6 October 2011 - Case #219
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. David Cohen, Herzliyah Medical Center, Israel.

Attend a Free 30 minute Webinar:
Best Practices for Pathology Document Management
Wednesday, October 12, 2011 at 12:00pm Eastern time
Learn how to:
Sponsored by AccuCore Group, (267) 564-5015Advertisement
Case #219
Clinical history:
A 76 year old man with an unknown clinical history had an irregular process on the posterior bladder wall, which was biopsied.
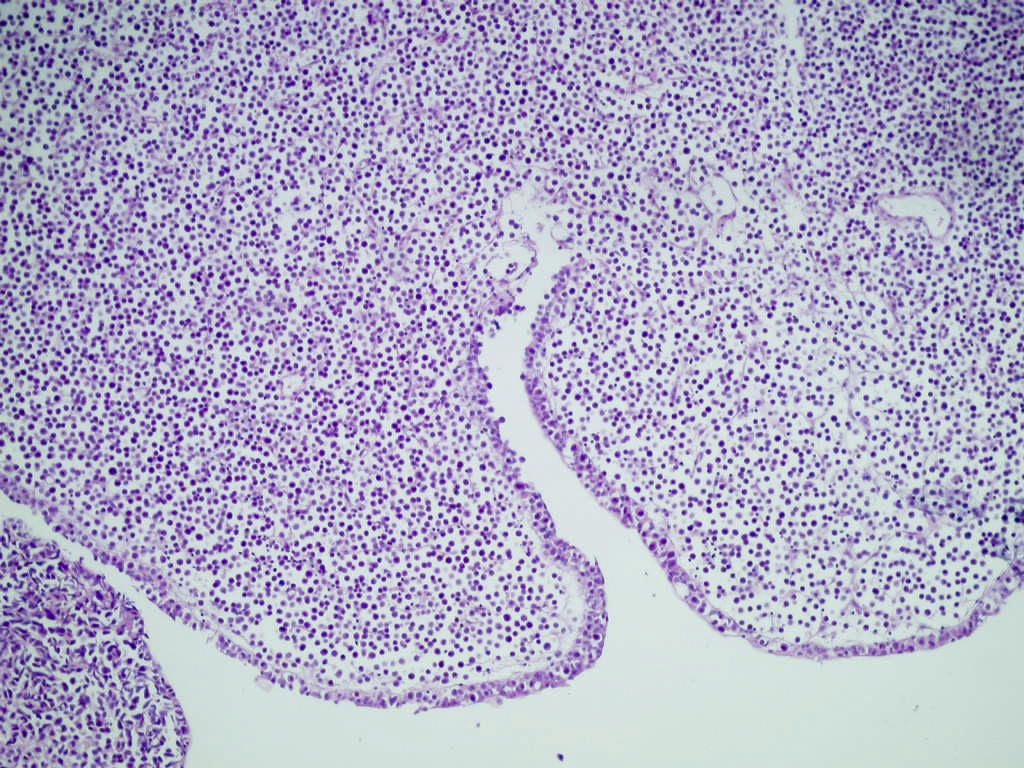
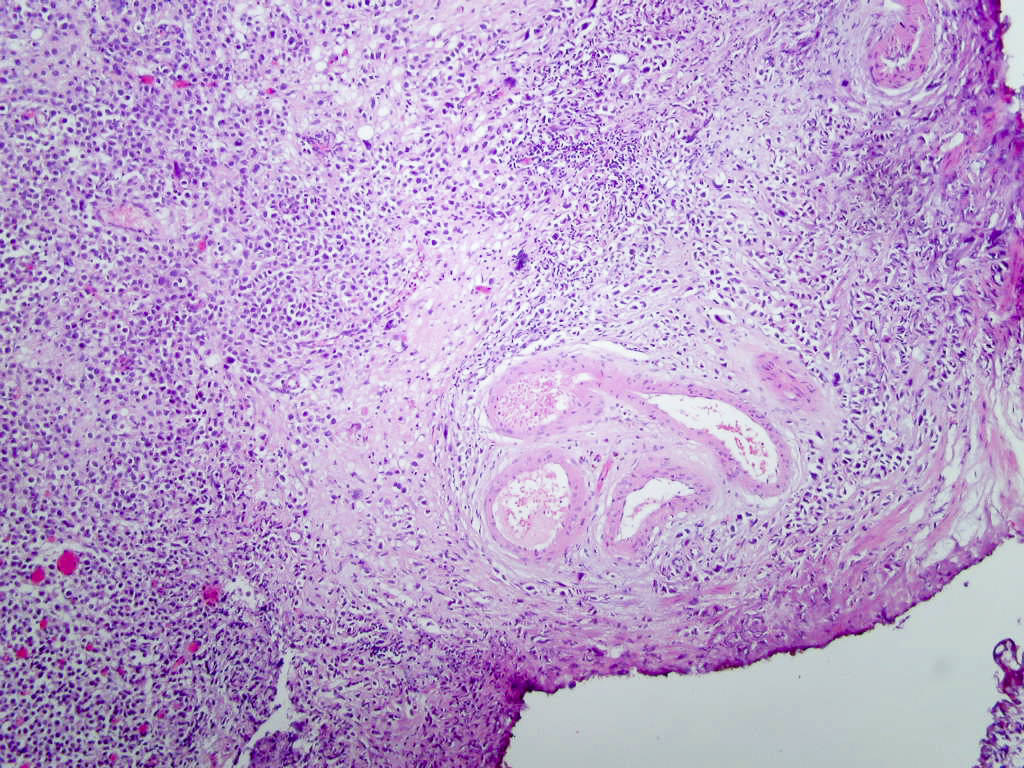
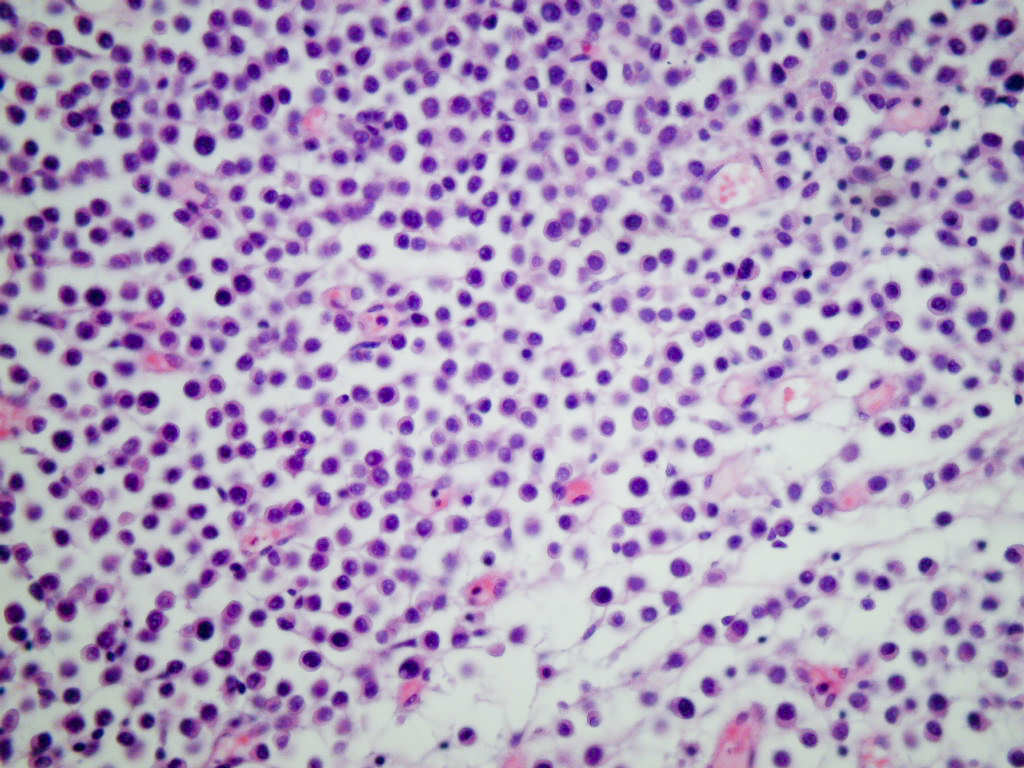
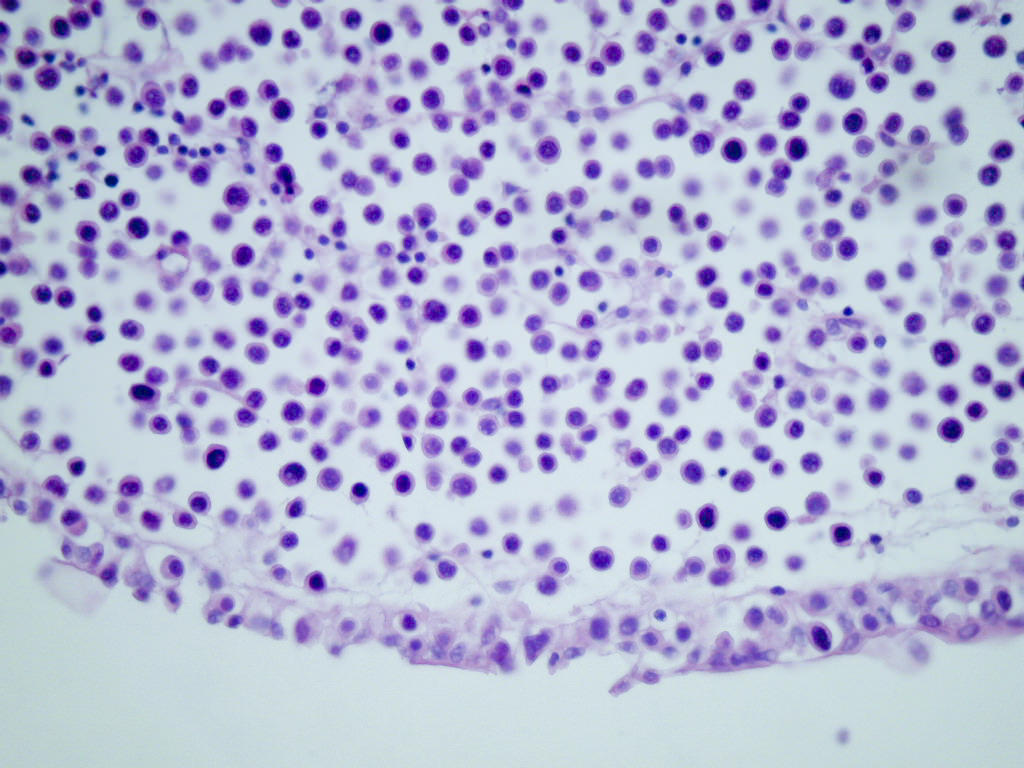
Microscopic images:
What is your diagnosis?
