31 August 2011 - Case #215
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Mandolin Summer Ziadie, Children's Medical Center of Dallas, Texas (USA).

The basic pathology research journal covering all biomedical disciplines in the broad spectrum of pathology.
New Options for Authors. Same Great Benefits.
Learn more about preparing your manuscript for submission to Laboratory Investigation online.
Visit us at www.laboratoryinvestigation.org for more information.
Advertisement
Case #215
Clinical history:
A 2 year old boy from El Paso was in good health until he began experiencing mild rhinorrhea and cough, followed by acute onset of left sided weakness. Lumbar puncture revealed a pleocytosis of 111 WBC. MRI revealed diffuse contrast enhancing lesions with surrounding edema throughout the bilateral cortex, midbrain, pons and cerebellum, thought to be consistent with cysticerci. The patient was managed with albendazole therapy and intravenous steroids, and improved sufficiently to be discharged home. A week later, he worsened again and presented with hemiparesis, ataxia and inability to handle secretions. By MRI, the lesions had increased in size. Pertinent history includes regular travel to Mexico but no known sick contacts at home and no known TB in the family. A biopsy was performed.
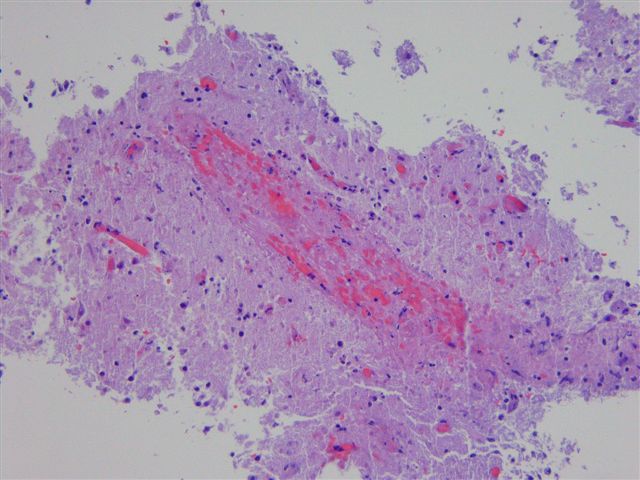
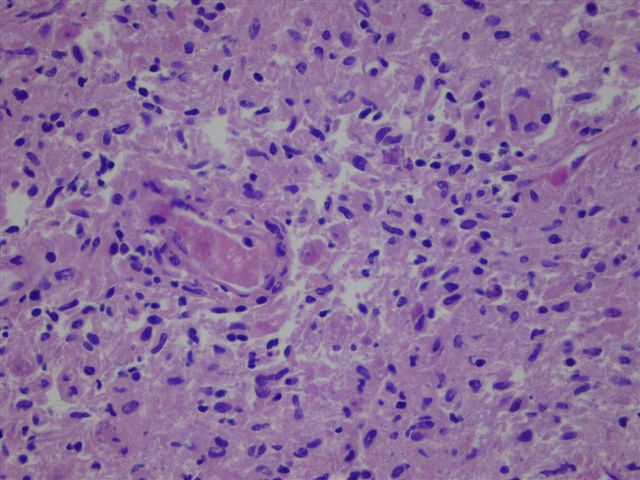
Microscopic images:
What is your diagnosis?
Diagnosis: Balamuthia mandrillaris encephalitis
Discussion:
The diagnosis was confirmed by PCR performed by the US Centers for Disease Control.
Balamuthia mandrilaris is an amoeba that primarily affects the nasal pyramid or the skin, producing granulomatous amoebic lesions (Hum Pathol 1999;30:269). The amoebae spread from the primary nasal lesion to the meninges, where they infiltrate vessels. Thrombotic amoebic angitis produces CNS infarcts, that are infiltrated by amoebae.
Balamuthia infection is extremely rare, with fewer than 200 human cases recognized worldwide since it was found to be a human pathogen in 1990. Balamuthia is often misdiagnosed as other neurologic diseases (Clin Infect Dis 2009;48:879). Infection occurs in both immunocompromised and otherwise healthy persons and often in children. Risk factors are poorly defined, but might include exposure to soil or stagnant water, young age and Hispanic ethnicity. Balamuthia can also be transmitted by organ transplant (MMWR Morb Mortal Wkly Rep 2010;59:1165).
Clinically, patients can have skin lesions months to years before having encephalitis symptoms. At biopsy, an amoebic trophozoite is observed, often infiltrating vessels. The amoebae have a nucleus with a large, central karyosome and vacuolated cytoplasm.
