13 May 2015 - Case #352
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Ankur Sangoi, El Camino Hospital, California (USA), for contributing this case and part of the discussion. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Advertisement
Case #352
Clinical history:
The pathologist received a morcellated myomectomy specimen from a 38 year old woman with leiomyomas.
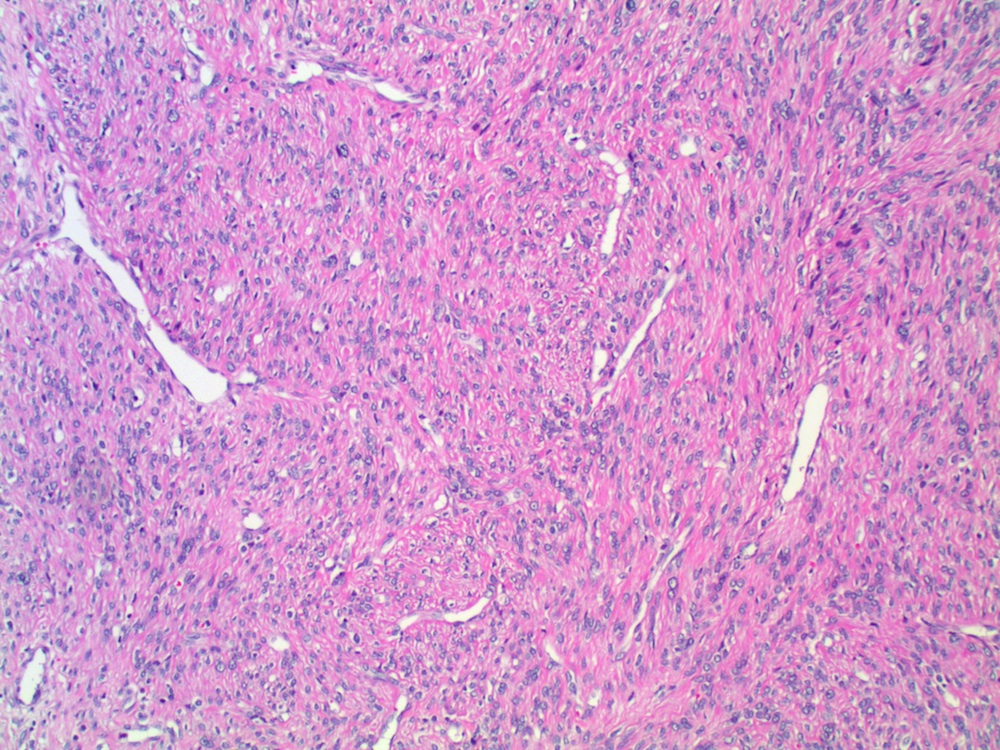
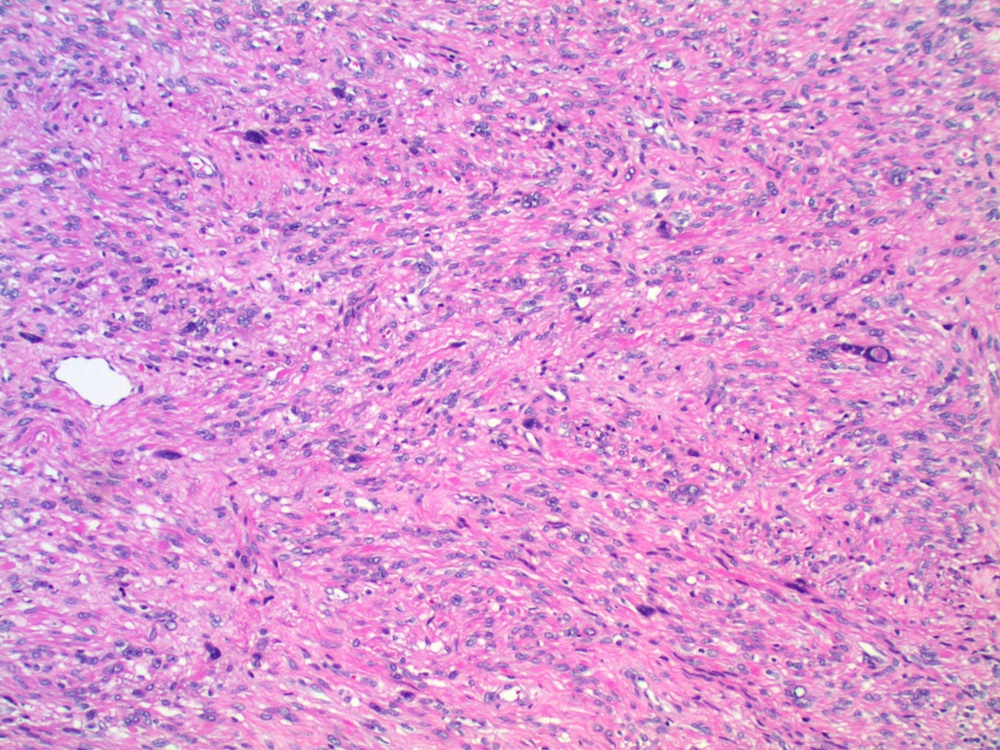
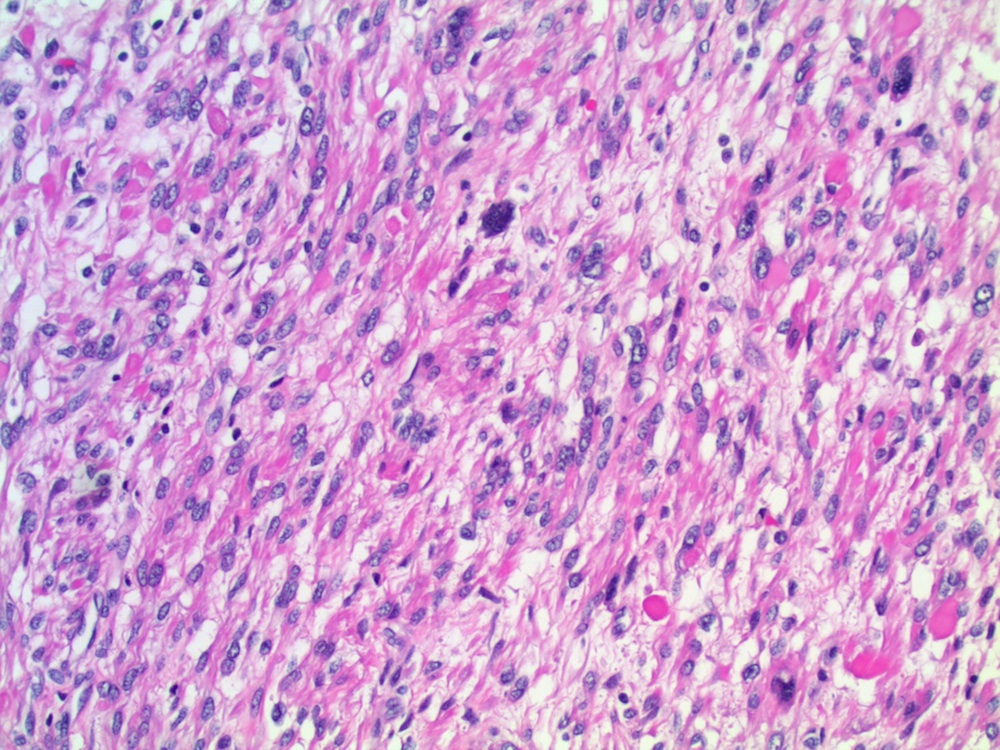
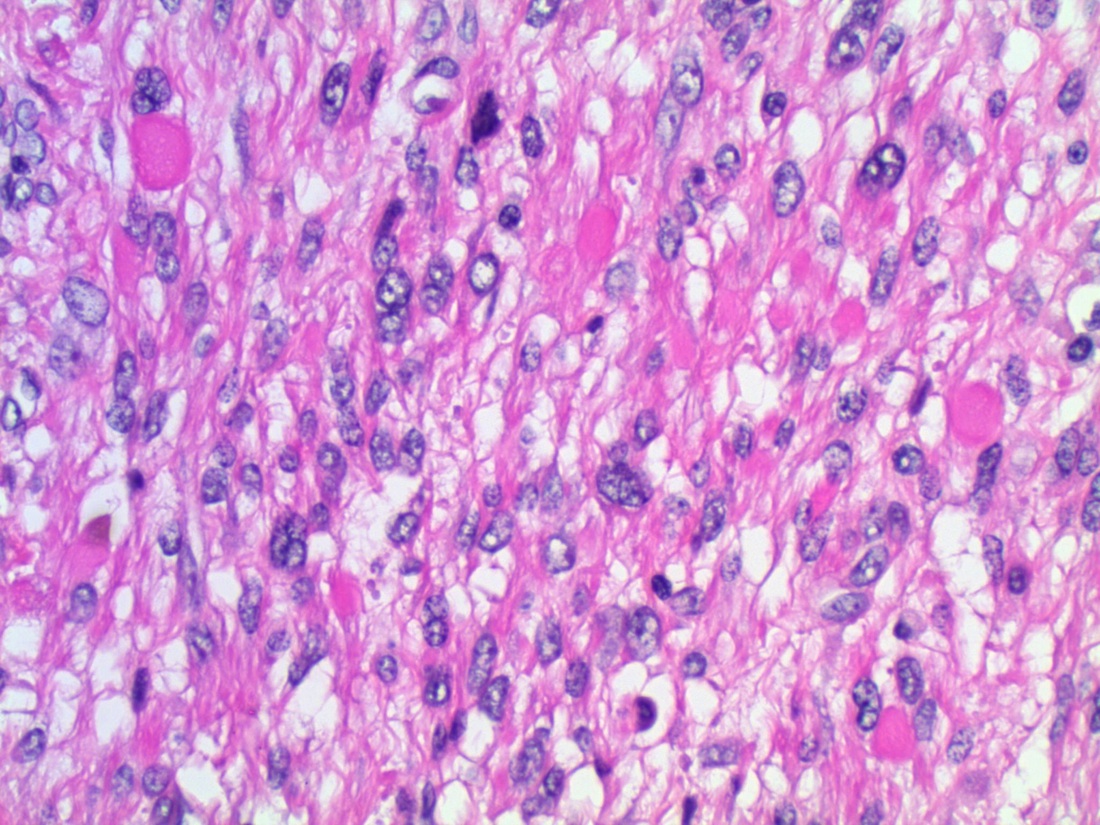
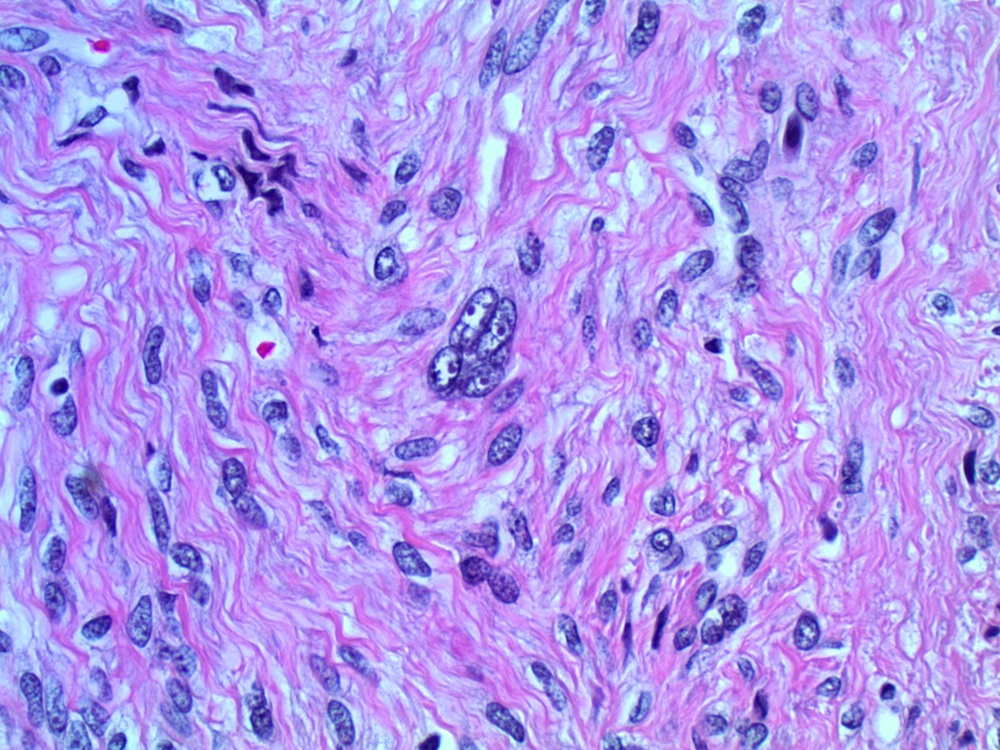
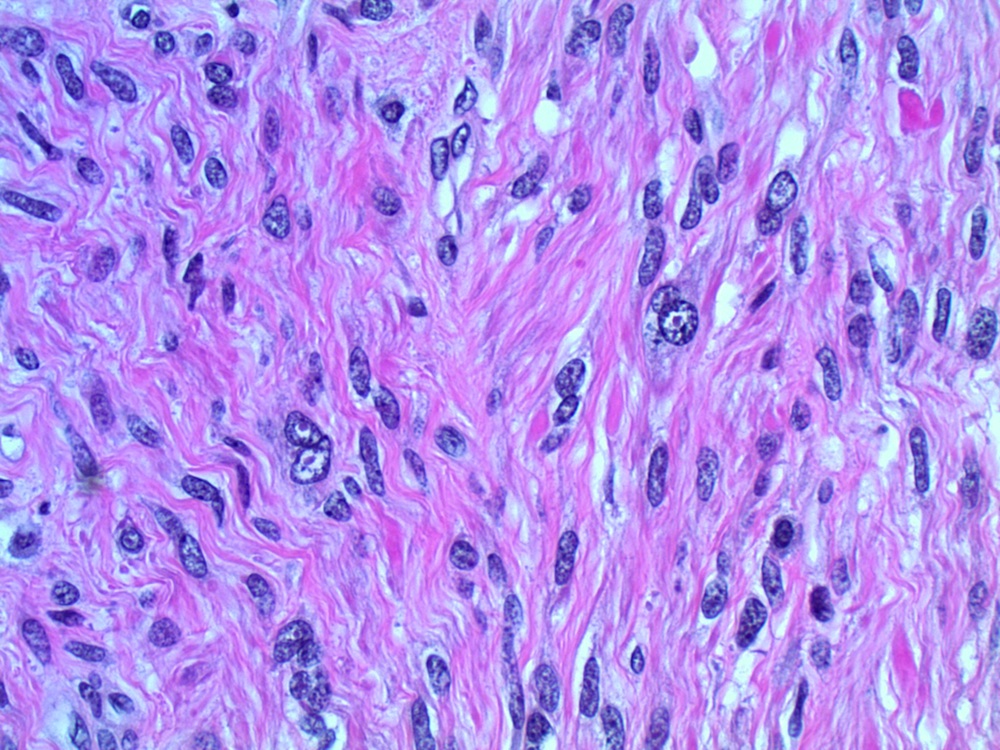
Microscopic images:
What is your diagnosis?
Diagnosis: Leiomyoma with bizarre nuclei, showing features suggestive of hereditary leiomyomatosis and renal cell carcinoma syndrome (HLRCC)
Discussion:
The key H&E morphologic features of this case include distinct eosinophilic (cherry-red) nucleoli surrounded by a perinucleolar halo (seen in the atypical cells and less obviously but also present in the nonatypical cells), cytoplasmic eosinophilic globules and background hemangioperiocytoma (HPC)-like vasculature (Am J Surg Pathol 2011;35:1235, Am J Surg Pathol 2013;37:74, Mod Pathol 2014;27:1020, Am J Surg Pathol 2019;43:1170).
HLRCC is an autosomal dominant syndrome due to germline mutations in the fumarate hydratase (FH) gene, a Kreb's cycle component (see Renal cell carcinoma-general). Syndromic patients are at risk for cutaneous and uterine leiomyomas, often presenting at a relatively young age, as well as an aggressive papillary type renal cell carcinoma (Am J Hum Genet 2003;73:95). A high level of fumarate, which accumulates in HLRCC tumor cells, causes aberrant succination of cellular proteins by forming a stable chemical modification, S-(2-succino)-cysteine (2SC), which can be detected by immunohistochemistry and is useful to differentiate HLRCC renal tumors from other high grade renal cell carcinomas (Am J Surg Pathol 2014;38:627). In this case, 2SC IHC was positive (image not available).
For nonsyndromic patients, leiomyoma with bizarre nuclei has a low recurrence rate (< 2%) with a negligible risk for distant metastasis. Leiomyoma with bizarre nuclei is the term preferred by the World Health Organization classification of tumors; other terms found in the literature include atypical leiomyoma and simplastic leiomyoma. It is currently regarded as a benign entity. If found in hysterectomy, no further treatment is needed. If seen in myomectomy, follow up for local intrauterine residual / recurrent disease is warranted (Am J Surg Pathol 2013;37:643). If there is residual tumor on imaging, it is important to monitor for regrowth and consider complete resection; features of malignancy can be focal in a leiomyosarcoma and in an incompletely resected tumor this diagnosis should still need consideration. Awareness of the morphologic features of HLRCC associated with symplastic / atypical / bizarre leiomyoma is important, because many patients lack a positive family history due to incomplete or variable penetrance, and the pathology report may lead to mutational testing and genetic counseling (Am J Surg Pathol 2019;43:639). For syndromic patients, annual surveillance by MRI is recommended beginning at age 8 years to detect the aggressive renal cell carcinoma (Int J Nephrol Renovasc Dis 2014;7:253).