Diagnosis: High grade urothelial carcinoma, plasmacytoid and lymphoma-like variant
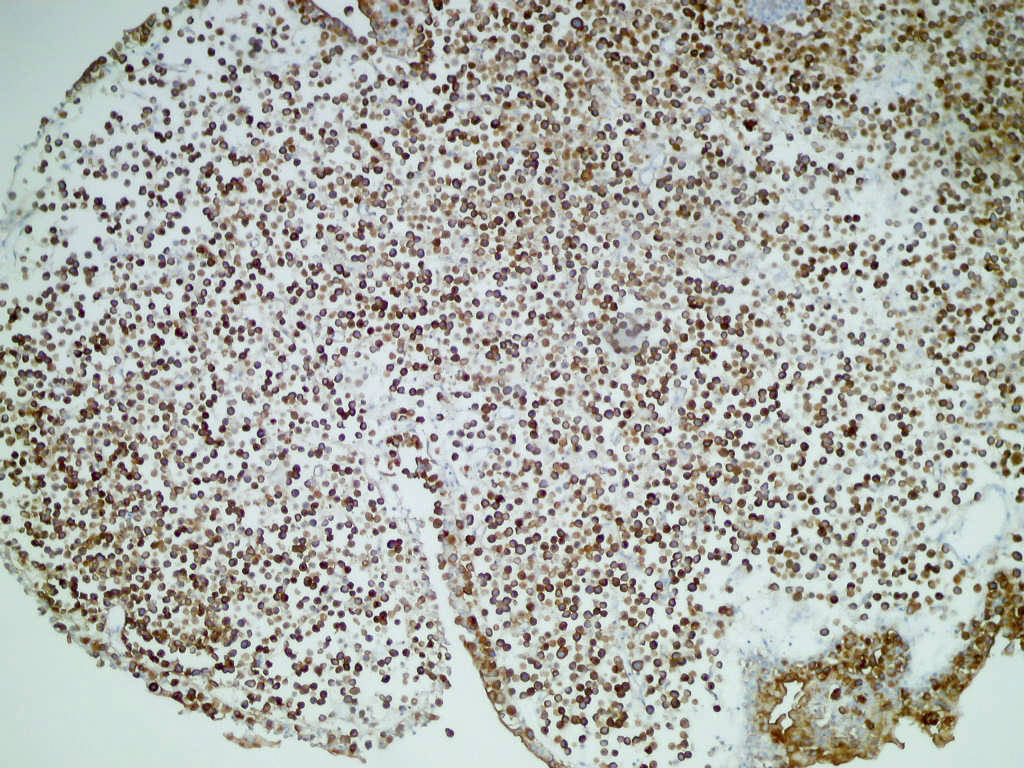
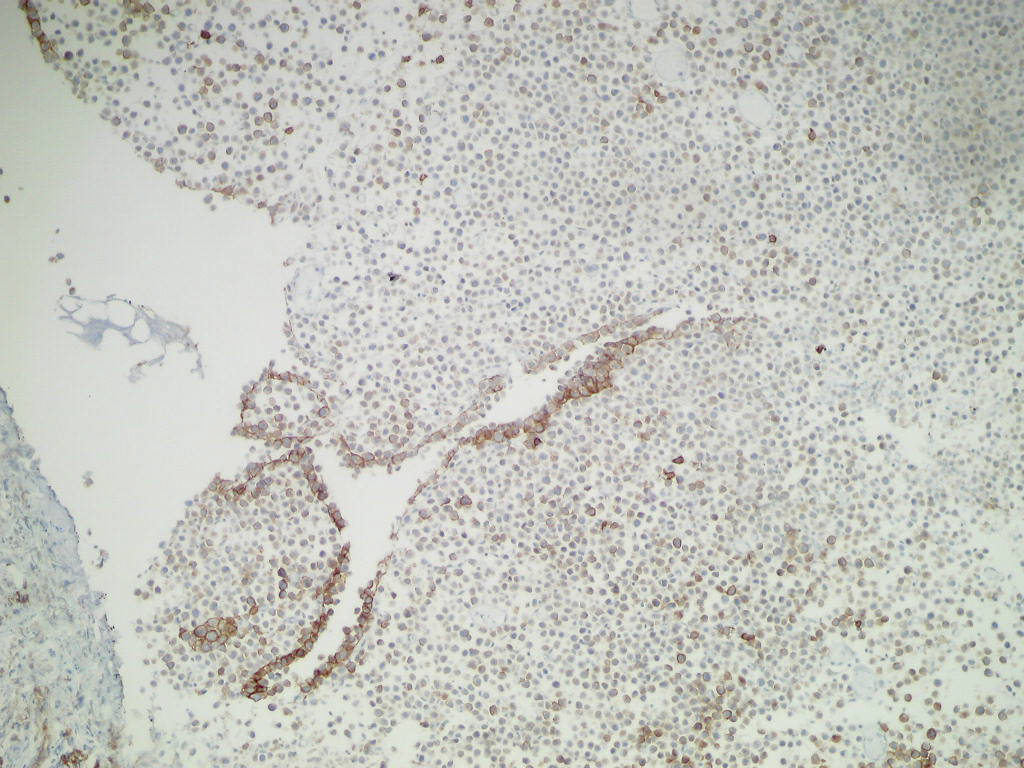
Immunostains:
Discussion:
The tumor consisted of a dyscohesive pattern of urothelial tumor cells resembling plasma cells, due to abundant glassy eosinophilic cytoplasm and eccentric nuclei. No binucleated forms were present. In some areas, the tumor resembled a low grade lymphoma. Obvious areas of high grade urothelial carcinoma were also present in other sections.
Plasmacytoid variant of urothelial carcinoma is part of the WHO / ISUP classification of tumors of the urinary tract. These tumors are rare and tend to present at advanced stage with a poor prognosis (Int J Cancer 2011;129:346). Tumors are strongly positive for epithelial markers (cytokeration, EMA) and GATA3, and are usually negative for CD38 and light chains, markers for plasma cells (Hum Pathol 2011;42:1149). There often is immunoreactivity for CD138 (Hum Pathol 2009;40:1023, Am J Surg Pathol 2009;33:417).
Differential diagnosis includes chronic cystitis and plasmacytoma, particularly a problem in limited biopsies.
Treatment consists of surgery plus chemotherapy (Int J Clin Oncol 2011;16:759).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. David Cohen, Herzliyah Medical Center, Israel.

Best Practices for Pathology Document Management
Learn how to:
- Reduce Pathology Dept. risk through good governance practices
- Improve productivity and address CAP, OSHA, ISO, The Joint Commission requirements
- Understand mandated ISO-15189-2003 requirements
