14 May 2014 - Case #312
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Joseph Fullmer, Upstate Medical University (USA) for contributing this case and part of the discussion.
Advertisement
Case #312
Clinical history:
A 1 day old boy had a prior ultrasound at 36 weeks showing a 7 x 6 cm cerebral fluid collection, with echogenicity suggestive for brain hemorrhage. Postnatal MRI on Emerson showed a large left hemispheric heterogeneous mass, occupying the posterior two - thirds of the left hemisphere, causing significant mass effect with midline shift and brainstem compression. The infant was taken immediately for surgery and a biopsy was obtained.
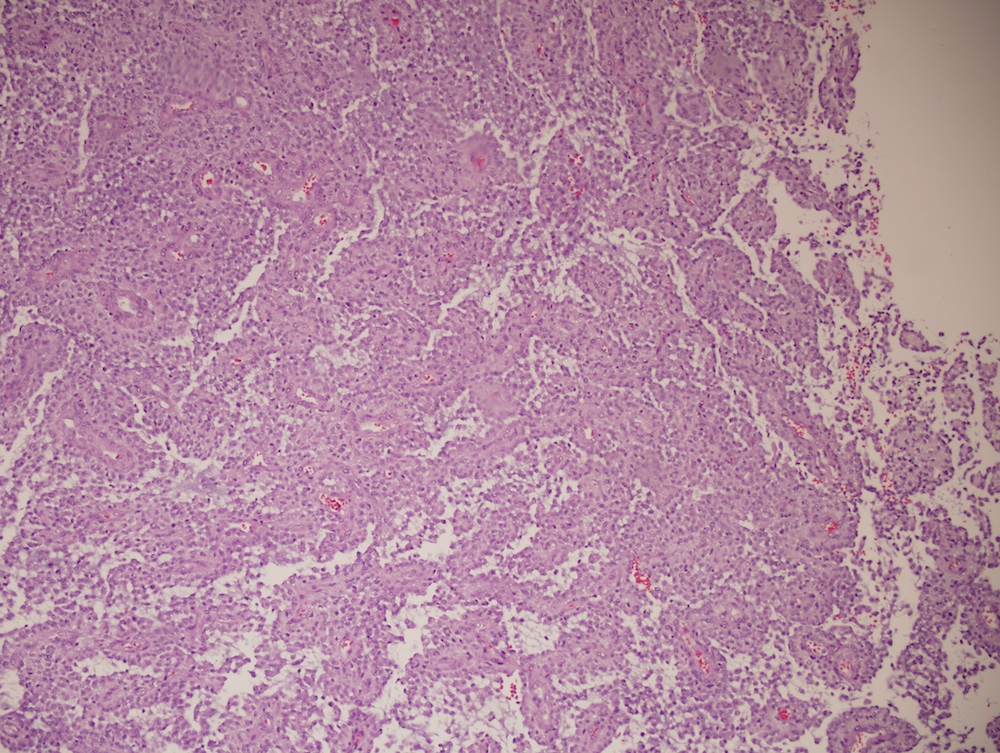
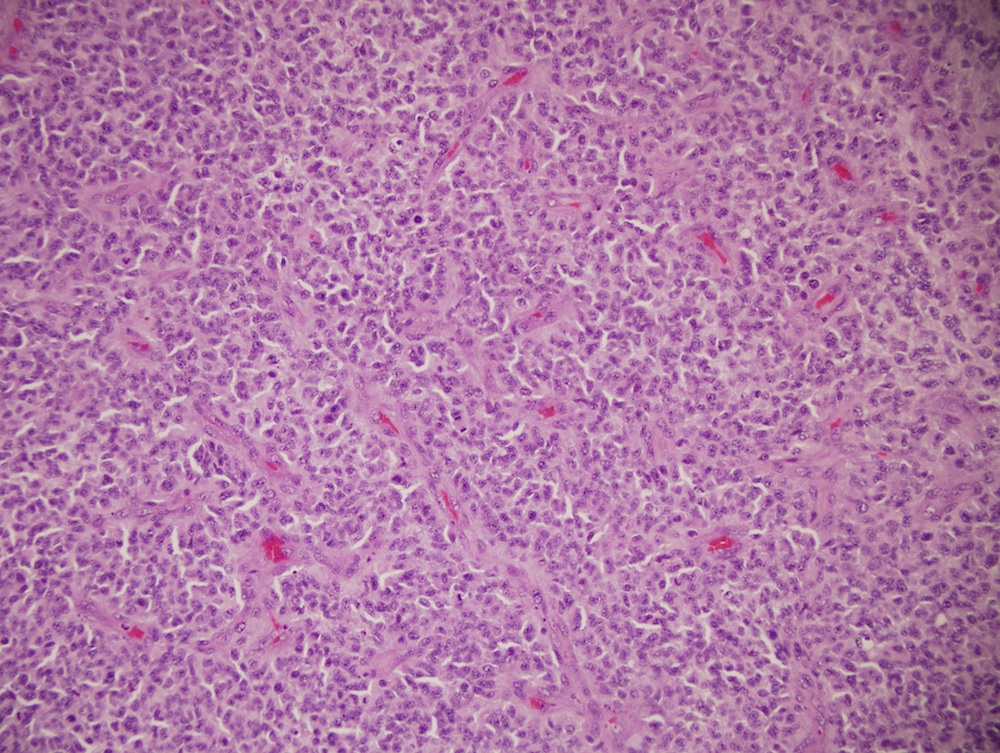
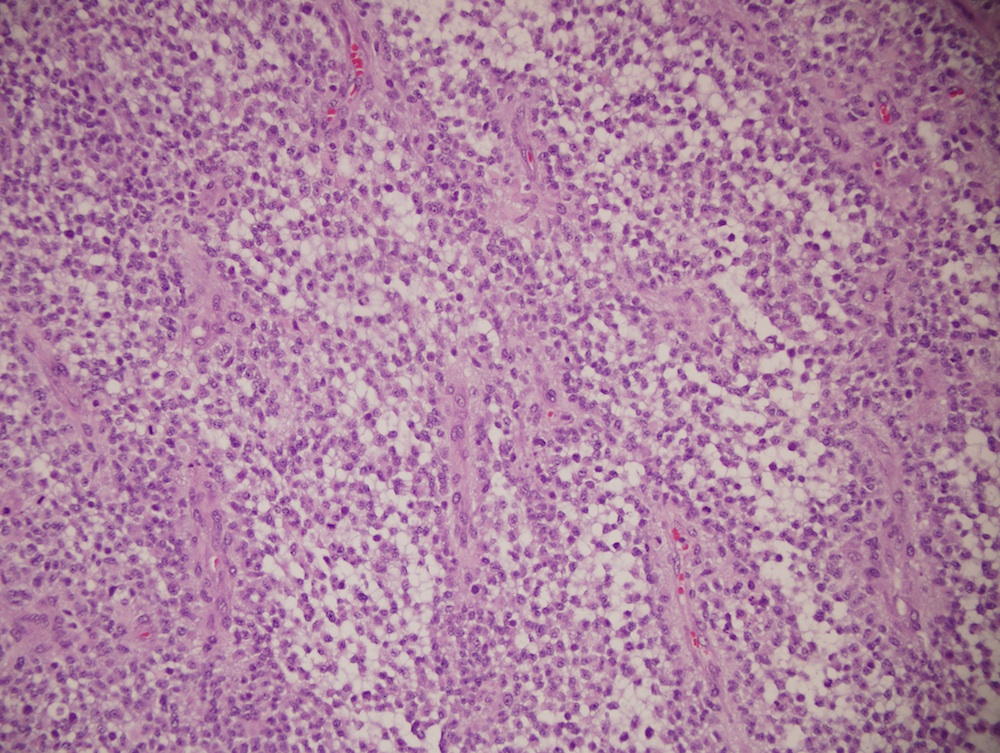
Microscopic images:
What is your diagnosis?
