9 December 2015 - Case of the Week #373
All cases are archived on our website. To view them sorted by number, diagnosis or category, visit our Home Page and click on the Case of the Week button. To subscribe or unsubscribe to the Case of the Week or our other email lists, click here.
Thanks to Dr. Cristina Aguilar, The Guthrie Clinic, Pennsylvania (USA) for contributing this case. To contribute a Case of the Week, follow the guidelines on our Case of the Week page.
Advertisement
Website news:
(1) The staff at PathologyOutlines.com wish you Happy Holidays and a Happy New Year!
(2) If you will be doing any online shopping this holiday season, please remember to use our Amazon link. Anything purchased (books, clothes, household items, toys, etc.) helps support PathologyOutlines.com by earning us a small commission on each purchase, with no extra cost to you! Please bookmark this link to your browser. Thank you for your support!
(3) Our Feature page for December is Grossing Equipment / Workstations, and highlights our advertisers EXAKT Technologies, Inc., Milestone Medical, MOPEC and Photodyne Technologies. It also contains an original short article, "Pathology Workstations: Frozen Section Safety", by Jaleh Mansouri, M.D.
Note: All future Feature pages will now be combined with the Buyer's Guide. You can access previous Feature pages by visiting the Past / Future Feature Pages section at the bottom of the Feature page.
Visit our Blog and Subscribe to our Posts or Follow by Email (click on the box on the right side) to see recent updates to the website.
