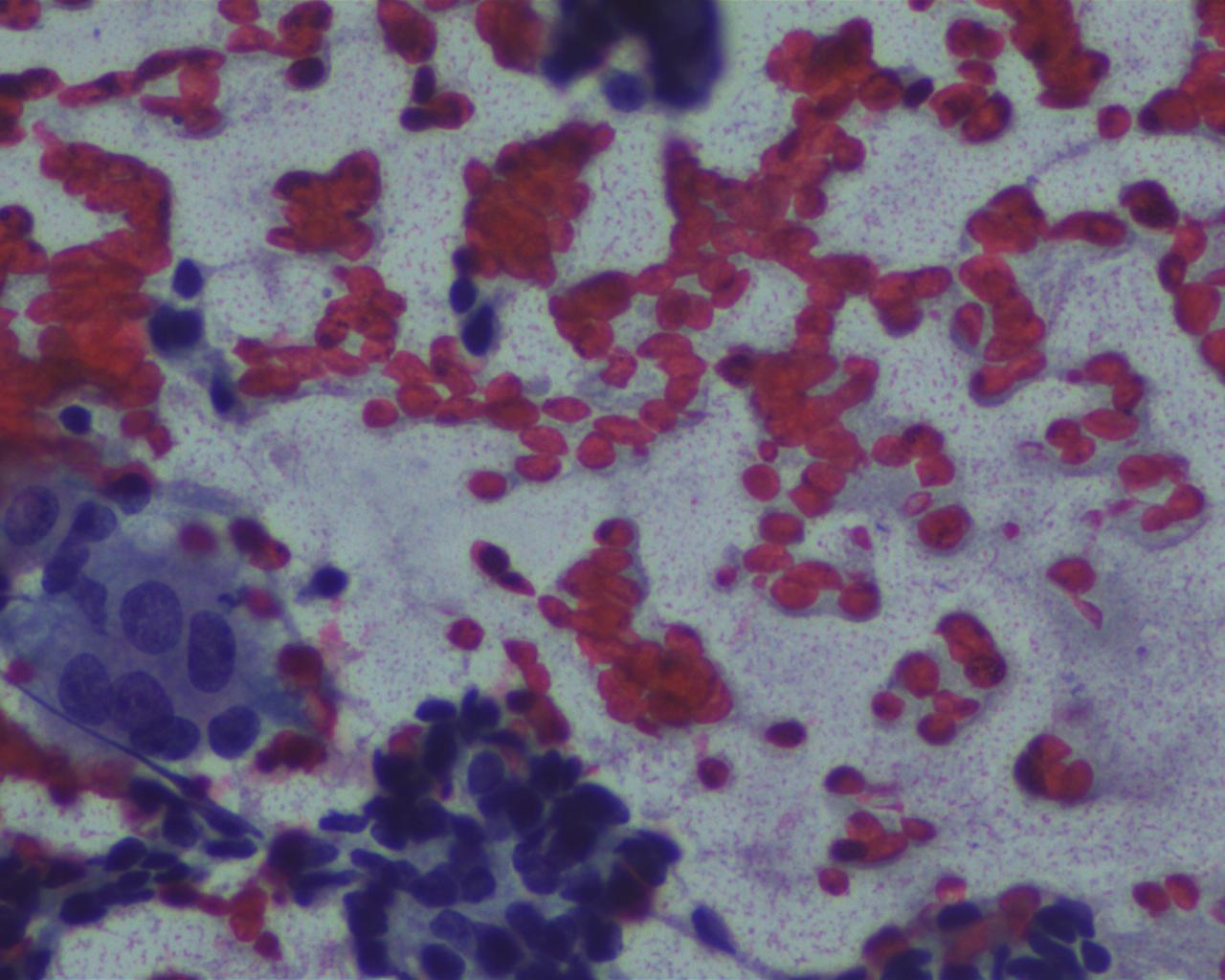
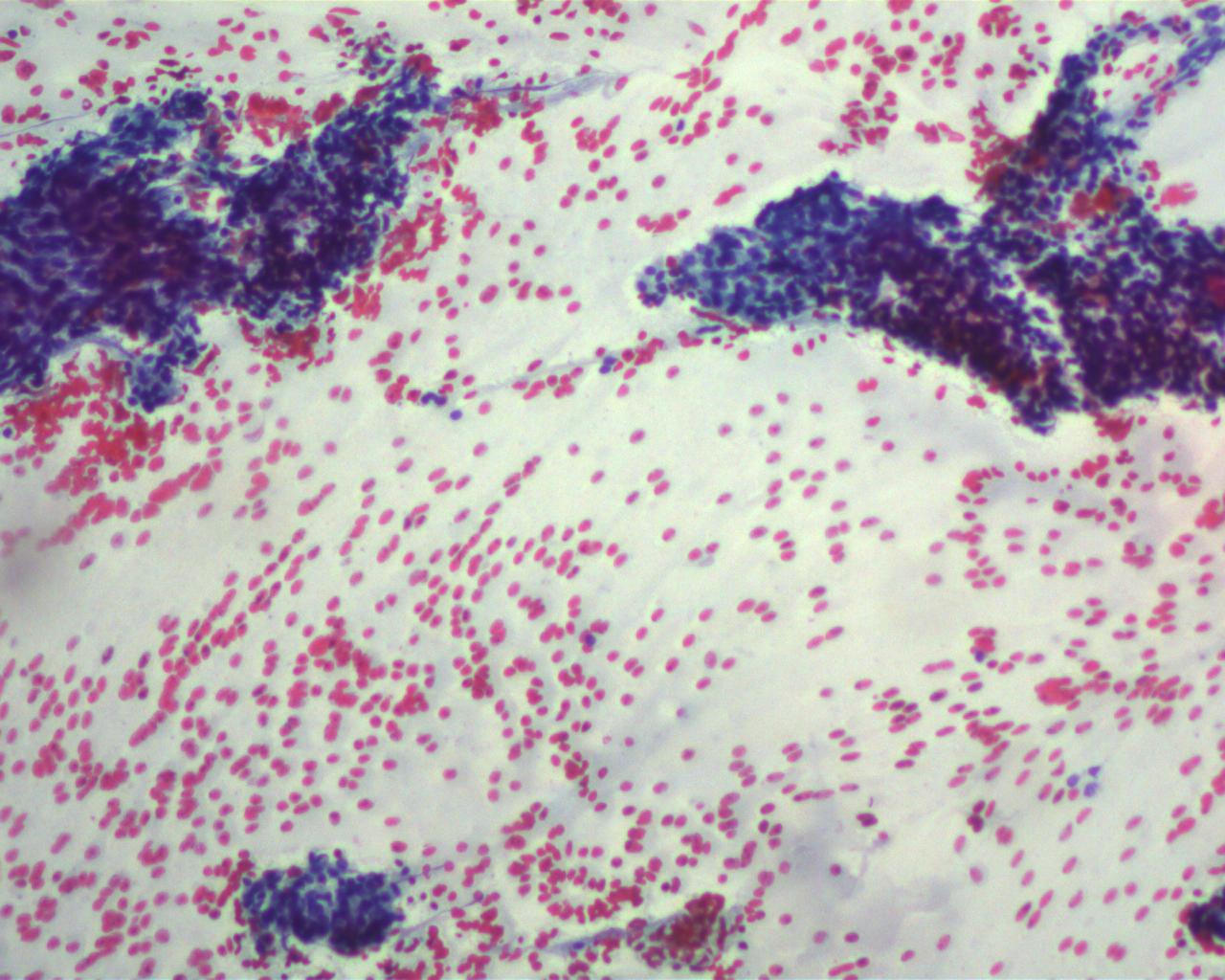
A 34 year old man presented with an occipital nodule. Fine needle aspiration was performed, followed by excision.