Diagnosis: Malignant astroblastoma
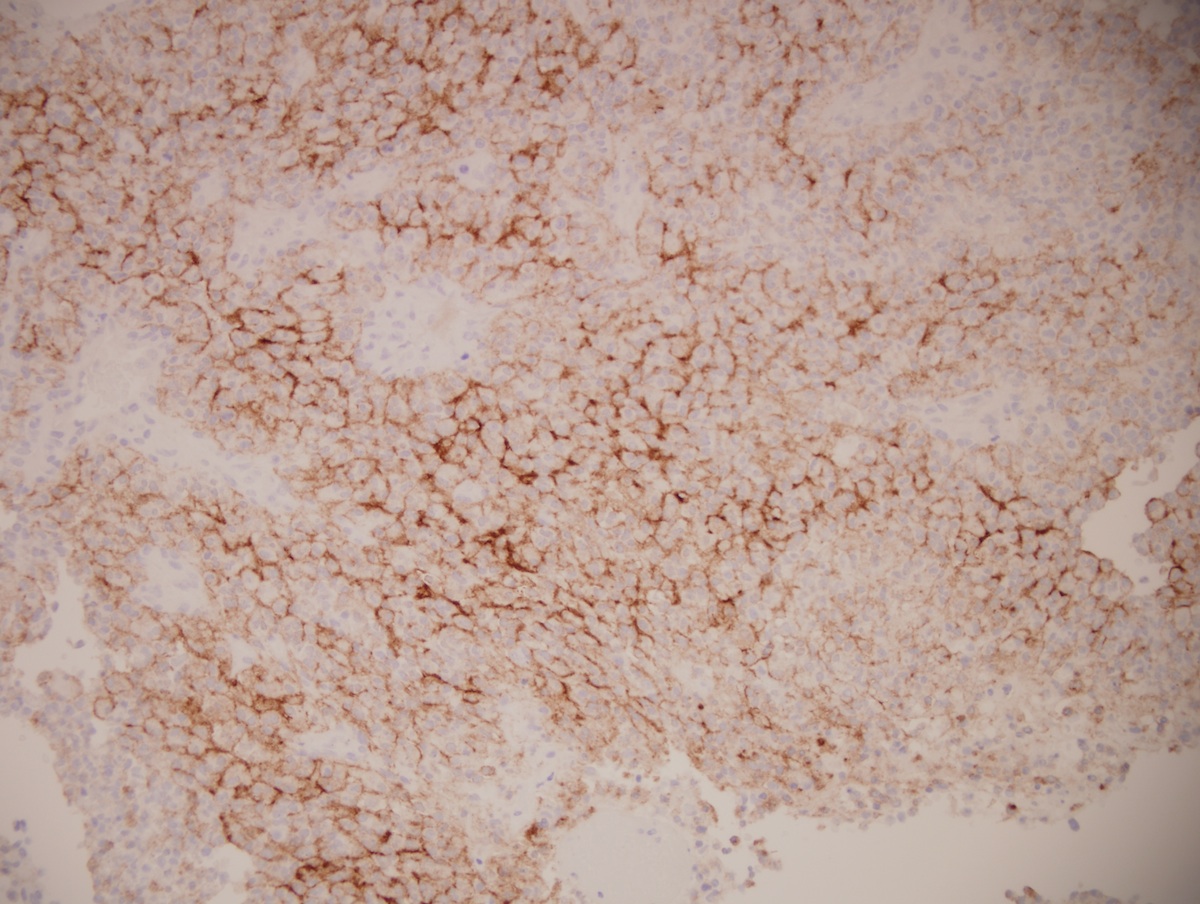
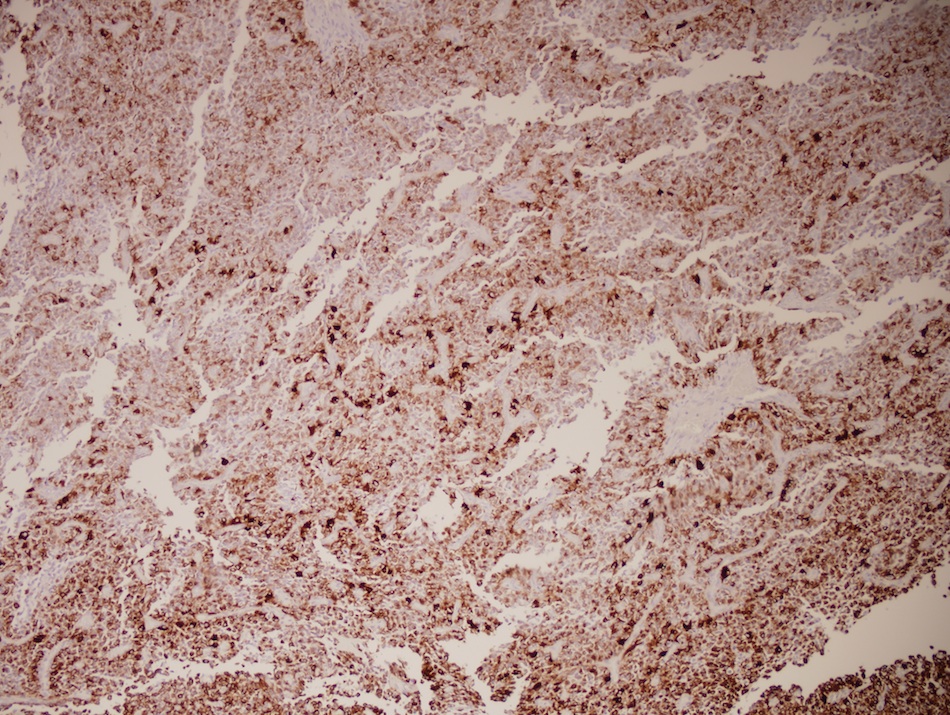
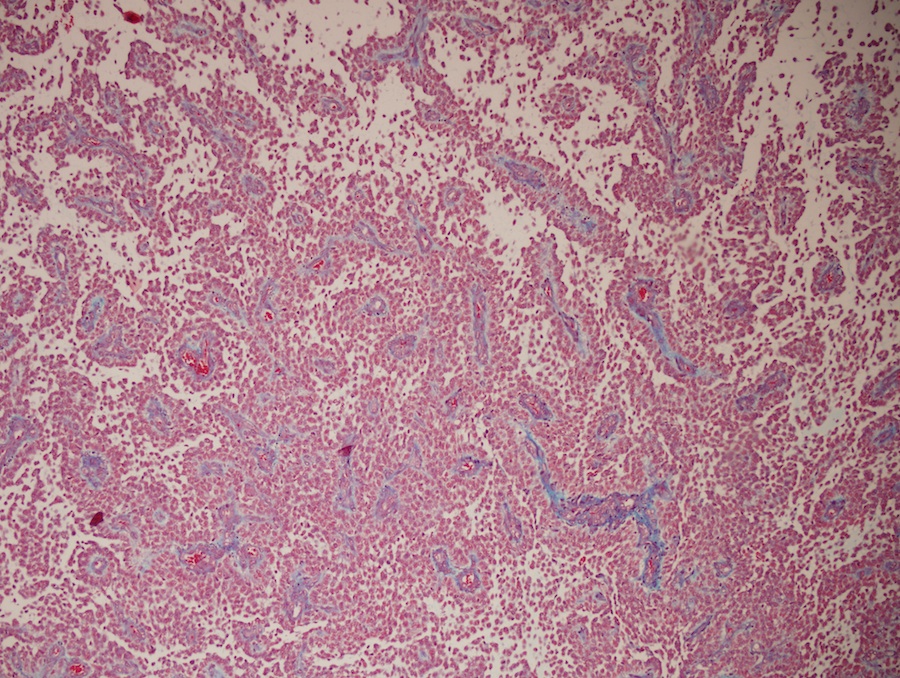
Immunostains:
Discussion:
Astroblastoma is a rare (< 3% of primary brain gliomas), compact glial neoplasm with perivascular pseudorosettes formed of GFAP+ cells arranged around central, often sclerotic, blood vessels (Wikipedia: Astroblastoma [Accessed 22 March 2024]). No WHO grade is assigned to this entity. It typically affects children and young adults, with a median age of 11 years.
Grossly, it is often a well circumscribed, peripheral, cerebral hemispheric mass that is firm and often cystic. Microscopically, it is well circumscribed with discrete pushing borders. High grade lesions may be infiltrative. Most astroblastomas have perivascular pseudorosettes resembling ependymoma, but with thick processes from the cell body to the adventitia of the vessel. Vascular hyalinization is common, with little fibrillar background. It is recommended to limit this diagnosis to tumors with a predominance of these features, which may be present focally in other tumors. High grade / malignant astroblastomas, such as this tumor, have hypercellular and mitotically active regions, often with vascular proliferation or necrosis with pseudopalisading. EMA highlights the cell membranes, GFAP stains tumor cells and trichrome stains vascular sclerosis.
The differential diagnosis includes:
Treatment consists of resection for well differentiated tumors but should be more aggressive for malignant tumors, which often recur (NIH: Astroblastoma [Accessed 22 March 2024]).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Joseph Fullmer, Upstate Medical University (USA) for contributing this case and part of the discussion.