Case of the Week #373
Clinical history:
A 61 year old man presented with a left brain mass, which was resected by craniotomy. The surgeon believed the mass arose from the dura.
Micro images:
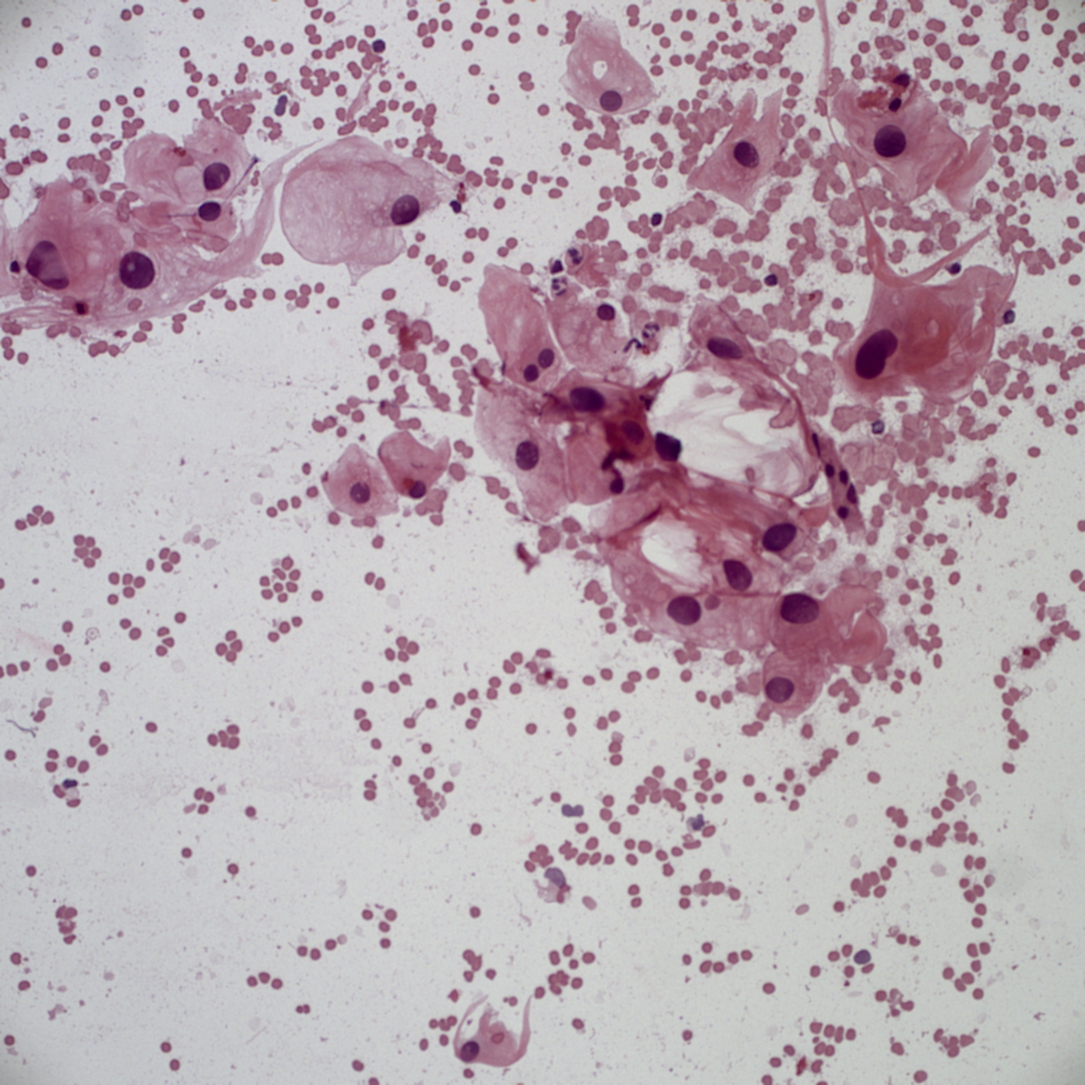
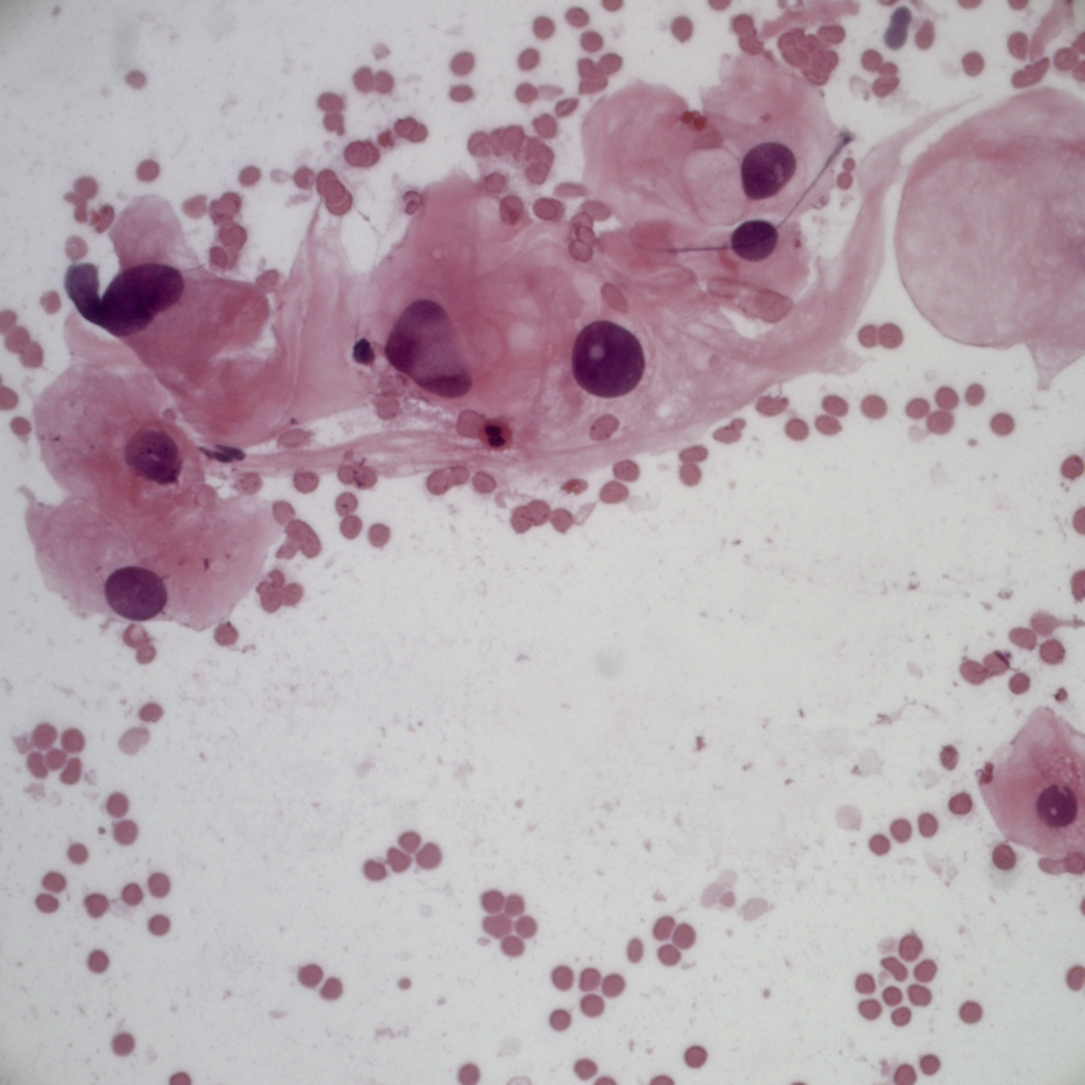
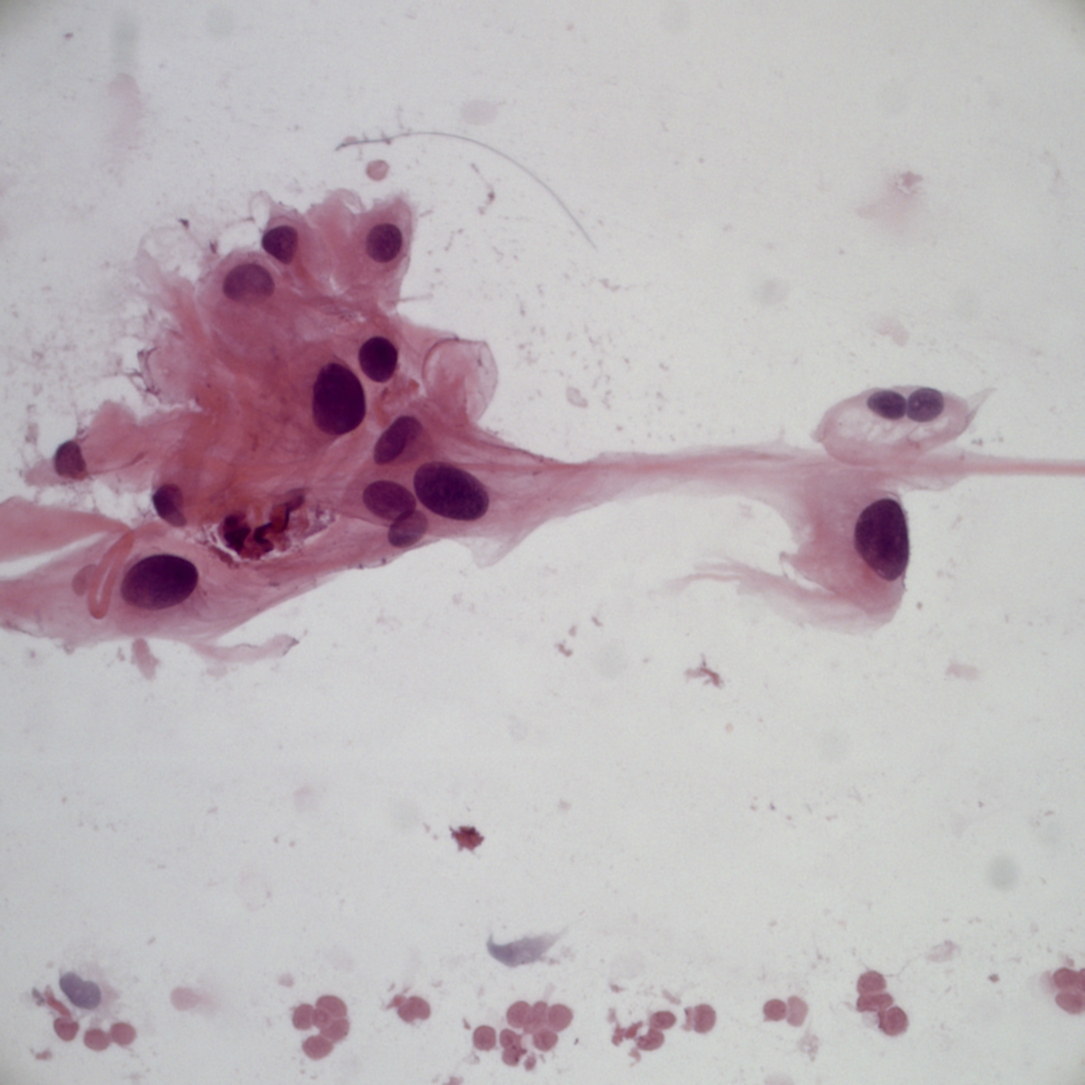
Smears:
Additional smears:
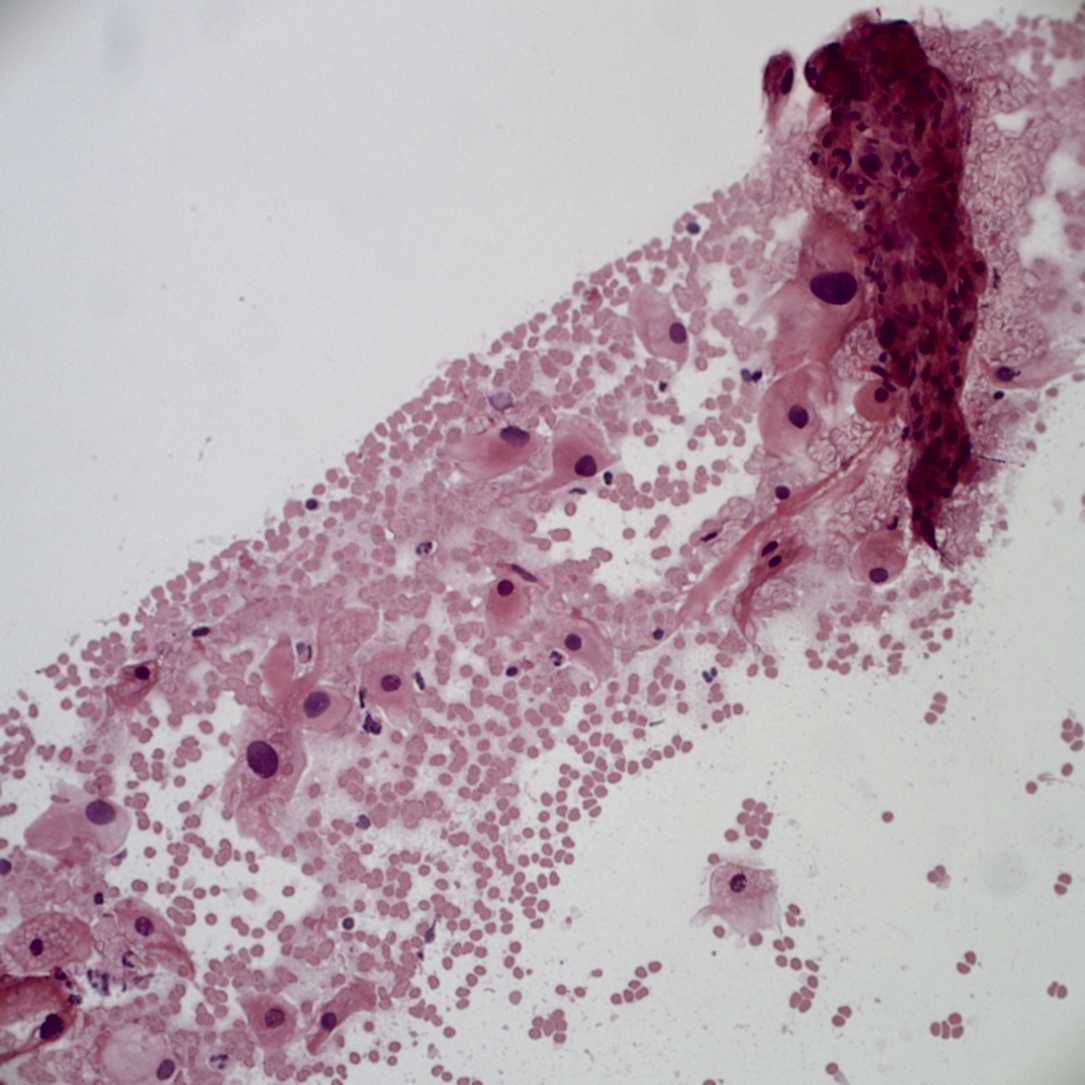
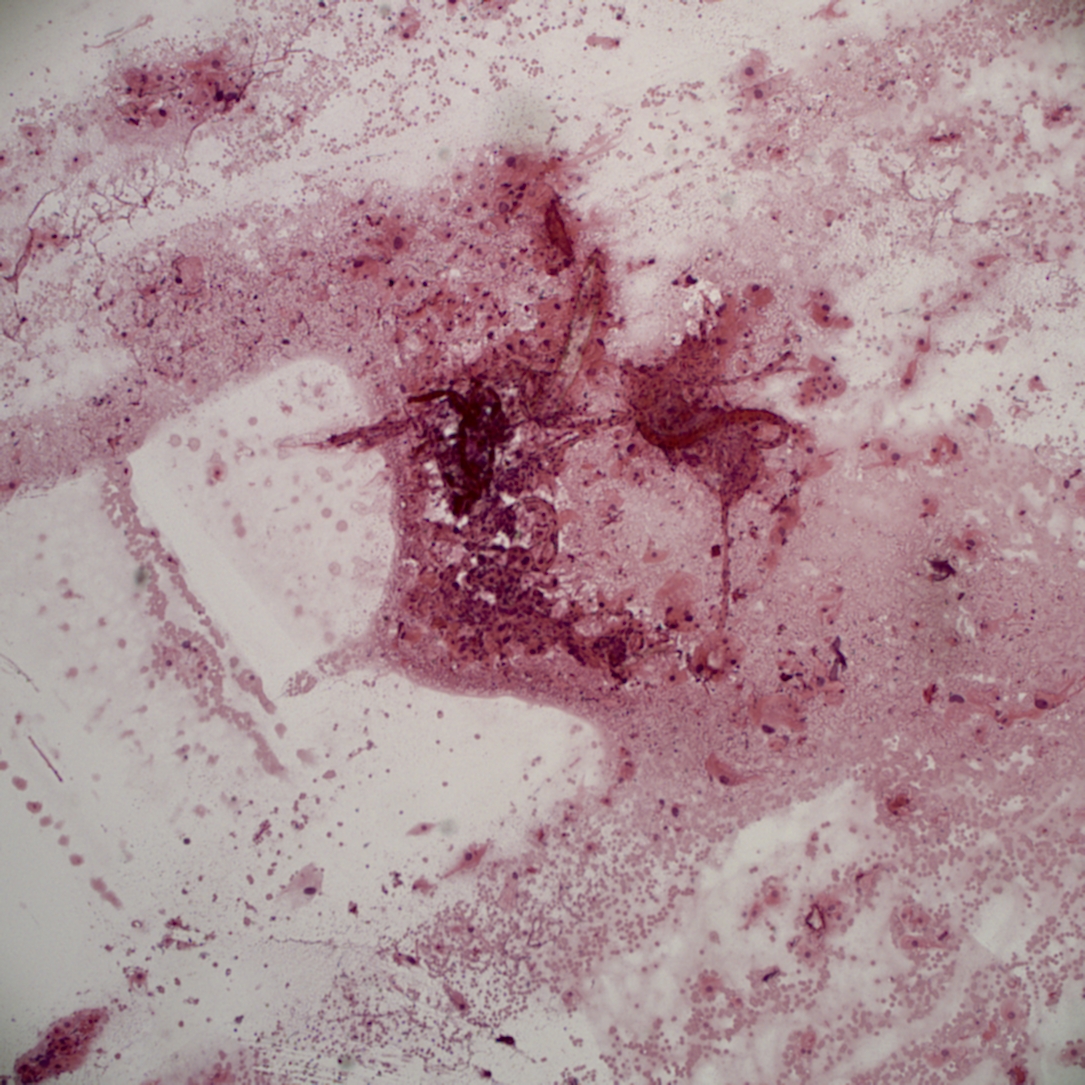
Frozen section:
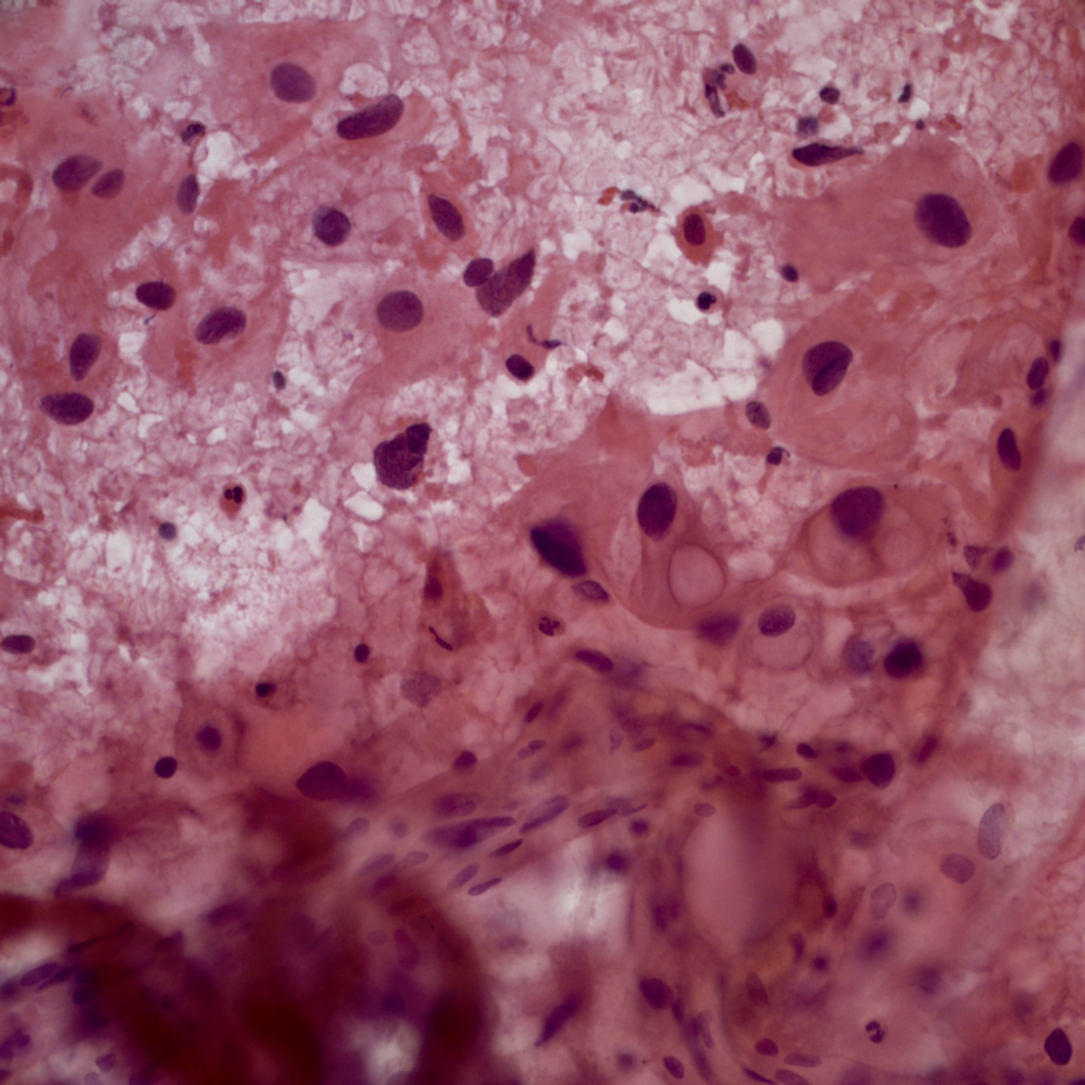