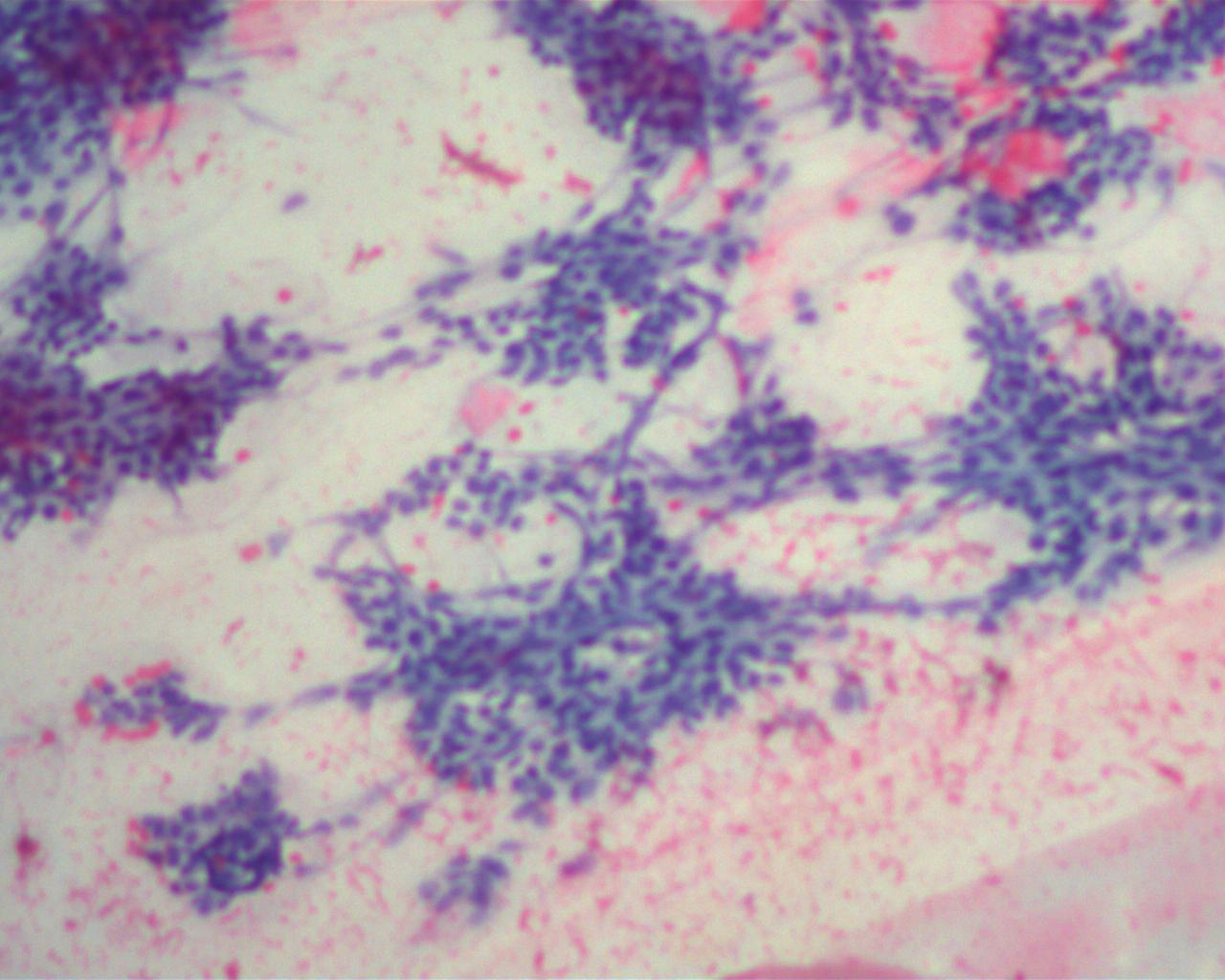
Cytology images:
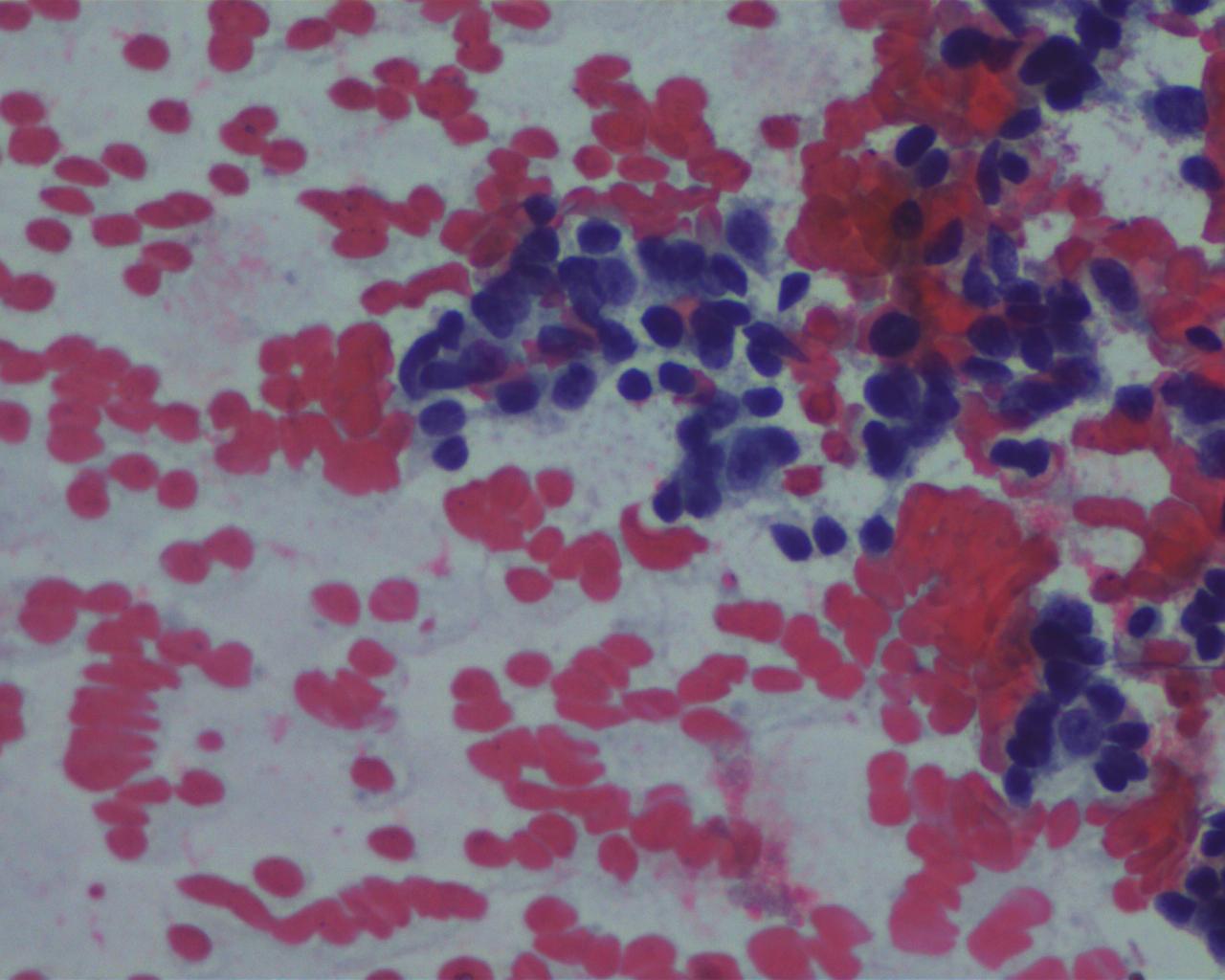
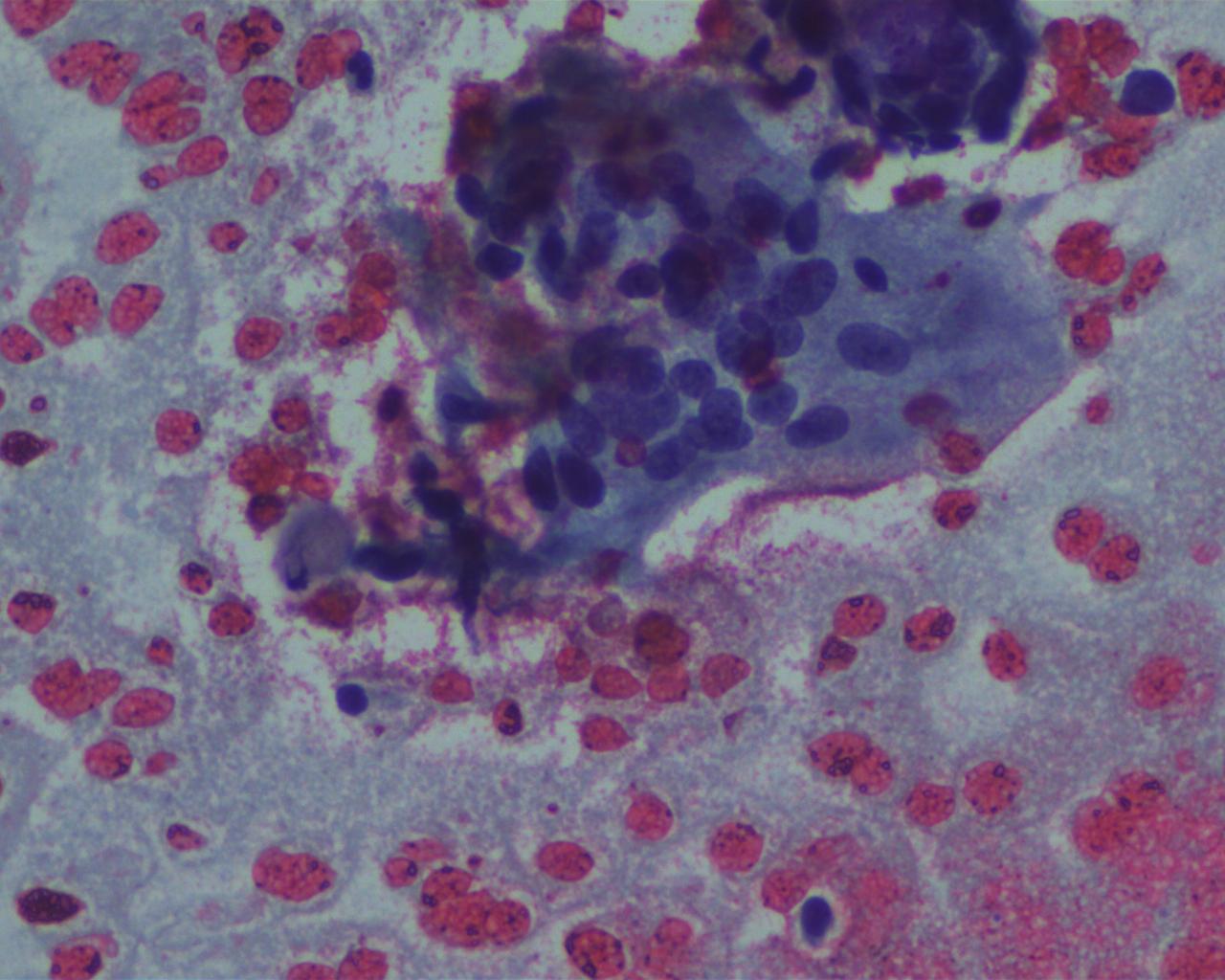
Additional cytology images:
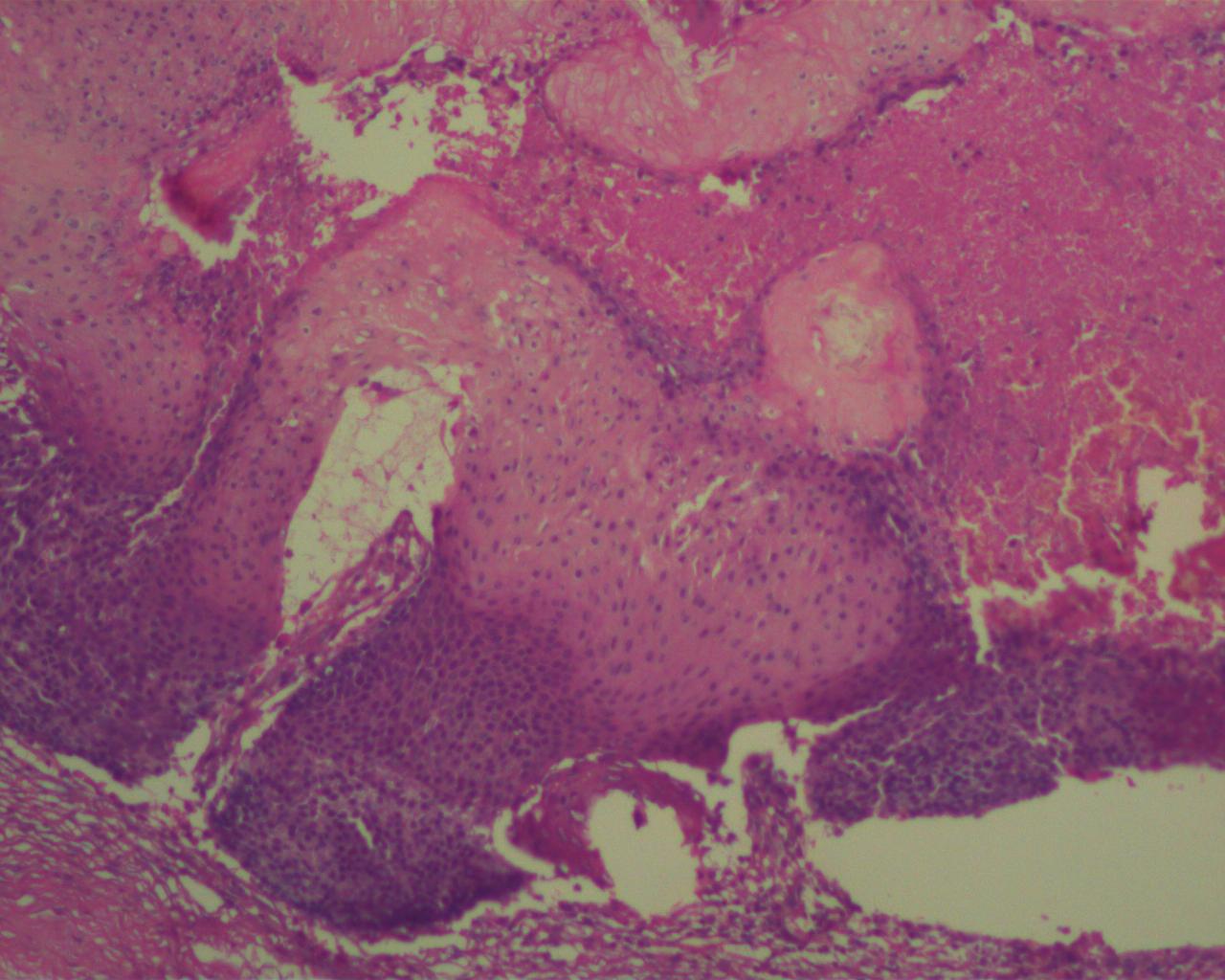
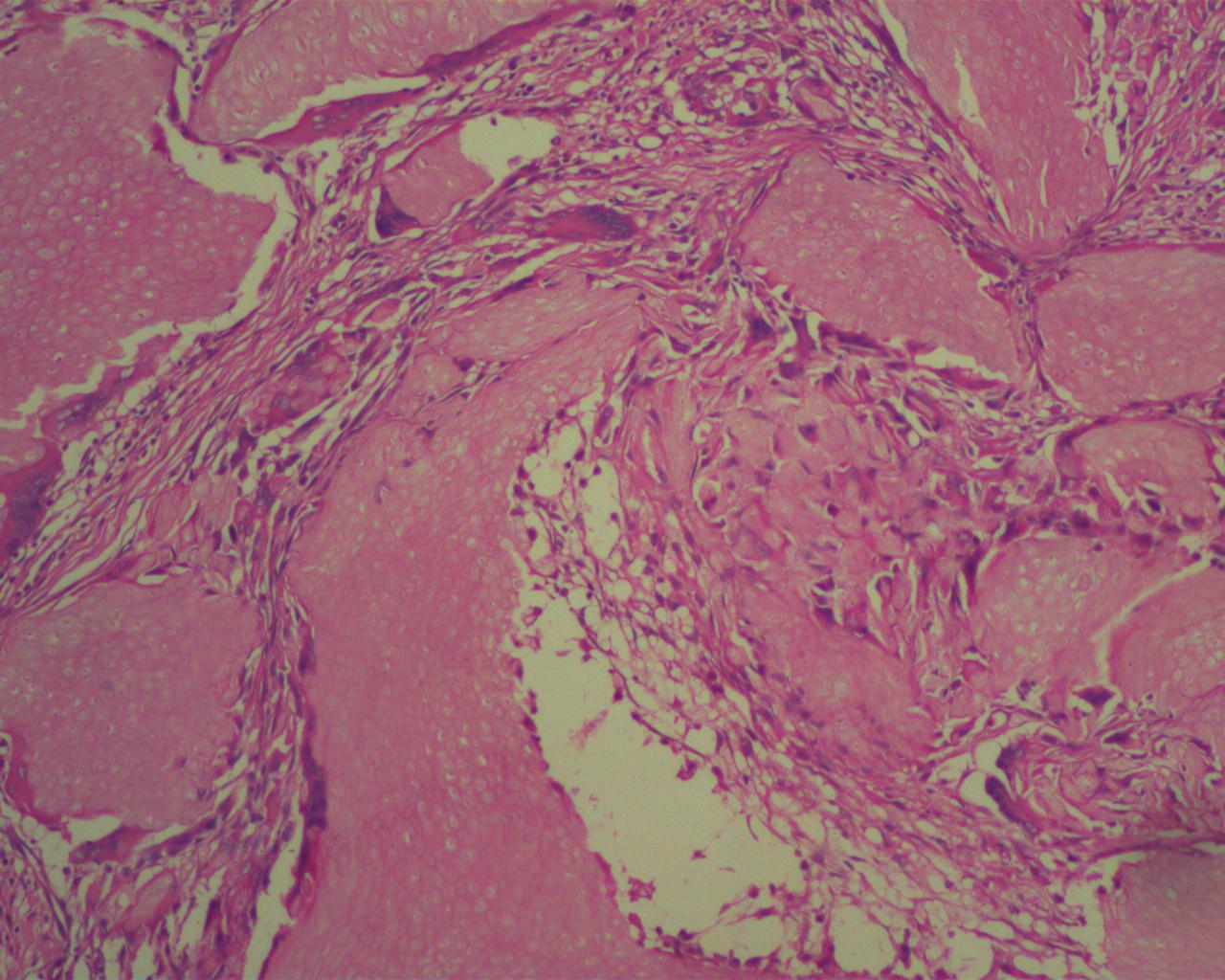
Histopathology images:
Additional histopathology images:
What is your diagnosis?
Diagnosis:
Pilomatrixoma (pilomatricoma, calcifying epithelioma of Malherbe)
Test question (answer at the end):
Which of the following are not typical of pilomatrixoma? (choose all that are appropriate)
A. Calcification, ossification and extramedullary hematopioiesis
B. Sheets of basaloid cells, occasionally with increased mitotic activity, Shadow cells, trichilemmal-type keratinization