Scientific Symposiums International Summer CME Series
Critical Issues in Cutaneous Pathology: Improving Your Diagnostic Accuracy
June 23-26, 2014
Hilton Head Island, South Carolina (USA)
Still Looking to fulfill your 2014 CME, SAMS/MOCS accreditation?
Join us this summer for an ALL NEW Dermatopathology course on Hilton Head Island, South Carolina
Register for our upcoming Dermatopathology course being held this June in order to learn the latest critical issues in Cutaneous Pathology and how to improve your diagnostic accuracy.
Our world-renowned faculty include Dirk M. Elston, M.D., Janis Taube, M.D.,Msc, Jinah Kim, M.D., Ph.D, and Loren Clarke, M.D.
This course is one not to be missed!
Website news:
(1) Thanks to the following image contributors to these topics:
(2) We posted an original article, The Warning Signs of a Failing Billing Company or Revenue Cycle Management Firm, by Mick Raich, Vachette Pathology.
(3) We have now posted the Pathology Jobs Report for the first quarter of 2014, available from the Jobs page or by clicking here. Learn what specialties are hot, and what employers are looking for.
Visit and follow our Blog to see recent updates to the website.
(1) Thanks to the following image contributors to these topics:
- Dr. Asmaa Gaber Abdou - Skin - Nonmelanocytic tumors - Verrucous carcinoma
- Dr. Elaine Alt - Colon non tumor - Ulcerative colitis
- Dr. Rico Lasaca - Parasitology - Schistosomiasis
- Dr. Marilin Rosa - Cervix-Cytology - Atrophy
- Dr. Semir Vranic - Breast - malignant - Ductal carcinoma, NOS - general, Breast - malignant - Neuroendocrine carcinoma - general
(2) We posted an original article, The Warning Signs of a Failing Billing Company or Revenue Cycle Management Firm, by Mick Raich, Vachette Pathology.
(3) We have now posted the Pathology Jobs Report for the first quarter of 2014, available from the Jobs page or by clicking here. Learn what specialties are hot, and what employers are looking for.
Visit and follow our Blog to see recent updates to the website.
Case #312
Clinical history:
A 1 day old boy had a prior ultrasound at 36 weeks showing a 7 x 6 cm cerebral fluid collection, with echogenicity suggestive for brain hemorrhage. Postnatal MRI on Emerson showed a large left hemispheric heterogeneous mass, occupying the posterior two - thirds of the left hemisphere, causing significant mass effect with midline shift and brainstem compression. The infant was taken immediately for surgery and a biopsy was obtained.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Malignant astroblastoma
Immunostains:
Discussion:
Astroblastoma is a rare (< 3% of primary brain gliomas), compact glial neoplasm with perivascular pseudorosettes formed of GFAP+ cells arranged around central, often sclerotic, blood vessels (Wikipedia: Astroblastoma [Accessed 22 March 2024]). No WHO grade is assigned to this entity. It typically affects children and young adults, with a median age of 11 years.
Grossly, it is often a well circumscribed, peripheral, cerebral hemispheric mass that is firm and often cystic. Microscopically, it is well circumscribed with discrete pushing borders. High grade lesions may be infiltrative. Most astroblastomas have perivascular pseudorosettes resembling ependymoma, but with thick processes from the cell body to the adventitia of the vessel. Vascular hyalinization is common, with little fibrillar background. It is recommended to limit this diagnosis to tumors with a predominance of these features, which may be present focally in other tumors. High grade / malignant astroblastomas, such as this tumor, have hypercellular and mitotically active regions, often with vascular proliferation or necrosis with pseudopalisading. EMA highlights the cell membranes, GFAP stains tumor cells and trichrome stains vascular sclerosis.
The differential diagnosis includes:
- Ependymoma: more fibrillar, nuclei smaller and less pleomorphic, true rosettes, less sclerosis; GFAP stains around blood vessels only; EMA has a dot-like or ring-like pattern (AJNR Am J Neuroradiol 2002;23:243, Childs Nerv Syst 2005;21:211)
- Pilocytic astrocytoma: biphasic piloid areas with Rosenthal fibers alternating with spongy microcystic areas with eosinophilic granular bodies
- Pleomorphic xanthoastrocytoma: fascicular pattern, pleomorphic cells, lipidized cells, eosinophilic granular bodies, perivascular lymphocytes
Treatment consists of resection for well differentiated tumors but should be more aggressive for malignant tumors, which often recur (NIH: Astroblastoma [Accessed 22 March 2024]).