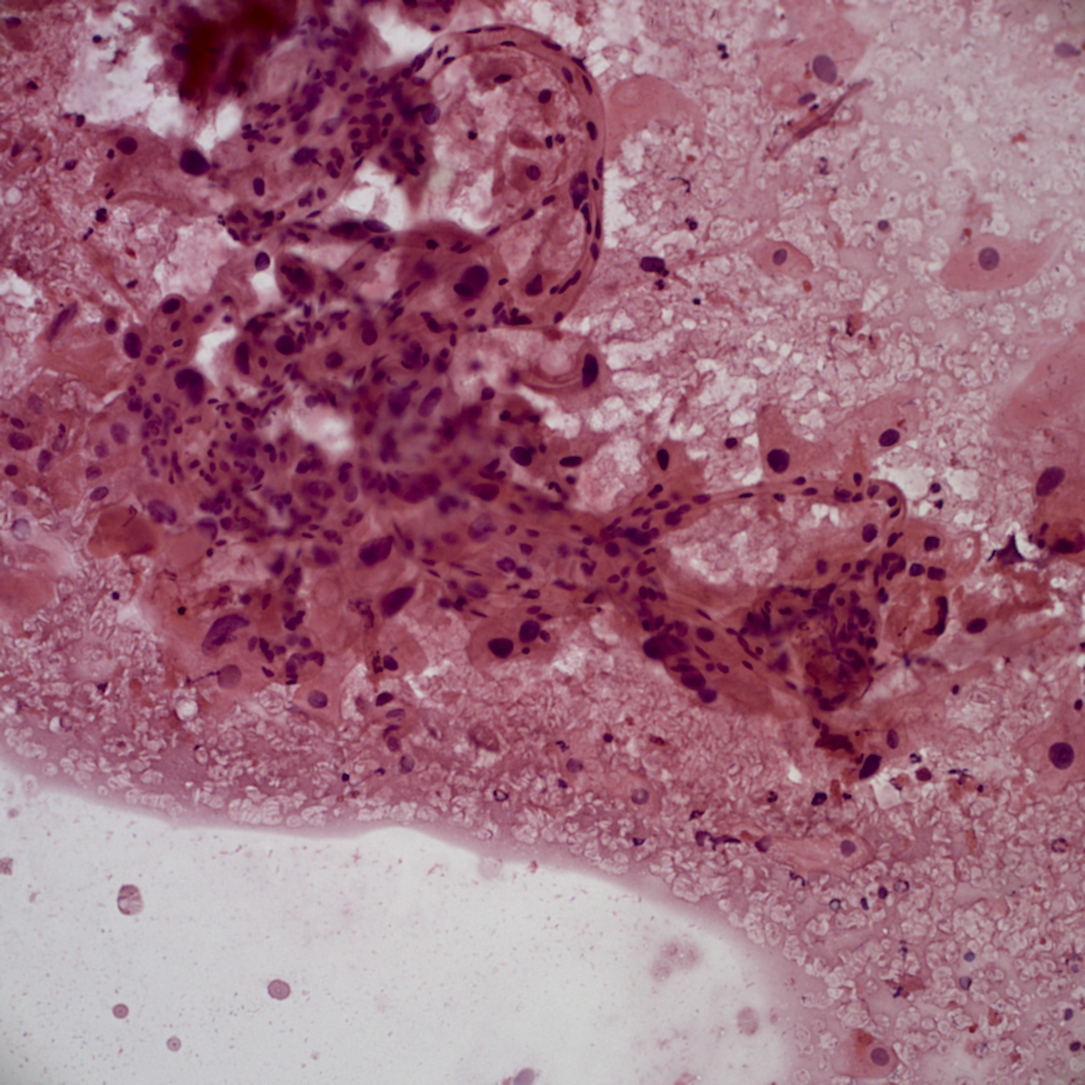
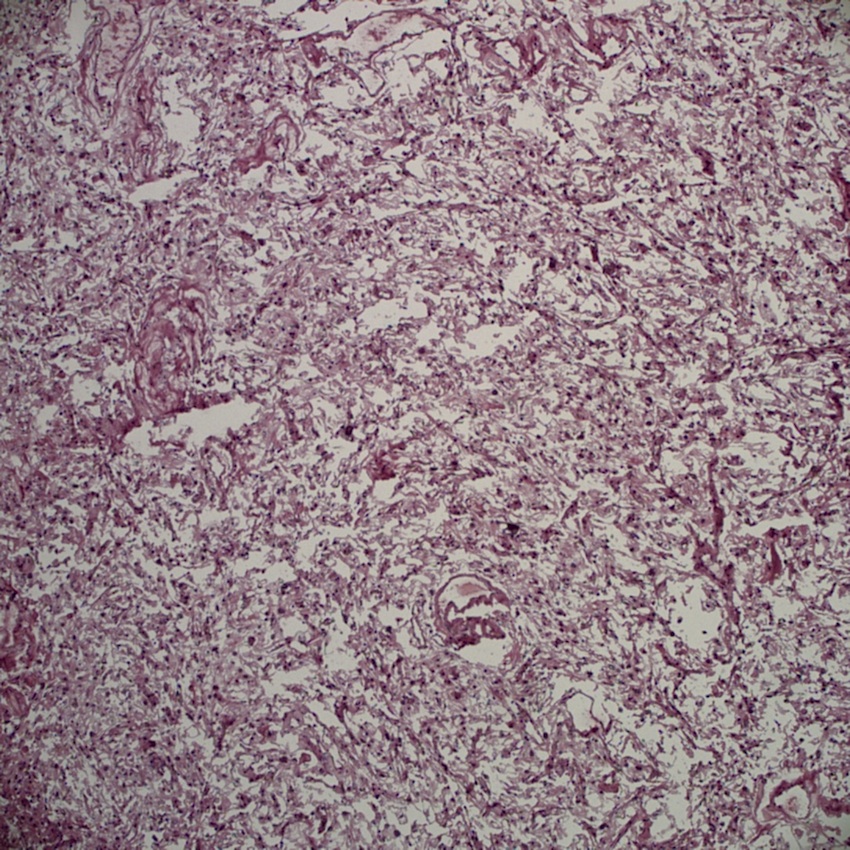
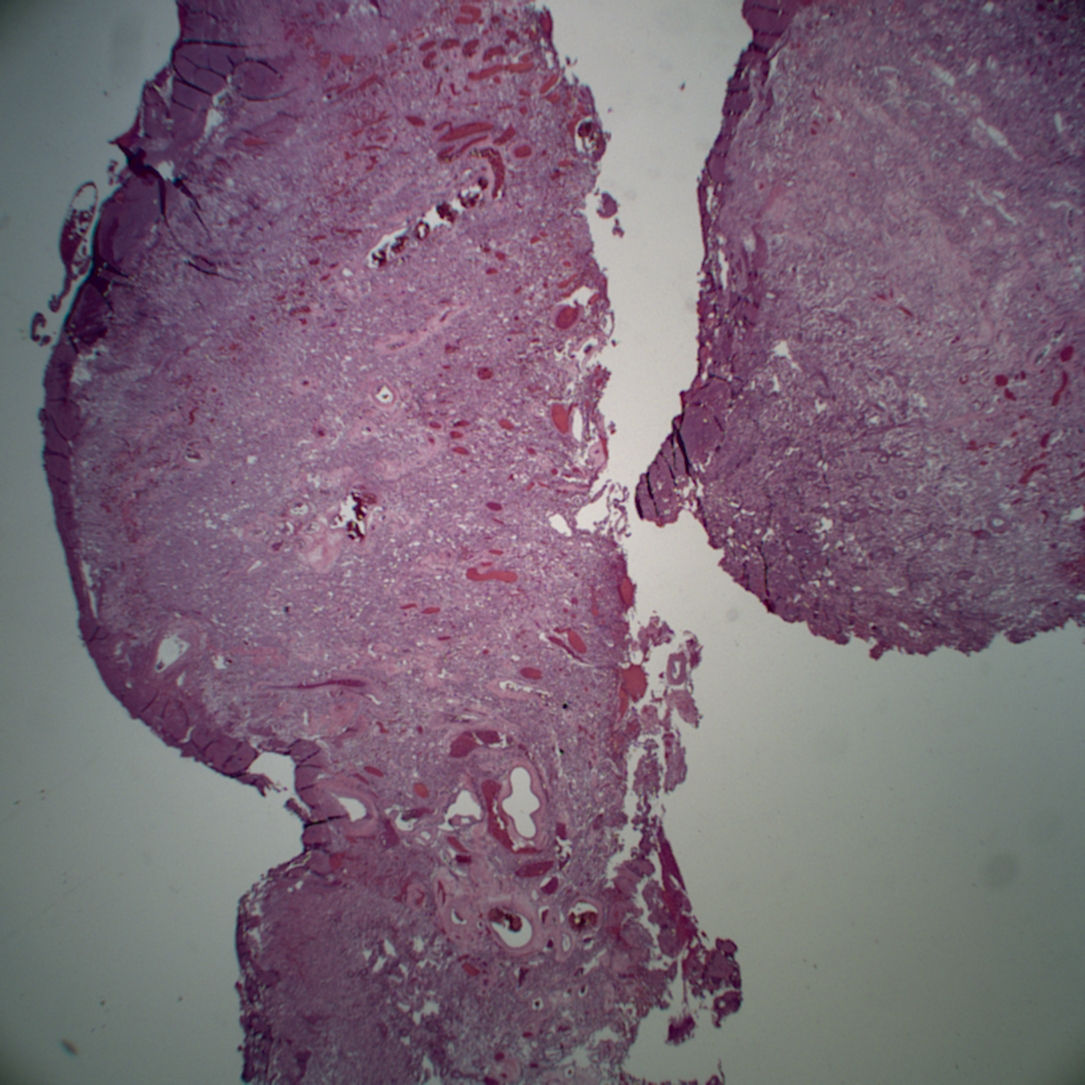
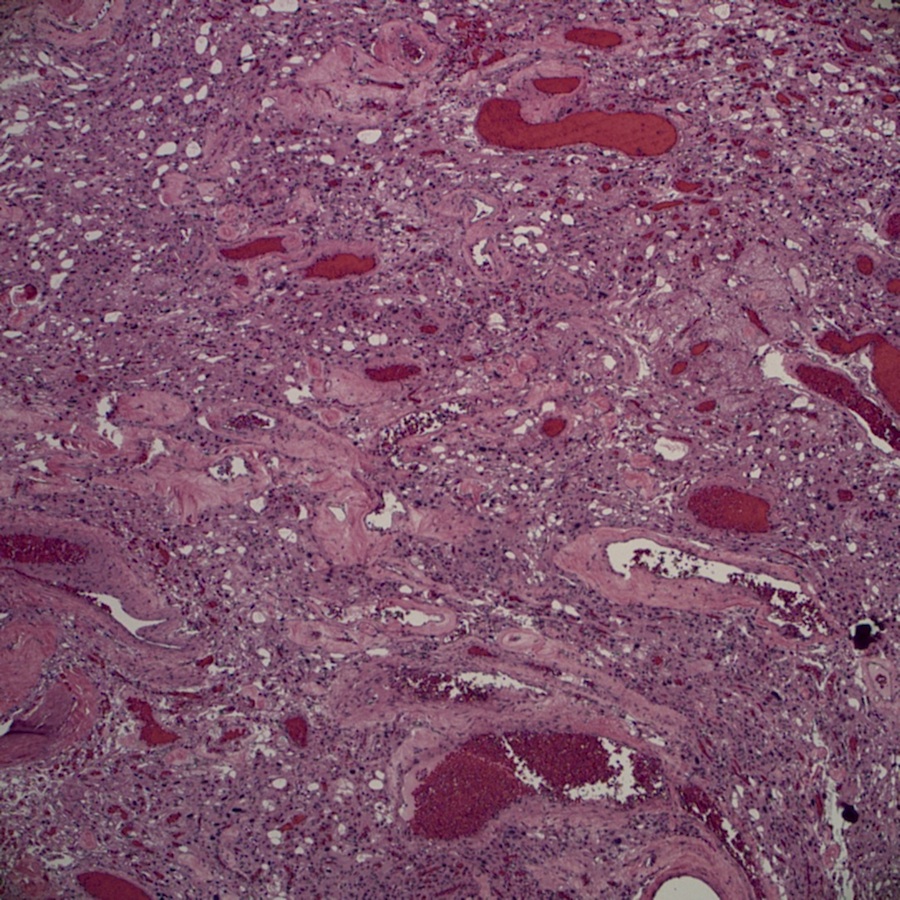
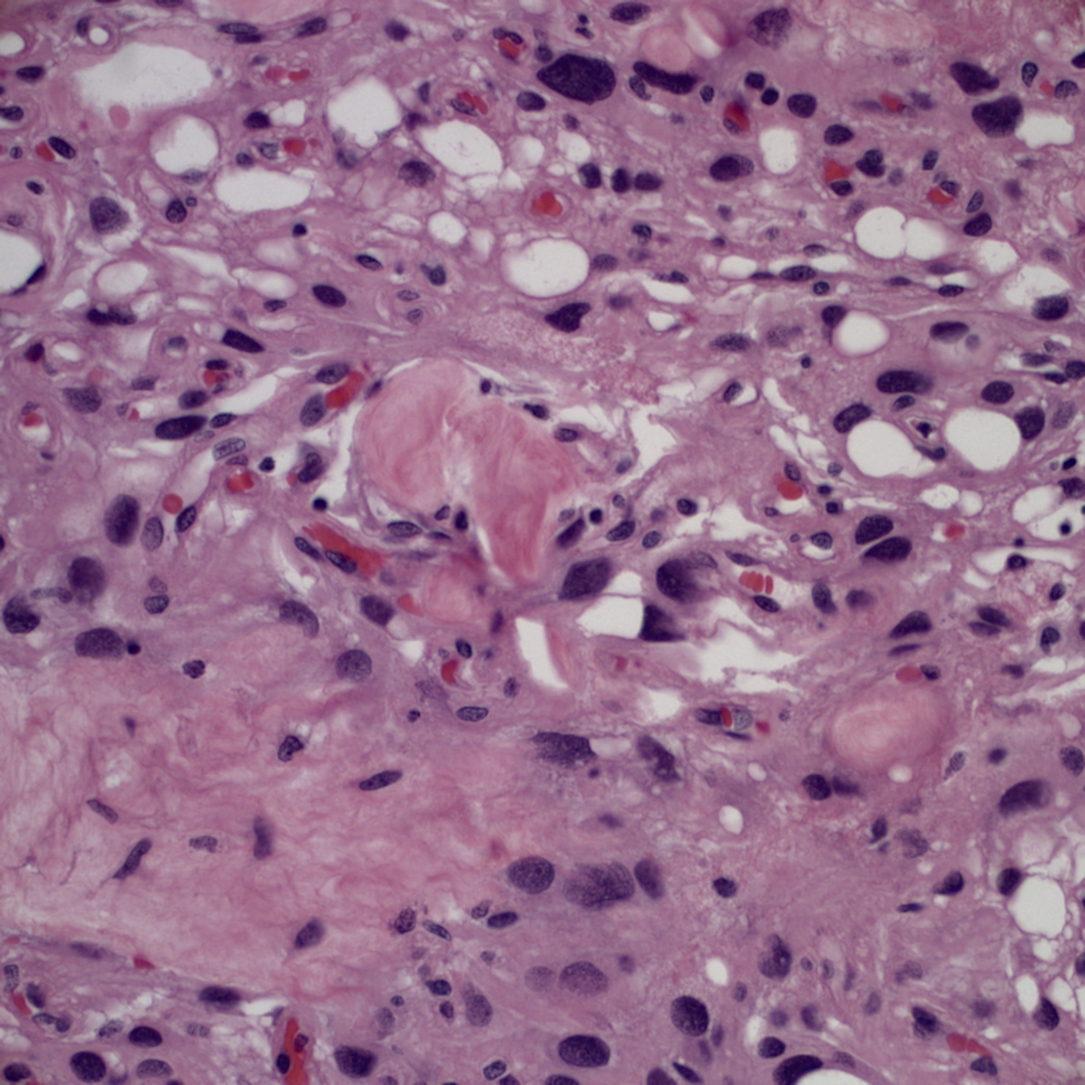
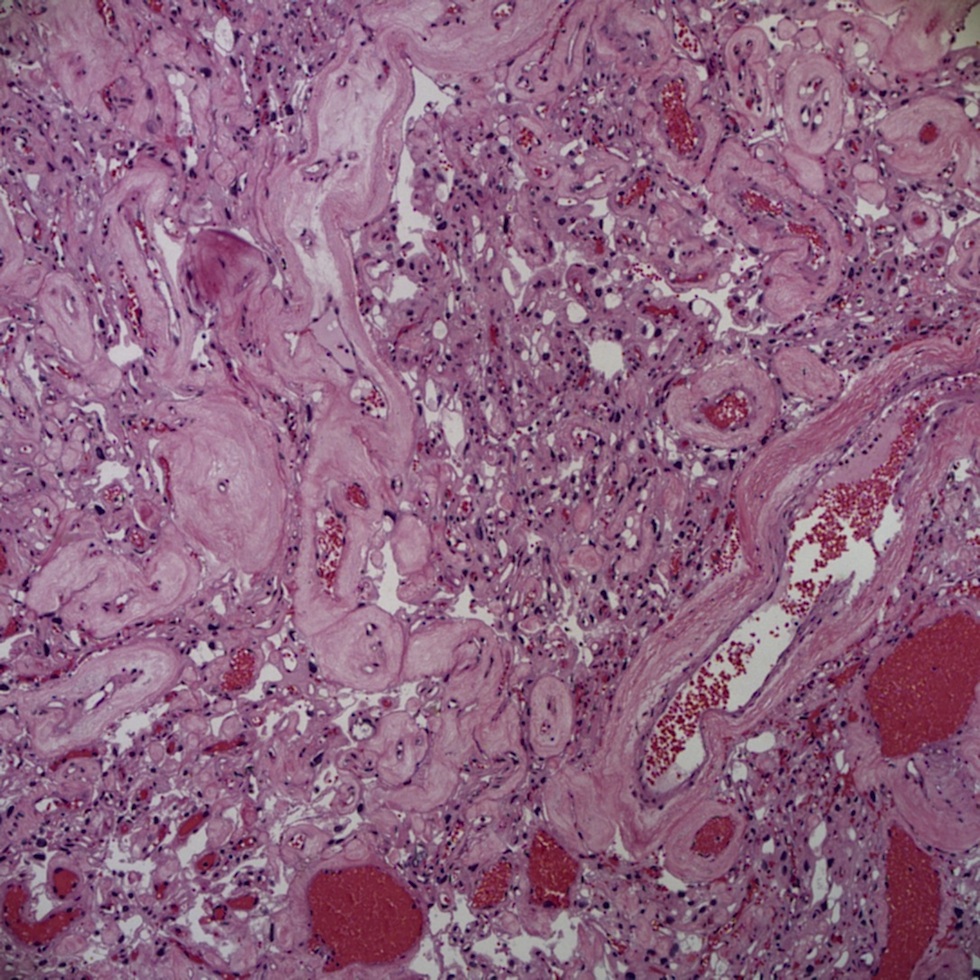
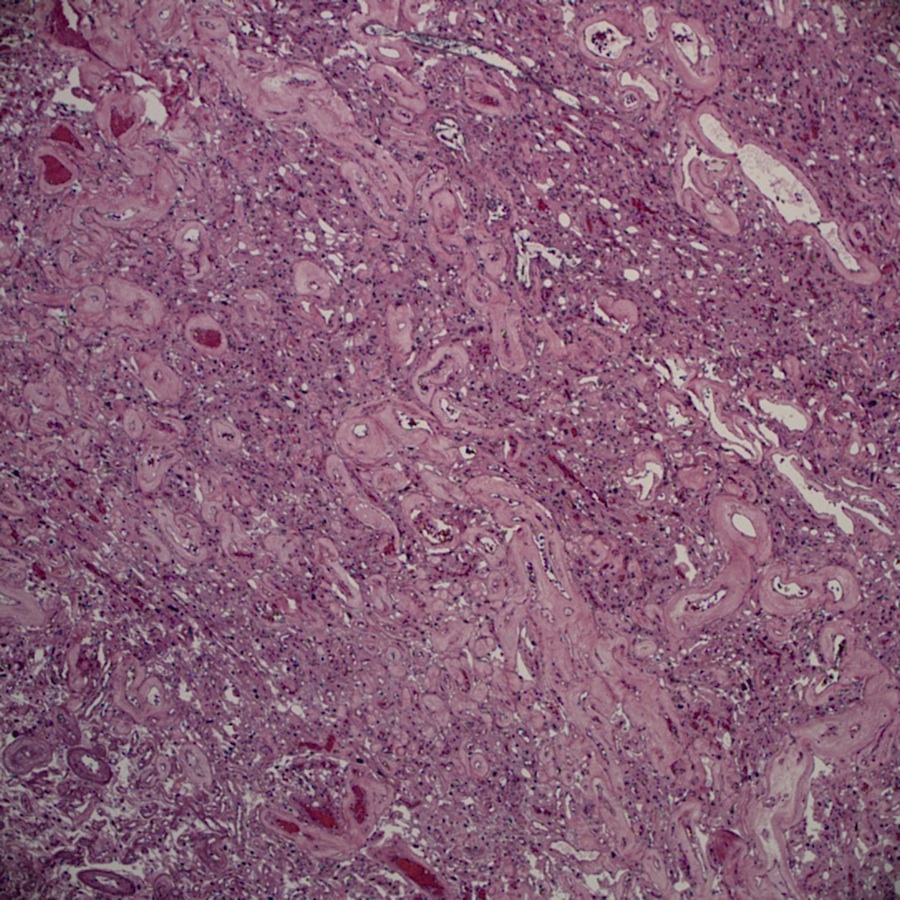
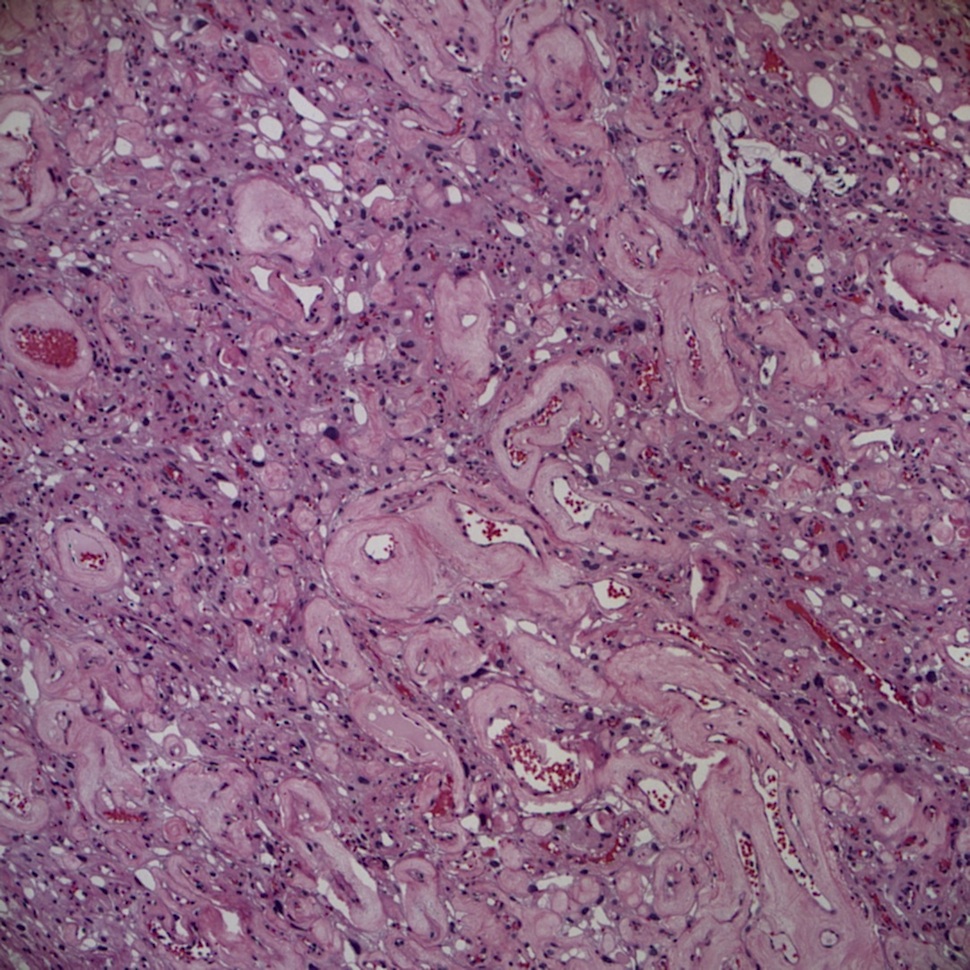
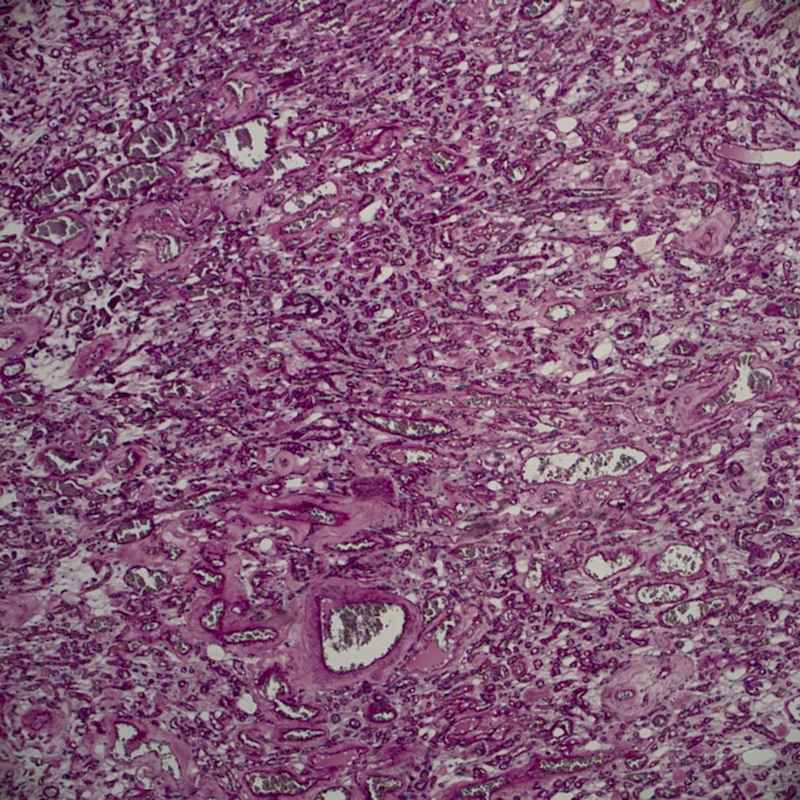
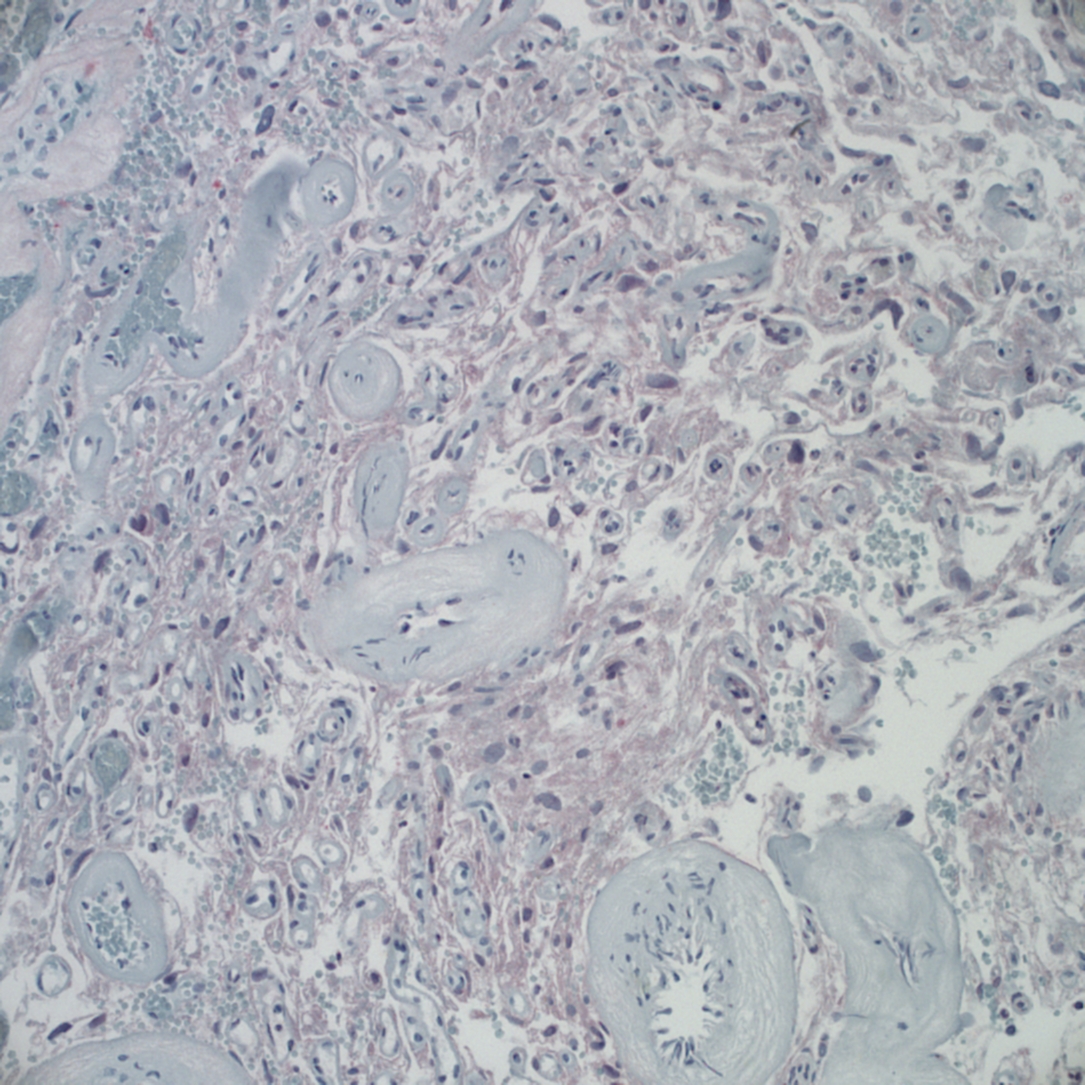
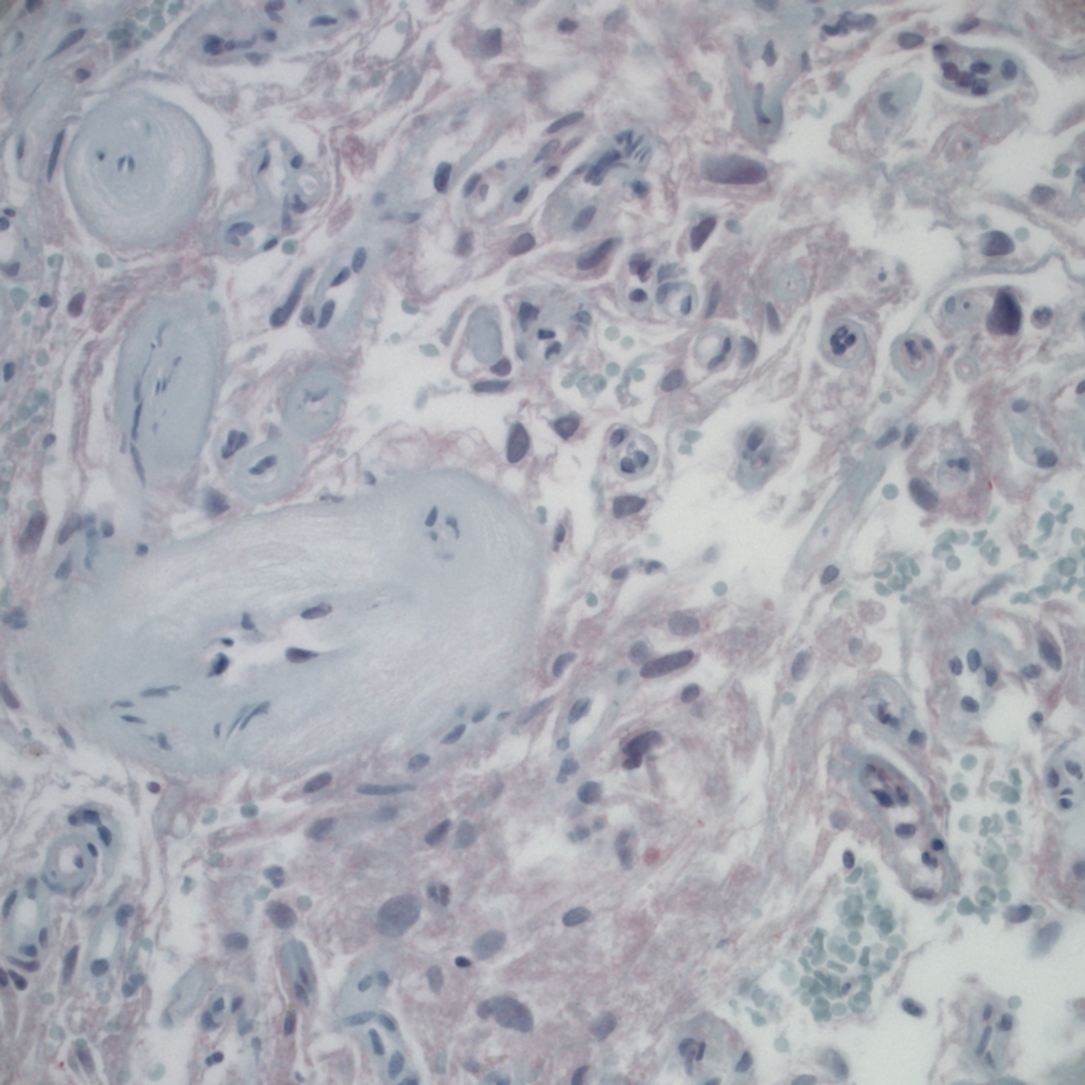
H&E images:
Additional H&E images:
What is your diagnosis?