- Leverage best practices to organize and share electronic documents
- Apply custom metadata to documents for effective taxonomies
- Automate change, review and approval processes
- Collaborate sharing Gross and Microscopic images
Sponsored by AccuCore Group, (267) 564-5015
Case #219
Clinical history:
A 76 year old man with an unknown clinical history had an irregular process on the posterior bladder wall, which was biopsied.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: High grade urothelial carcinoma, plasmacytoid and lymphoma-like variant
Immunostains:
Discussion:
The tumor consisted of a dyscohesive pattern of urothelial tumor cells resembling plasma cells, due to abundant glassy eosinophilic cytoplasm and eccentric nuclei. No binucleated forms were present. In some areas, the tumor resembled a low grade lymphoma. Obvious areas of high grade urothelial carcinoma were also present in other sections.
Plasmacytoid variant of urothelial carcinoma is part of the WHO / ISUP classification of tumors of the urinary tract. These tumors are rare and tend to present at advanced stage with a poor prognosis (Int J Cancer 2011;129:346). Tumors are strongly positive for epithelial markers (cytokeration, EMA) and GATA3, and are usually negative for CD38 and light chains, markers for plasma cells (Hum Pathol 2011;42:1149). There often is immunoreactivity for CD138 (Hum Pathol 2009;40:1023, Am J Surg Pathol 2009;33:417).
Differential diagnosis includes chronic cystitis and plasmacytoma, particularly a problem in limited biopsies.
Treatment consists of surgery plus chemotherapy (Int J Clin Oncol 2011;16:759).