C. Budding nests of atypical basaloid cells associated with a desmoplastic stromal response, zonal necrosis and marked cytologic atypia
D. Recurrence following local excision
Discussion:
Pilomatixoma (pilomatricoma, calcifying epithelioma of Malherbe) is a benign skin appendigeal tumor with differentiation towards the follicular matrix. Lesions typically arise either in the head and neck or the upper extremities of children and young adults, with a second peak in incidence in individuals over 50 years old.
Histologic features are characteristic. Pilomatrixomas, often partially cystic in early lesions, contain solid nests/sheets of basaloid cells with trichilemmal-type keratinization transitioning into shadow cells, amorphous keratinous debris and foci of calcification more centrally. Additional features include ossification, extramedullary hematopoiesis and foreign body type inflammatory response. Variants may demonstrate pigmentation, anetoderma (possibly due to elastophagocytosis) and ulceration with extrusion of keratinous debris. Multiple pilomatrixomas may be seen in patients with myotonic dystrophy, Rubinstein-Taybi syndrome and Turner syndrome. Cysts with features of pilomatrixoma are identified in patients with Gardner syndrome (J Clin Pathol 2007;60:129).
As illustrated in this case, deeper seated lesions and those arising in the head and neck region clinically mimic enlarged lymph nodes. Fine needle aspiration (FNA) may result in an erroneous interpretation of malignancy, especially in a limited sample where only one component predominates (e.g. cohesive sheets of mitotically active basaloid cells), and is a well known pitfall. A cell block preparation, which reveals the shadow cells, may be helpful in arriving at the correct diagnosis (Malays J Med Sci 2015;22:84, report of two cases).
The vast majority of pilomatrixomas are benign and do not recur following local excision. Although not necessary for diagnosis, the majority of these lesions strongly express BCL2. Activating mutations of β‐catenin may contribute to tumorigenesis in pilomatrixomas.
Features suggestive of aggressive behaviour (and likely recurrence following excision) include large size, longstanding history and budding nests infiltrating into adjacent tissues associated with desmoplasia (proliferating pilomatrixoma). True pilomatrix carcinoma is rare and shows zones of geographic necrosis, invasive growth and marked cytologic atypia associated with recurrence and lymph node metastasis. The differential diagnosis includes basal cell carcinoma (peripheral palisading, atypia, retraction artifact, typically lacks of shadow cells).
Test Question Answer:
C & D
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Week page. To subscribe or unsubscribe to Case of the Week or our other email lists, click here.