Diagnosis:
Angiomatous meningioma, WHO grade I
Necrosis associated with angioembolic material (elsewhere)
Discussion:
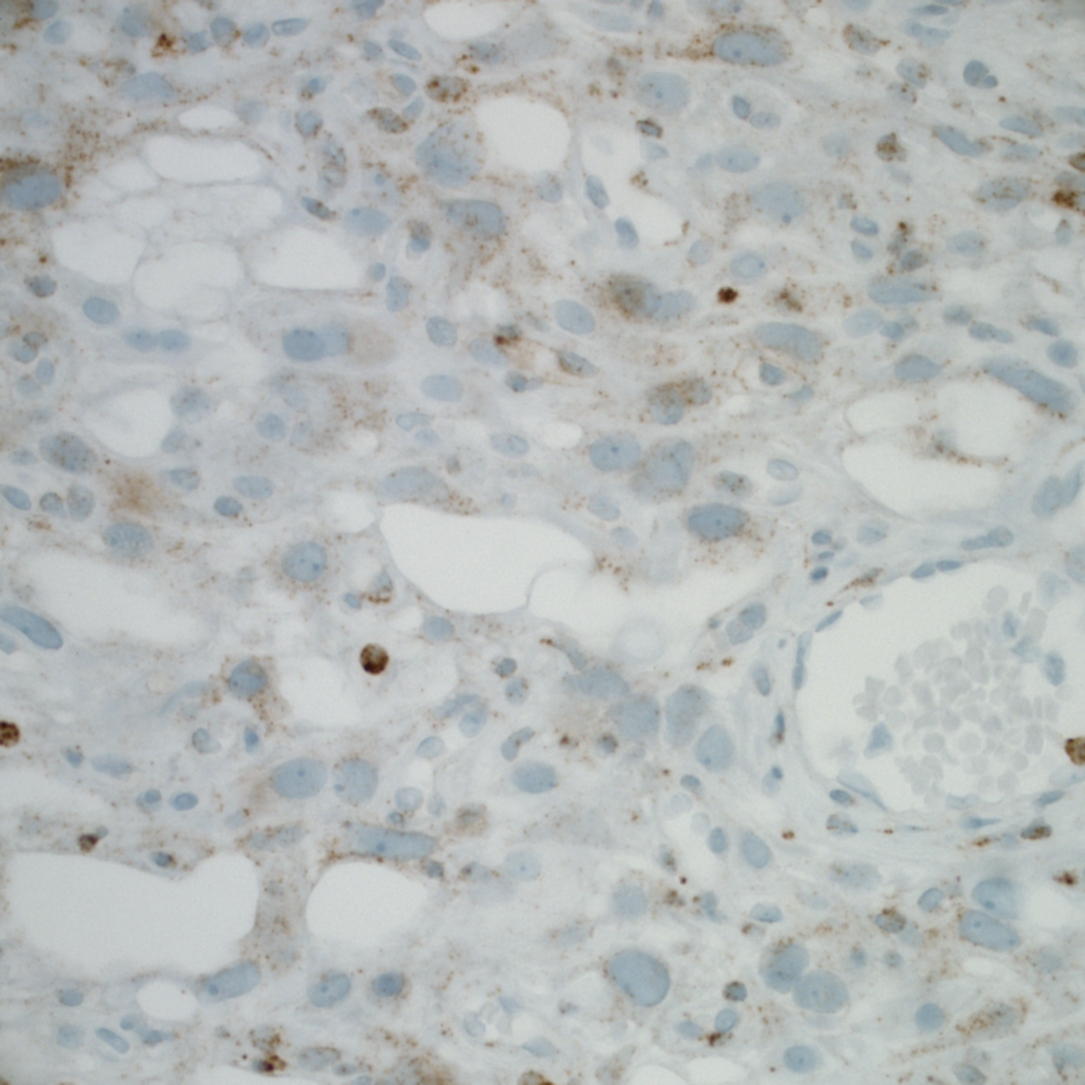
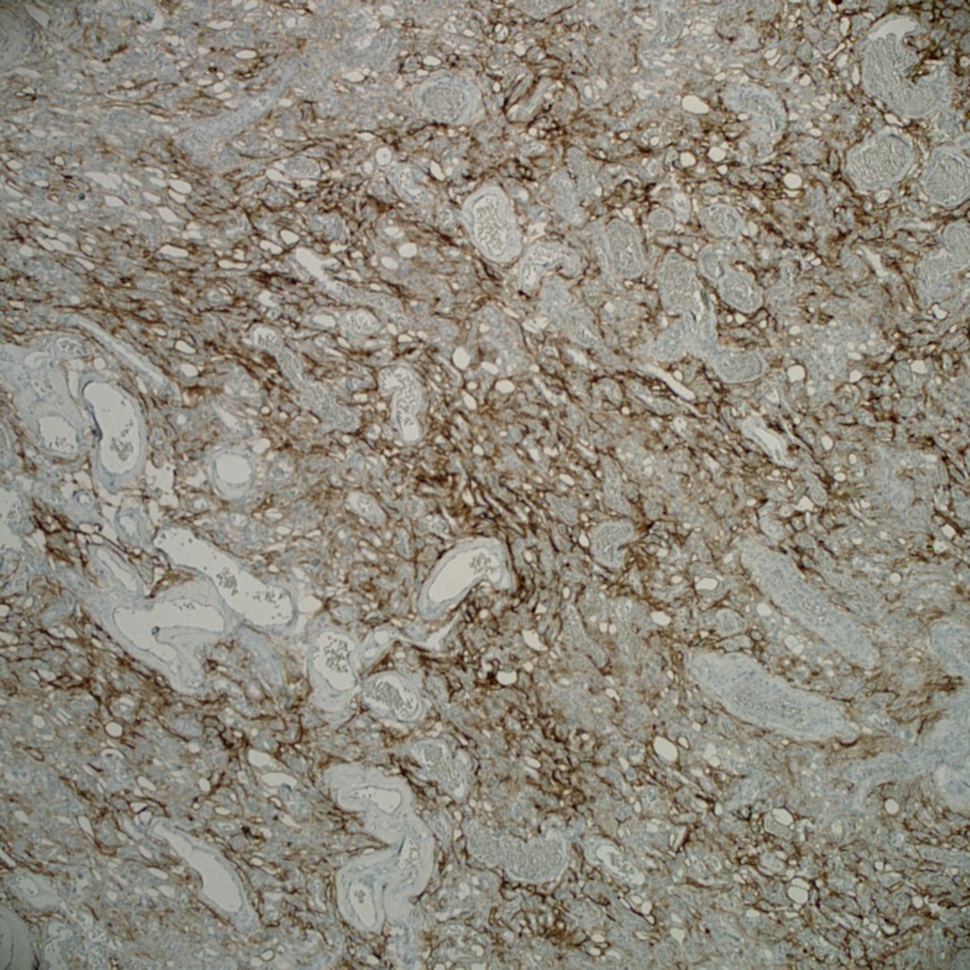
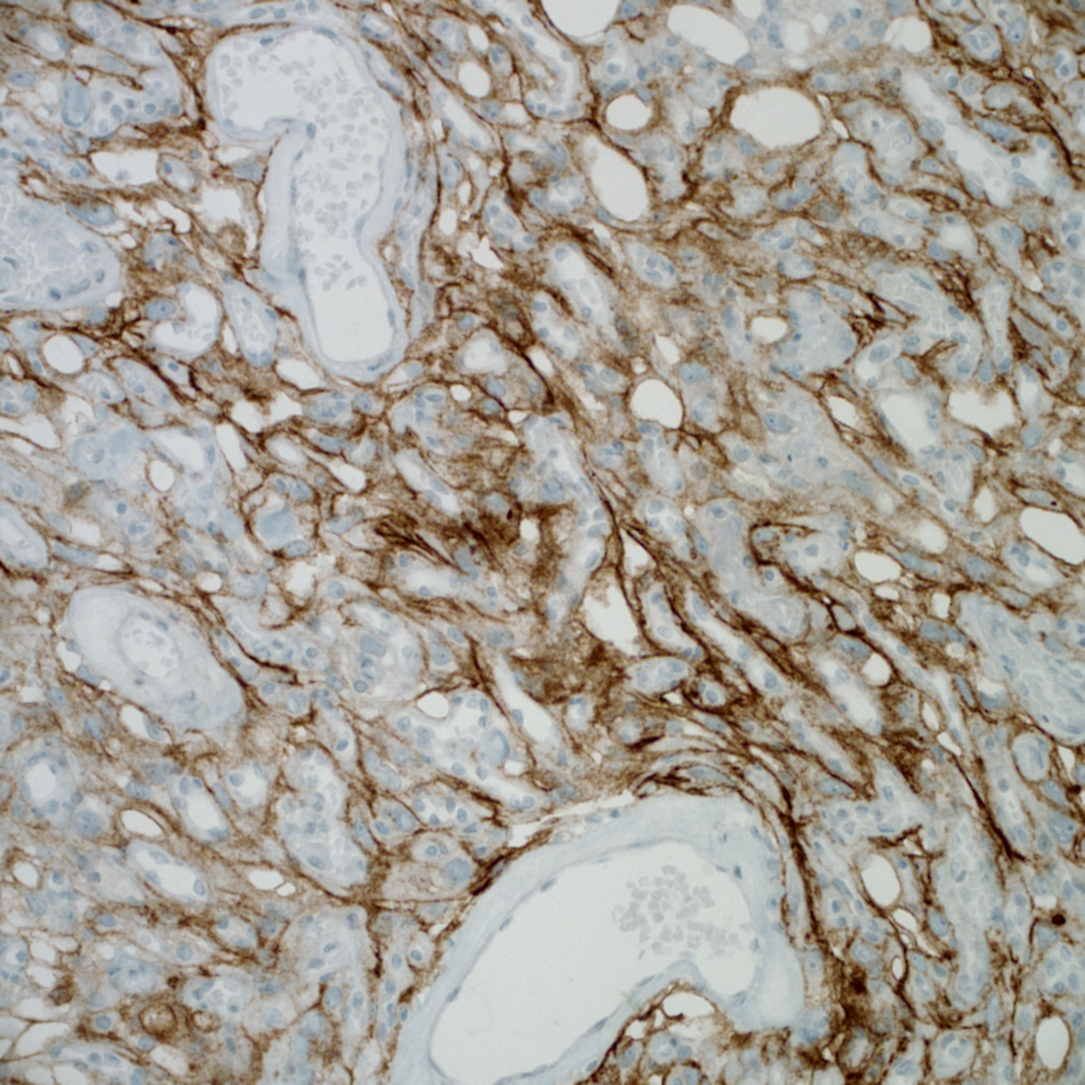
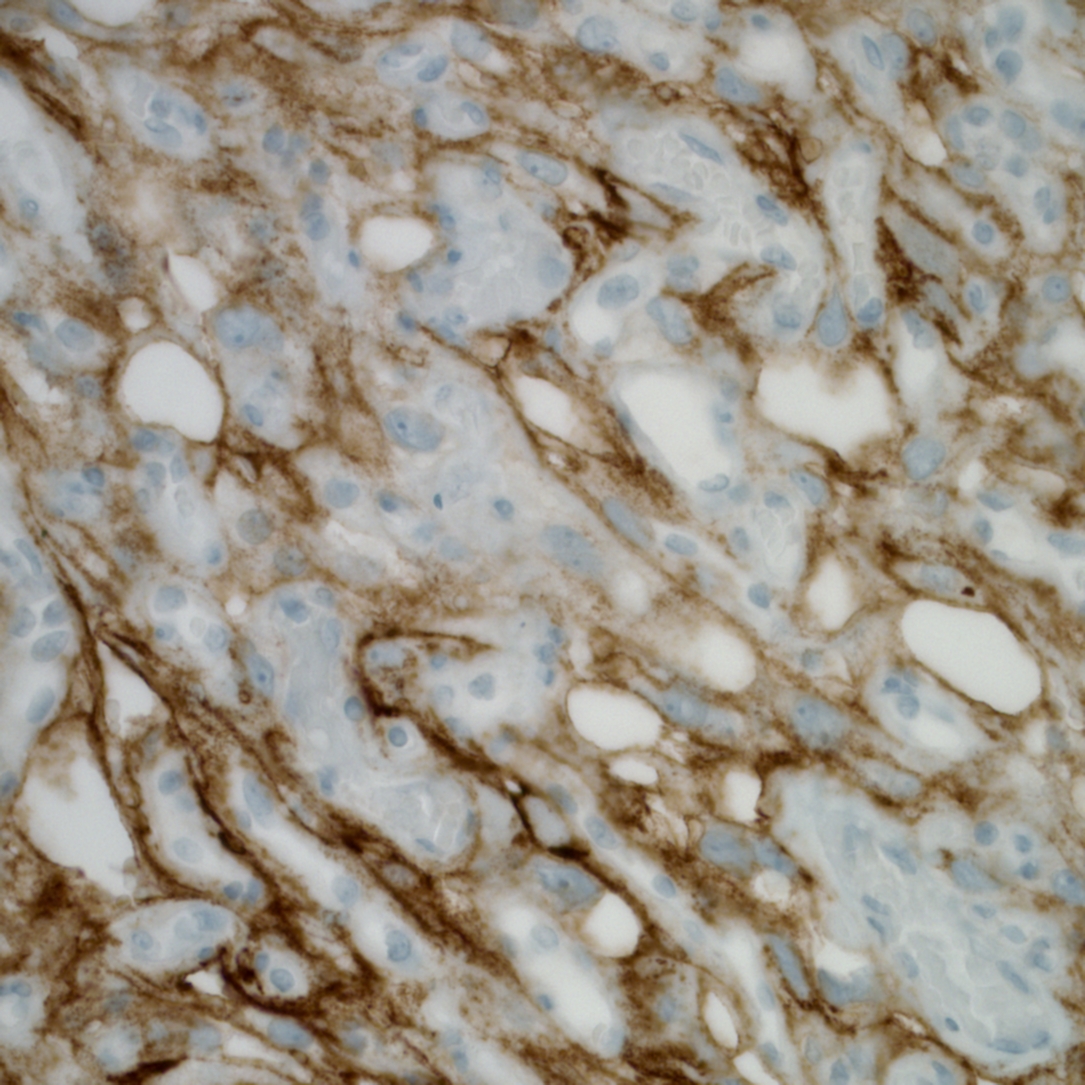
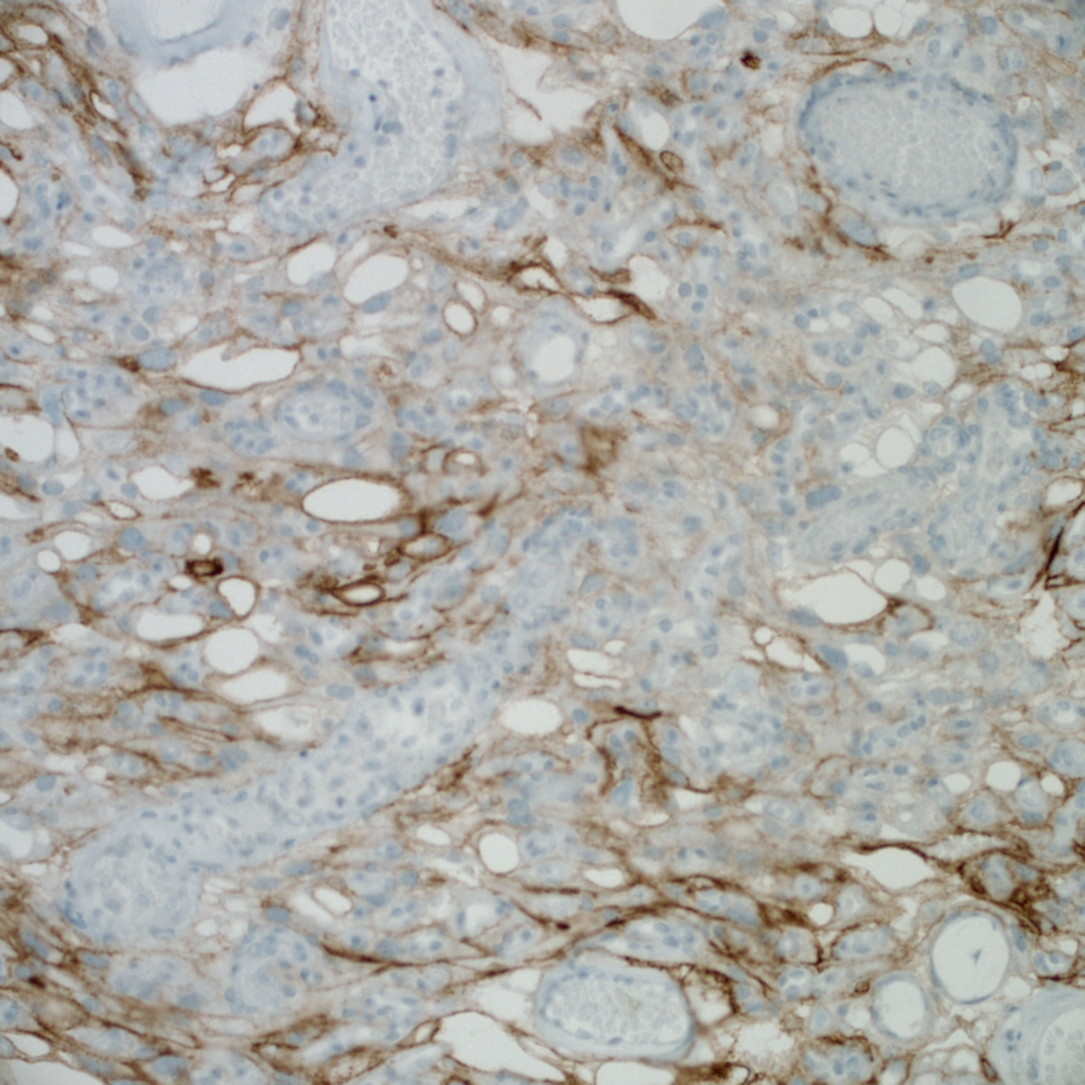
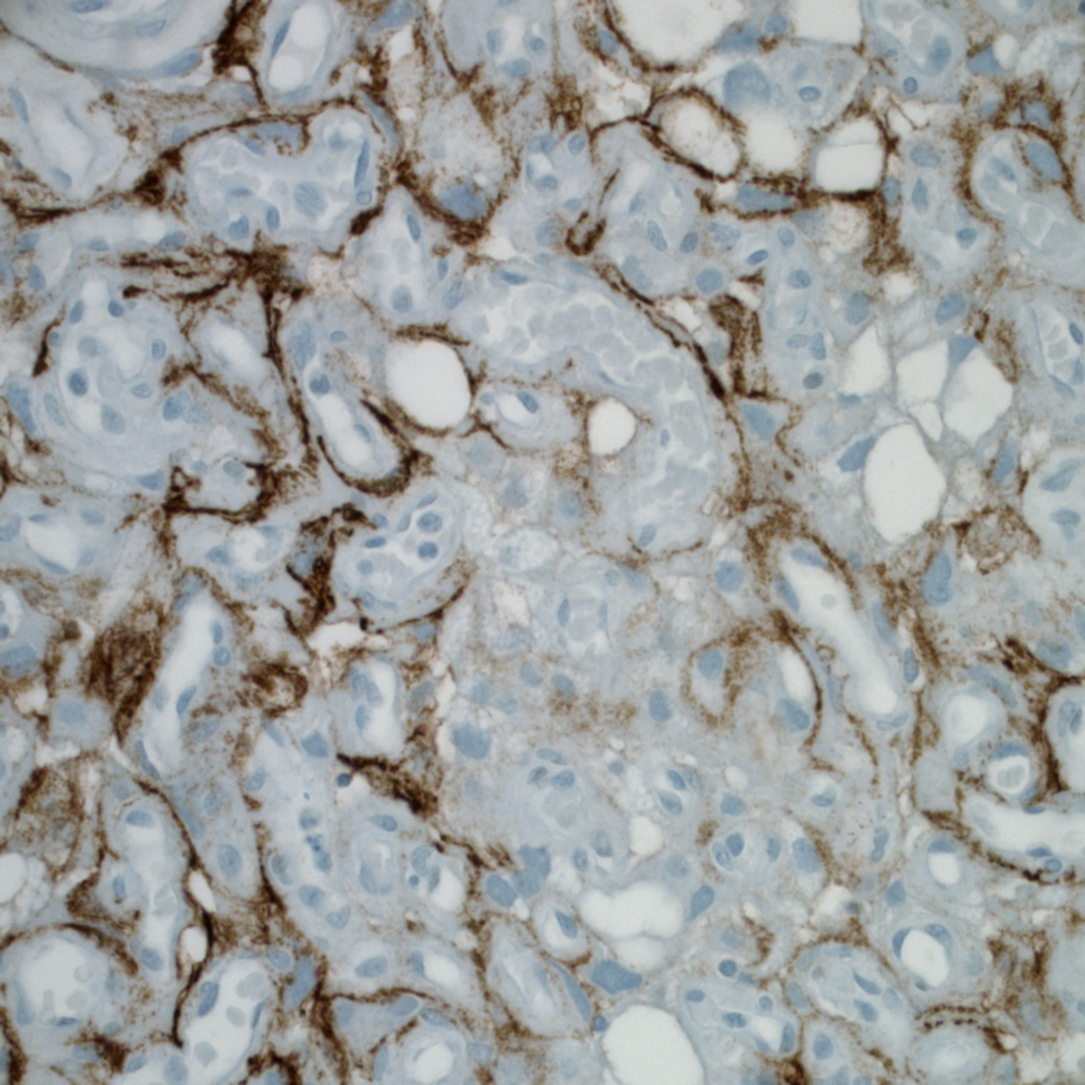
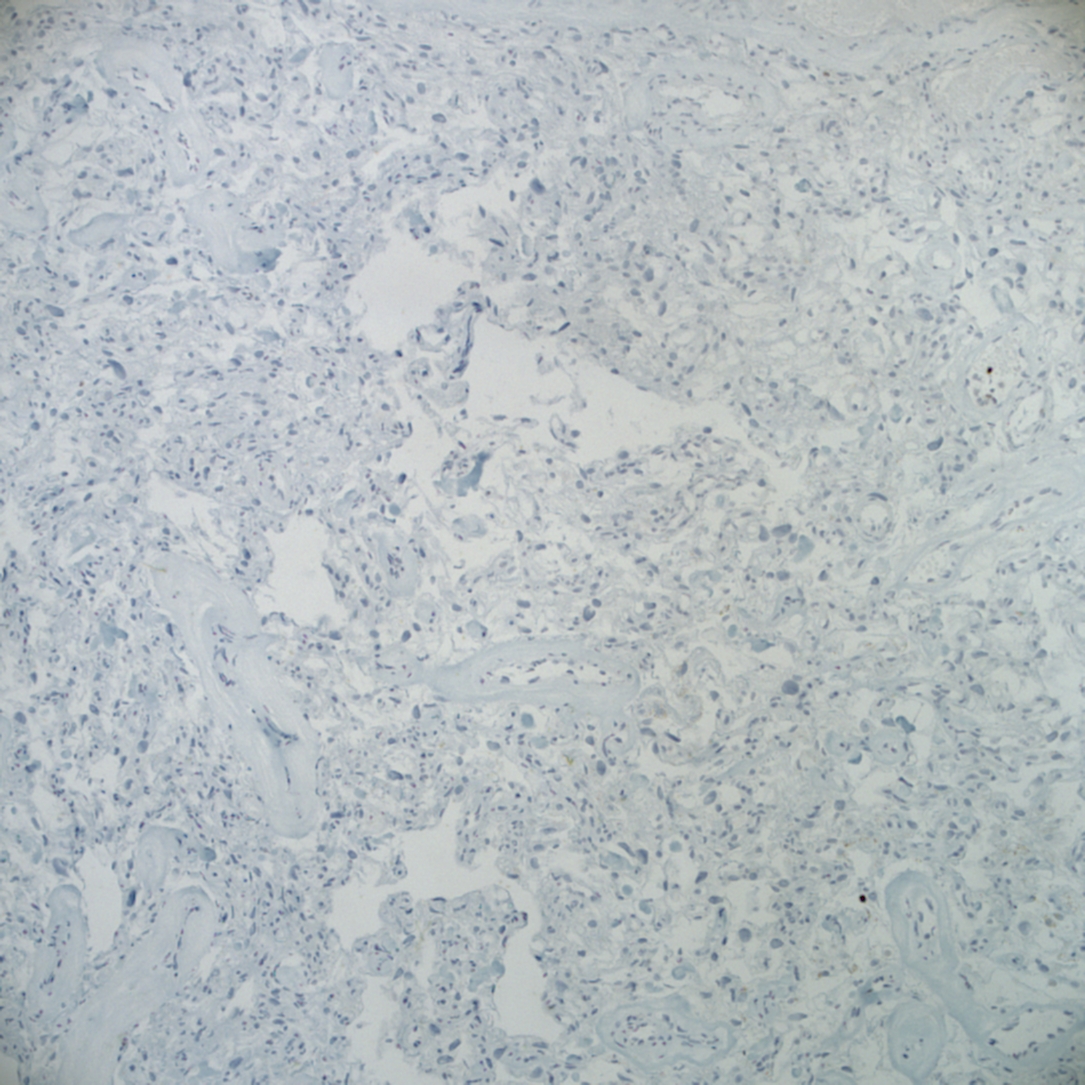
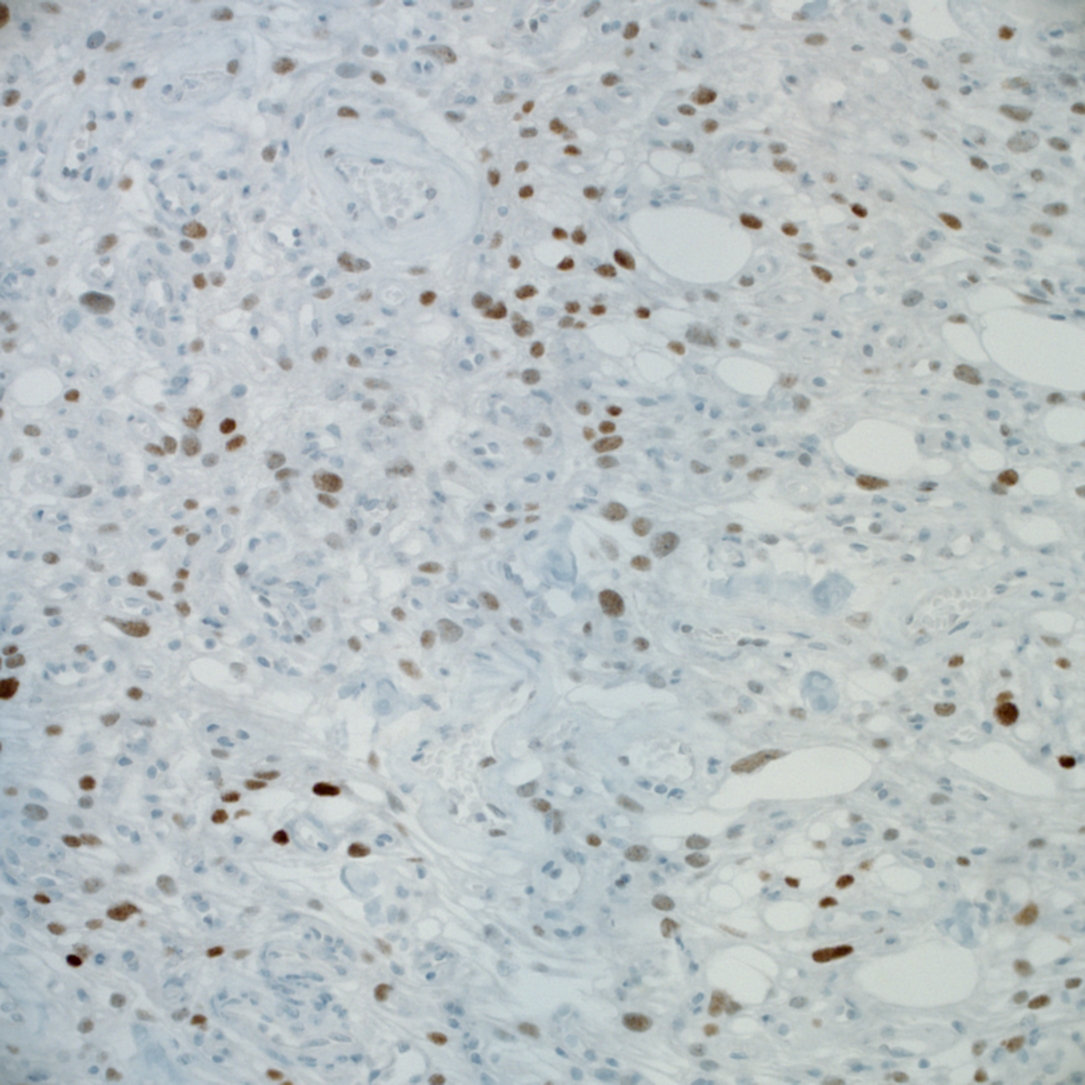
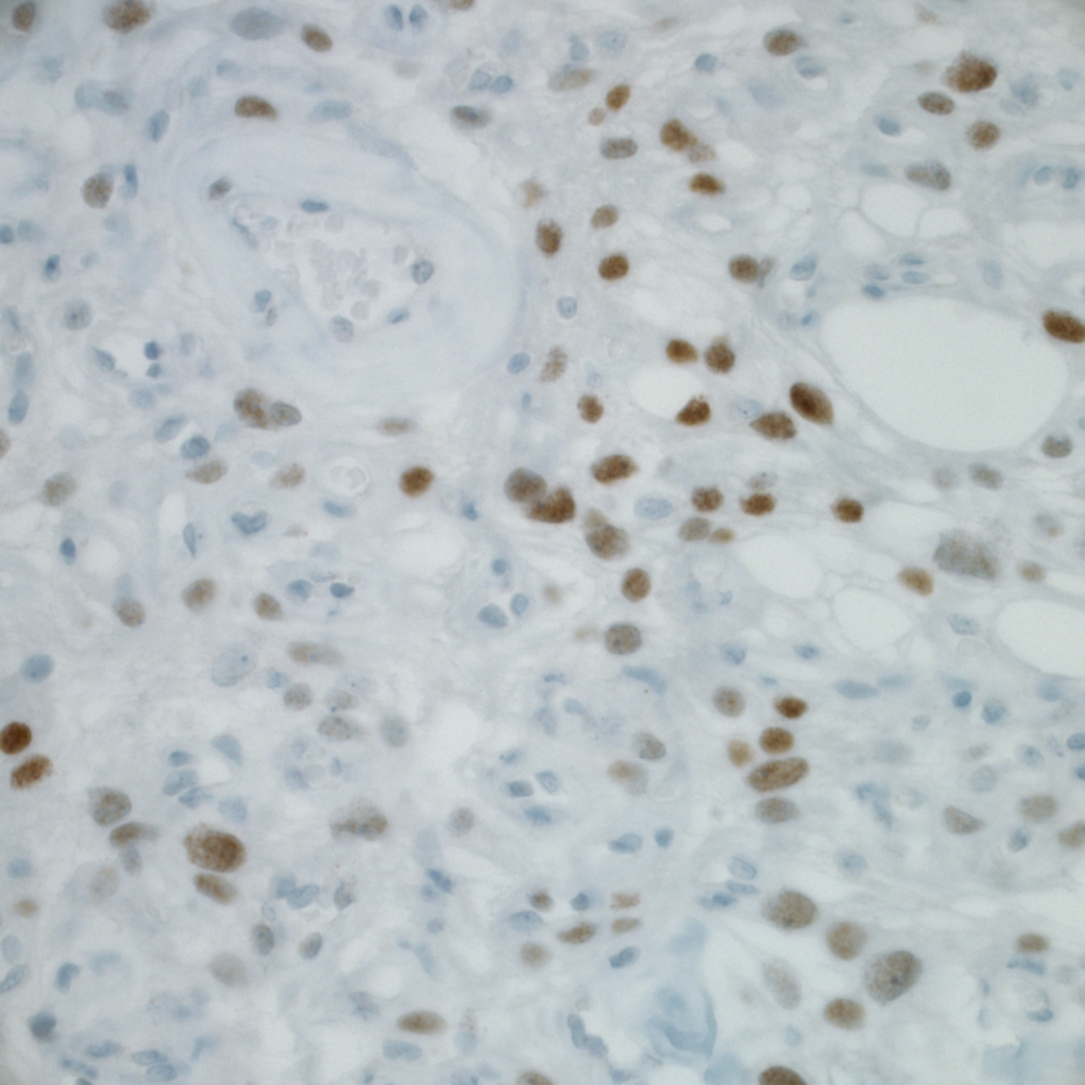
Immunostains were obtained:
Meningiomas are neoplasms which originate from meningothelial cells. Most arise within the cranial cavity and are dura based. They may occur in childhood or adolescence, but are more commonly encountered in middle or later adult life. Females are more commonly affected, and there has been evidence that their growth is subject to hormonal influence (Rosai and Ackerman's Surgical Pathology, 2011). Angiomatous meningioma, constituting roughly 2% of meningiomas, is a rare histological variant of meningioma whose vascular component exceeds 50% of the total tumor area (Int J Clin Exp Pathol 2013;6:695, Am J Surg Pathol 2004;28:390). Compared to conventional meningioma, it has a high male to female ratio and more frequent peritumoral edema (Int J Clin Exp Pathol 2013;6:695).
On gross examination, meningiomas are solid and lobulated, and broadly anchored to the dura mater.
On histology, angiomatous meningioma features abundant blood vessels with at least focal classic meningothelial differentiation (syncytial cells with indistinct cell membranes and eosinophilic cytoplasm, intranuclear pseudoinclusions and a lobulated architecture with meningothelial "whorls"). Immunostains are strongly positive for EMA / MUC1 and S100. BCL2 is negative in tumor cells and only a focal area of tumor cells stain positive for p63. Both E-cadherin and N-CAM show light focal staining. CD34 and PASD highlight the dense vascularity present in the tumor. Ki-67 proliferation is ~1%.
The WHO / Mayo Clinic criteria stratifies meningothelial tumors into meningioma (WHO grade I), atypical meningioma (WHO grade II) and anaplastic meningioma (WHO grade III), based on features such as mitotic activity, cellular density, growth pattern, atypical cellular features (macronucleoli, high N:C ratio) and presence of necrosis (Rosai and Ackerman's Surgical Pathology, 2011). The present case showed no atypical features, and is thus classified as WHO grade I.
The differential diagnosis might include hemangioblastoma and hemangiopericytoma, especially if interpreting a small fragment of tissue from, for example, an intraoperative consultation (Indian J Pathol Microbiol 2008;51:53). Immunohistochemistry can be helpful in equivocal cases, with EMA, CK and progesterone positivity confirming a diagnosis of meningioma. Hemangioblastoma would express inhibin and NSE.