Once infection progresses to encephalitis, it is almost always fatal, although a few patients have survived (Clin Infect Dis 2010;51:e7, Pediatrics 2010;125:e699).
Differential diagnosis includes other amoebae that attack the CNS, including Acanthamoeba, Naegleria fowleri and Sappinia, which have microscopic differences in the cysts and trophozoites. In this case, the 2 year old boy died of his disease and no autopsy was performed.
Reference: CDC: Free Living Amebic Infections [Accessed 14 May 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Mandolin Summer Ziadie, Children's Medical Center of Dallas, Texas (USA).

The basic pathology research journal covering all biomedical disciplines in the broad spectrum of pathology.
New Options for Authors. Same Great Benefits.
- Open Access
- Color Choices
- Rapid publication
- Efficient Peer-Review
Learn more about preparing your manuscript for submission to Laboratory Investigation online.
Visit us at www.laboratoryinvestigation.org for more information.
Website news:
(1) We have updated the Chronic Myeloid Neoplasms chapter based on a review by Nikhil Sangle, M.D., FRCPath.(Engl.), University of Utah Health Sciences Center and ARUP Laboratories.
(2) We are looking for good grossing videos to add to our online textbook. If you know of any that we can use, or are interested in creating one, please contact us.
(3) We are looking for short (~500 words) pathology related educational articles to be included on our monthly Feature Page. This could be part of a presentation you have already given. Contact us with your ideas, if interested.
Visit and follow our Blog to see recent updates to the website.
(1) We have updated the Chronic Myeloid Neoplasms chapter based on a review by Nikhil Sangle, M.D., FRCPath.(Engl.), University of Utah Health Sciences Center and ARUP Laboratories.
(2) We are looking for good grossing videos to add to our online textbook. If you know of any that we can use, or are interested in creating one, please contact us.
(3) We are looking for short (~500 words) pathology related educational articles to be included on our monthly Feature Page. This could be part of a presentation you have already given. Contact us with your ideas, if interested.
Visit and follow our Blog to see recent updates to the website.
Case #215
Clinical history:
A 2 year old boy from El Paso was in good health until he began experiencing mild rhinorrhea and cough, followed by acute onset of left sided weakness. Lumbar puncture revealed a pleocytosis of 111 WBC. MRI revealed diffuse contrast enhancing lesions with surrounding edema throughout the bilateral cortex, midbrain, pons and cerebellum, thought to be consistent with cysticerci. The patient was managed with albendazole therapy and intravenous steroids, and improved sufficiently to be discharged home. A week later, he worsened again and presented with hemiparesis, ataxia and inability to handle secretions. By MRI, the lesions had increased in size. Pertinent history includes regular travel to Mexico but no known sick contacts at home and no known TB in the family. A biopsy was performed.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Balamuthia mandrillaris encephalitis
Discussion:
The diagnosis was confirmed by PCR performed by the US Centers for Disease Control.
Balamuthia mandrilaris is an amoeba that primarily affects the nasal pyramid or the skin, producing granulomatous amoebic lesions (Hum Pathol 1999;30:269). The amoebae spread from the primary nasal lesion to the meninges, where they infiltrate vessels. Thrombotic amoebic angitis produces CNS infarcts, that are infiltrated by amoebae.
Balamuthia infection is extremely rare, with fewer than 200 human cases recognized worldwide since it was found to be a human pathogen in 1990. Balamuthia is often misdiagnosed as other neurologic diseases (Clin Infect Dis 2009;48:879). Infection occurs in both immunocompromised and otherwise healthy persons and often in children. Risk factors are poorly defined, but might include exposure to soil or stagnant water, young age and Hispanic ethnicity. Balamuthia can also be transmitted by organ transplant (MMWR Morb Mortal Wkly Rep 2010;59:1165).
Clinically, patients can have skin lesions months to years before having encephalitis symptoms. At biopsy, an amoebic trophozoite is observed, often infiltrating vessels. The amoebae have a nucleus with a large, central karyosome and vacuolated cytoplasm.
Once infection progresses to encephalitis, it is almost always fatal, although a few patients have survived (Clin Infect Dis 2010;51:e7, Pediatrics 2010;125:e699).
Differential diagnosis includes other amoebae that attack the CNS, including Acanthamoeba, Naegleria fowleri and Sappinia, which have microscopic differences in the cysts and trophozoites. In this case, the 2 year old boy died of his disease and no autopsy was performed.
Reference: CDC: Free Living Amebic Infections [Accessed 14 May 2024]