Thanks to Dr. R. F. Chinoy, Prince Aly Khan Hospital, Mumbai (India) for contributing this case and Dr. Belinda Lategan, St. Boniface Hospital Winnipeg, Manitoba (Canada) for writing the discussion. To contribute a Case of the Week, first make sure that we are currently accepting cases, then follow the guidelines on our main Case of the Week page.
Advertisement
Website news:
(1) Our request this week is for micro images relevant to NKX3-1 in normal prostate, PIN, prostatic adenocarcinoma, other. If you own images of these entities, please email them as attachments to Dr. Nat Pernick at NatPernick@gmail.com, with any corresponding clinical history. There is no payment for image contributions, but we will acknowledge you as contributor, so please indicate how you want your name to be displayed.
(2) We have now posted versions of the Jobs, Fellowships, and Conferences pages as of March 1, 2017, April 1, 2017 and May 1, 2017. We have them posted as far back as January 2012. The format is the name of the file, plus yyyymm, where yyyy is the year and mm is the month. So, for example, jobs posted as of April 1, 2016 are at http://pathologyoutlines.com/jobs201604.html.
(3) We have now posted the Jobs Report for the first quarter of 2017, click here. It is also accessible from the Jobs page by clicking on the orange link.
Visit and follow our Blog to see recent updates to the website.
Case of the Week #424
Clinical history:
A 34 year old man presented with an occipital nodule. Fine needle aspiration was performed, followed by excision.
Cytology images:
Additional cytology images:
Histopathology images:
Additional histopathology images:
What is your diagnosis?
Diagnosis:
Pilomatrixoma (pilomatricoma, calcifying epithelioma of Malherbe)
Test question (answer at the end):
Which of the following are not typical of pilomatrixoma? (choose all that are appropriate)
A. Calcification, ossification and extramedullary hematopioiesis
B. Sheets of basaloid cells, occasionally with increased mitotic activity, Shadow cells, trichilemmal-type keratinization
C. Budding nests of atypical basaloid cells associated with a desmoplastic stromal response, zonal necrosis and marked cytologic atypia
D. Recurrence following local excision
Discussion:
Pilomatixoma (pilomatricoma, calcifying epithelioma of Malherbe) is a benign skin appendigeal tumor with differentiation towards the follicular matrix. Lesions typically arise either in the head and neck or the upper extremities of children and young adults, with a second peak in incidence in individuals over 50 years old.
Histologic features are characteristic. Pilomatrixomas, often partially cystic in early lesions, contain solid nests/sheets of basaloid cells with trichilemmal-type keratinization transitioning into shadow cells, amorphous keratinous debris and foci of calcification more centrally. Additional features include ossification, extramedullary hematopoiesis and foreign body type inflammatory response. Variants may demonstrate pigmentation, anetoderma (possibly due to elastophagocytosis) and ulceration with extrusion of keratinous debris. Multiple pilomatrixomas may be seen in patients with myotonic dystrophy, Rubinstein-Taybi syndrome and Turner syndrome. Cysts with features of pilomatrixoma are identified in patients with Gardner syndrome (J Clin Pathol 2007;60:129).
As illustrated in this case, deeper seated lesions and those arising in the head and neck region clinically mimic enlarged lymph nodes. Fine needle aspiration (FNA) may result in an erroneous interpretation of malignancy, especially in a limited sample where only one component predominates (e.g. cohesive sheets of mitotically active basaloid cells), and is a well known pitfall. A cell block preparation, which reveals the shadow cells, may be helpful in arriving at the correct diagnosis (Malays J Med Sci 2015;22:84, report of two cases).
The vast majority of pilomatrixomas are benign and do not recur following local excision. Although not necessary for diagnosis, the majority of these lesions strongly express BCL2. Activating mutations of β‐catenin may contribute to tumorigenesis in pilomatrixomas.
Features suggestive of aggressive behaviour (and likely recurrence following excision) include large size, longstanding history and budding nests infiltrating into adjacent tissues associated with desmoplasia (proliferating pilomatrixoma). True pilomatrix carcinoma is rare and shows zones of geographic necrosis, invasive growth and marked cytologic atypia associated with recurrence and lymph node metastasis. The differential diagnosis includes basal cell carcinoma (peripheral palisading, atypia, retraction artifact, typically lacks of shadow cells).
Test Question Answer:
C & D