The prognosis is favorable, similar to other types of WHO I meningiomas, and gross total resection is the treatment of choice. Patients with residual tumor after surgery can benefit from radiation therapy (Int J Clin Exp Pathol 2013;6:695, Am J Surg Pathol 2004;28:390).
Discussion by Dr. Jennifer R. Kaley, University of Arkansas for Medical Sciences (USA).
All cases are archived on our website. To view them sorted by number, diagnosis or category, visit our Home Page and click on the Case of the Week button. To subscribe or unsubscribe to the Case of the Week or our other email lists, click here.
Thanks to Dr. Cristina Aguilar, The Guthrie Clinic, Pennsylvania (USA) for contributing this case. To contribute a Case of the Week, follow the guidelines on our Case of the Week page.
All New CME Course

A Review of Diagnostic Liver Pathology: Evolving Concepts and Clinical Implications
February 22-25, 2016
Mauna Lani Bay Hotel, Big Island of Hawaii
Register Now!
Website news:
(1) The staff at PathologyOutlines.com wish you Happy Holidays and a Happy New Year!
(2) If you will be doing any online shopping this holiday season, please remember to use our Amazon link. Anything purchased (books, clothes, household items, toys, etc.) helps support PathologyOutlines.com by earning us a small commission on each purchase, with no extra cost to you! Please bookmark this link to your browser. Thank you for your support!
(3) Our Feature page for December is Grossing Equipment / Workstations, and highlights our advertisers EXAKT Technologies, Inc., Milestone Medical, MOPEC and Photodyne Technologies. It also contains an original short article, "Pathology Workstations: Frozen Section Safety", by Jaleh Mansouri, M.D.
Note: All future Feature pages will now be combined with the Buyer's Guide. You can access previous Feature pages by visiting the Past / Future Feature Pages section at the bottom of the Feature page.
Visit our Blog and Subscribe to our Posts or Follow by Email (click on the box on the right side) to see recent updates to the website.
Case of the Week #373
Clinical history:
A 61 year old man presented with a left brain mass, which was resected by craniotomy. The surgeon believed the mass arose from the dura.
Micro images:
Smears:
Additional smears:
Frozen section:
H&E images:
Additional H&E images:
What is your diagnosis?
Diagnosis:
Angiomatous meningioma, WHO grade I
Necrosis associated with angioembolic material (elsewhere)
Discussion:
Immunostains were obtained:
Meningiomas are neoplasms which originate from meningothelial cells. Most arise within the cranial cavity and are dura based. They may occur in childhood or adolescence, but are more commonly encountered in middle or later adult life. Females are more commonly affected, and there has been evidence that their growth is subject to hormonal influence (Rosai and Ackerman's Surgical Pathology, 2011). Angiomatous meningioma, constituting roughly 2% of meningiomas, is a rare histological variant of meningioma whose vascular component exceeds 50% of the total tumor area (Int J Clin Exp Pathol 2013;6:695, Am J Surg Pathol 2004;28:390). Compared to conventional meningioma, it has a high male to female ratio and more frequent peritumoral edema (Int J Clin Exp Pathol 2013;6:695).
On gross examination, meningiomas are solid and lobulated, and broadly anchored to the dura mater.
On histology, angiomatous meningioma features abundant blood vessels with at least focal classic meningothelial differentiation (syncytial cells with indistinct cell membranes and eosinophilic cytoplasm, intranuclear pseudoinclusions and a lobulated architecture with meningothelial "whorls"). Immunostains are strongly positive for EMA / MUC1 and S100. BCL2 is negative in tumor cells and only a focal area of tumor cells stain positive for p63. Both E-cadherin and N-CAM show light focal staining. CD34 and PASD highlight the dense vascularity present in the tumor. Ki-67 proliferation is ~1%.
The WHO / Mayo Clinic criteria stratifies meningothelial tumors into meningioma (WHO grade I), atypical meningioma (WHO grade II) and anaplastic meningioma (WHO grade III), based on features such as mitotic activity, cellular density, growth pattern, atypical cellular features (macronucleoli, high N:C ratio) and presence of necrosis (Rosai and Ackerman's Surgical Pathology, 2011). The present case showed no atypical features, and is thus classified as WHO grade I.
The differential diagnosis might include hemangioblastoma and hemangiopericytoma, especially if interpreting a small fragment of tissue from, for example, an intraoperative consultation (Indian J Pathol Microbiol 2008;51:53). Immunohistochemistry can be helpful in equivocal cases, with EMA, CK and progesterone positivity confirming a diagnosis of meningioma. Hemangioblastoma would express inhibin and NSE.
The prognosis is favorable, similar to other types of WHO I meningiomas, and gross total resection is the treatment of choice. Patients with residual tumor after surgery can benefit from radiation therapy (Int J Clin Exp Pathol 2013;6:695, Am J Surg Pathol 2004;28:390).
Discussion by Dr. Jennifer R. Kaley, University of Arkansas for Medical Sciences (USA).