26 October 2011 - Case #221
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Huma Siddiqui, South Texas Veterans Health Care System (USA).
CancerTYPE ID is a standardized, objective molecular test based on the differential expression of 92 genes, that classifies tumors by matching the gene expression pattern of a patients tumor tissue to a database of known tumor types and histological subtypes.
CancerTYPE IDs database includes 2,206 tumors from multiple tumor banks, selected to provide broader and deeper representation of the heterogeneity of tumors. The 92-gene assay does not overlap with IHC markers, providing complementary data to standard tumor diagnosis.
CancerTYPE ID uses real-time reverse transcription polymerase chain reaction (RT-PCR). A very low copy number of RNA molecules can be detected, thus reducing the sample tissue required for testing. Testing is conducted and results are generated at bioTheranostics' CAP-accredited, CLIA-certified laboratory.
Advertisement
Case #221
Clinical history:
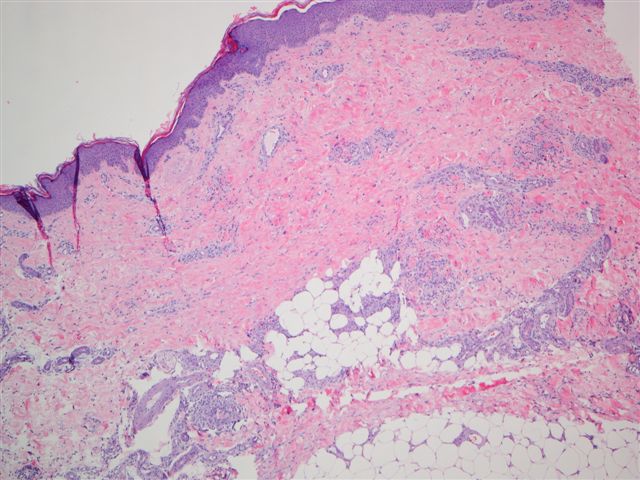
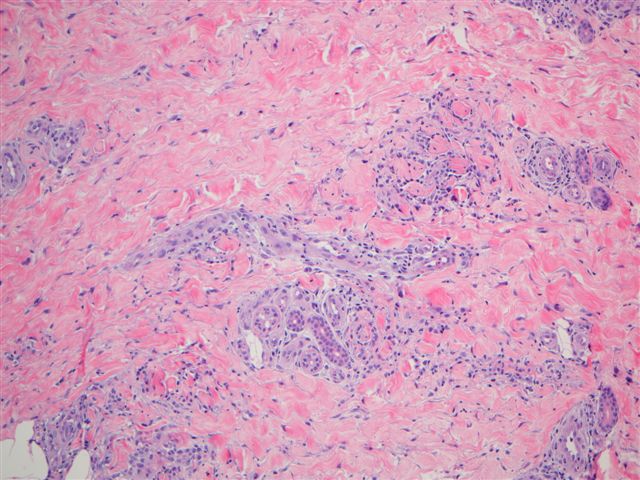
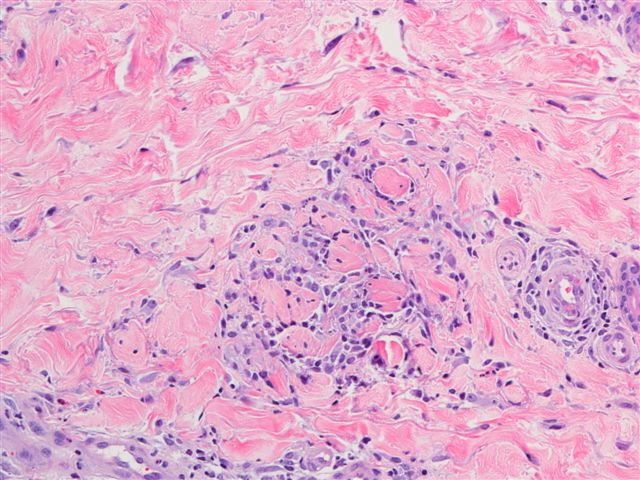
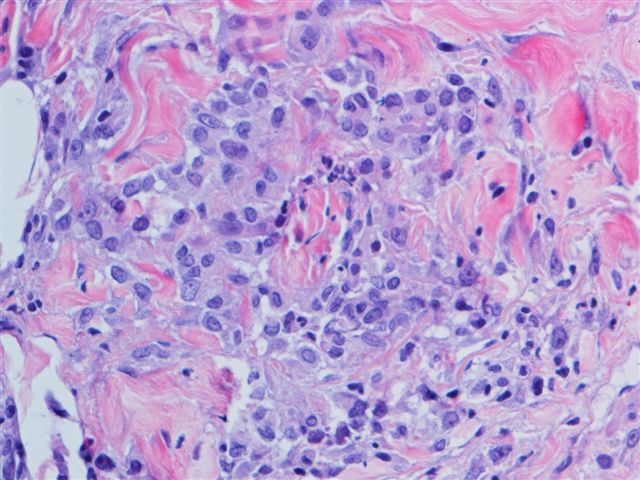
A 34 year old white woman with a history of SLE had a rash involving her trunk and extremities, which was biopsied.
Microscopic images:
What is your diagnosis?