Reference: Hum Pathol 2014;45:2311
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Ankur Sangoi, El Camino Hospital, California (USA), for contributing this case and part of the discussion. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.

Shop Amazon.com! Win a $100, $50 or $25 Amazon Gift Card!
To promote shopping at Amazon.com, particularly by going through our website, we will award Amazon gift cards of $100, $50 and $25 through a drawing of those who made purchases at Amazon.com in May or June 2015.
Website news:
(1) We have now posted the 2014 Jobs Report summary, click here. It is also available from going to the Jobs page, then click on Pathologist Jobs Report, then click on 2014 summary.
(2) We have now added the names of all the Case of the Week contributors to our main Case of the Week page. We thank all of our contributors once again and don't forget to check out our upcoming cases for the next few weeks!
Visit and follow our Blog to see recent updates to the website.
(1) We have now posted the 2014 Jobs Report summary, click here. It is also available from going to the Jobs page, then click on Pathologist Jobs Report, then click on 2014 summary.
(2) We have now added the names of all the Case of the Week contributors to our main Case of the Week page. We thank all of our contributors once again and don't forget to check out our upcoming cases for the next few weeks!
Visit and follow our Blog to see recent updates to the website.
Case #352
Clinical history:
The pathologist received a morcellated myomectomy specimen from a 38 year old woman with leiomyomas.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Leiomyoma with bizarre nuclei, showing features suggestive of hereditary leiomyomatosis and renal cell carcinoma syndrome (HLRCC)
Discussion:
The key H&E morphologic features of this case include distinct eosinophilic (cherry-red) nucleoli surrounded by a perinucleolar halo (seen in the atypical cells and less obviously but also present in the nonatypical cells), cytoplasmic eosinophilic globules and background hemangioperiocytoma (HPC)-like vasculature (Am J Surg Pathol 2011;35:1235, Am J Surg Pathol 2013;37:74, Mod Pathol 2014;27:1020, Am J Surg Pathol 2019;43:1170).
HLRCC is an autosomal dominant syndrome due to germline mutations in the fumarate hydratase (FH) gene, a Kreb's cycle component (see Renal cell carcinoma-general). Syndromic patients are at risk for cutaneous and uterine leiomyomas, often presenting at a relatively young age, as well as an aggressive papillary type renal cell carcinoma (Am J Hum Genet 2003;73:95). A high level of fumarate, which accumulates in HLRCC tumor cells, causes aberrant succination of cellular proteins by forming a stable chemical modification, S-(2-succino)-cysteine (2SC), which can be detected by immunohistochemistry and is useful to differentiate HLRCC renal tumors from other high grade renal cell carcinomas (Am J Surg Pathol 2014;38:627). In this case, 2SC IHC was positive (image not available).
For nonsyndromic patients, leiomyoma with bizarre nuclei has a low recurrence rate (< 2%) with a negligible risk for distant metastasis. Leiomyoma with bizarre nuclei is the term preferred by the World Health Organization classification of tumors; other terms found in the literature include atypical leiomyoma and simplastic leiomyoma. It is currently regarded as a benign entity. If found in hysterectomy, no further treatment is needed. If seen in myomectomy, follow up for local intrauterine residual / recurrent disease is warranted (Am J Surg Pathol 2013;37:643). If there is residual tumor on imaging, it is important to monitor for regrowth and consider complete resection; features of malignancy can be focal in a leiomyosarcoma and in an incompletely resected tumor this diagnosis should still need consideration. Awareness of the morphologic features of HLRCC associated with symplastic / atypical / bizarre leiomyoma is important, because many patients lack a positive family history due to incomplete or variable penetrance, and the pathology report may lead to mutational testing and genetic counseling (Am J Surg Pathol 2019;43:639). For syndromic patients, annual surveillance by MRI is recommended beginning at age 8 years to detect the aggressive renal cell carcinoma (Int J Nephrol Renovasc Dis 2014;7:253).
Reference: Hum Pathol 2014;45:2311