Diagnosis: Palisaded neutrophilic and granulomatous dermatitis
Discussion:
Palisaded neutrophilic and granulomatous dermatitis (PNGD) typically presents as a papular eruption on the extremities in patients with lupus erythematosus (women or men), rheumatoid arthritis or other immune complex disorders (Dermatol Online J 2003;9:1, Arch Dermatol 1994;130:1278). There often are linear inflammatory indurations on the lateral aspects of the trunk (rope sign). Occasionally, there is no systemic disease (Indian J Dermatol Venereol Leprol 2011;77:615). Due to a variable clinical presentation, it has been called Churg-Strauss granuloma, rheumatoid papules, superficial ulcerating rheumatoid necrobiosis and interstitital granulomatous dermatitis with arthritis.
Clinically, most lesions are symmetrically distributed on the extremities, with variable numbers of lesions. There is a spectrum of histologic changes, ranging from early leukocytoclastic vasculitis with dense neutrophilic infiltrates and degenerated collagen, to later findings of palisaded granulomas surrounding neutrophilic debris, fibrin and degenerated collagen.
The differential diagnosis includes granulomatous drug reactions (vacuolar interface changes, often epidermotropic lymphocytes, resolves with discontinuation of drug), rheumatoid dermatosis (marked homogeneous necrobiosis with numerous giant cells and stromal fibrosis), interstitial granuloma annulare (mid dermal necrobiotic collagen surrounded by palisading histiocytes, fibroblasts and lymphocytes; variable mucin, vasculitis, foreign body giant cells) and necrotizing granulomas due to infectious organisms.
Treatment of the underlying collagen vascular disease may provide a good response, although recurrences are common.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Huma Siddiqui, South Texas Veterans Health Care System (USA).
CancerTYPE ID is a standardized, objective molecular test based on the differential expression of 92 genes, that classifies tumors by matching the gene expression pattern of a patients tumor tissue to a database of known tumor types and histological subtypes.
CancerTYPE IDs database includes 2,206 tumors from multiple tumor banks, selected to provide broader and deeper representation of the heterogeneity of tumors. The 92-gene assay does not overlap with IHC markers, providing complementary data to standard tumor diagnosis.
CancerTYPE ID uses real-time reverse transcription polymerase chain reaction (RT-PCR). A very low copy number of RNA molecules can be detected, thus reducing the sample tissue required for testing. Testing is conducted and results are generated at bioTheranostics' CAP-accredited, CLIA-certified laboratory.
Website news:
(1) We are looking for more cases of the week. We are also looking for a reviewer(s) for the Salivary Gland chapter, and authors with expertise in AP computer systems and LIS systems, to add content to these pages. For more information, click here.
(2) Thanks to everyone who stopped by our booth at ASCP. We received many new ideas, and hope to have authors for new topics and more reviewers.
(3) We posted an article on our Management page, 2012 ICD-9 Code Changes Bring Significant Changes for Pathology / Lab Coding, by Laura Edgeworth, PSA, LLC. We have also added another Coding question, about sentinel node biopsy.
(4) Thanks to Jessica Wallace, PA, Bassett Medical Center, Cooperstown, NY for authoring a new chapter on Frozen Sections.
Visit and follow our Blog to see recent updates to the website.
(1) We are looking for more cases of the week. We are also looking for a reviewer(s) for the Salivary Gland chapter, and authors with expertise in AP computer systems and LIS systems, to add content to these pages. For more information, click here.
(2) Thanks to everyone who stopped by our booth at ASCP. We received many new ideas, and hope to have authors for new topics and more reviewers.
(3) We posted an article on our Management page, 2012 ICD-9 Code Changes Bring Significant Changes for Pathology / Lab Coding, by Laura Edgeworth, PSA, LLC. We have also added another Coding question, about sentinel node biopsy.
(4) Thanks to Jessica Wallace, PA, Bassett Medical Center, Cooperstown, NY for authoring a new chapter on Frozen Sections.
Visit and follow our Blog to see recent updates to the website.
Case #221
Clinical history:
A 34 year old white woman with a history of SLE had a rash involving her trunk and extremities, which was biopsied.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Palisaded neutrophilic and granulomatous dermatitis
Discussion:
Palisaded neutrophilic and granulomatous dermatitis (PNGD) typically presents as a papular eruption on the extremities in patients with lupus erythematosus (women or men), rheumatoid arthritis or other immune complex disorders (Dermatol Online J 2003;9:1, Arch Dermatol 1994;130:1278). There often are linear inflammatory indurations on the lateral aspects of the trunk (rope sign). Occasionally, there is no systemic disease (Indian J Dermatol Venereol Leprol 2011;77:615). Due to a variable clinical presentation, it has been called Churg-Strauss granuloma, rheumatoid papules, superficial ulcerating rheumatoid necrobiosis and interstitital granulomatous dermatitis with arthritis.
Clinically, most lesions are symmetrically distributed on the extremities, with variable numbers of lesions. There is a spectrum of histologic changes, ranging from early leukocytoclastic vasculitis with dense neutrophilic infiltrates and degenerated collagen, to later findings of palisaded granulomas surrounding neutrophilic debris, fibrin and degenerated collagen.
The differential diagnosis includes granulomatous drug reactions (vacuolar interface changes, often epidermotropic lymphocytes, resolves with discontinuation of drug), rheumatoid dermatosis (marked homogeneous necrobiosis with numerous giant cells and stromal fibrosis), interstitial granuloma annulare (mid dermal necrobiotic collagen surrounded by palisading histiocytes, fibroblasts and lymphocytes; variable mucin, vasculitis, foreign body giant cells) and necrotizing granulomas due to infectious organisms.
Treatment of the underlying collagen vascular disease may provide a good response, although recurrences are common.