24 August 2011 - Case #214
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Jessica Kozel, University of Missiouri and Dr. Leon Barnes, University of Pittsburgh (USA).
CancerTYPE ID is a standardized, objective molecular test based on the differential expression of 92 genes, that classifies tumors by matching the gene expression pattern of a patients tumor tissue to a database of known tumor types and histological subtypes.
CancerTYPE IDs database includes 2,206 tumors from multiple tumor banks, selected to provide broader and deeper representation of the heterogeneity of tumors. The 92-gene assay does not overlap with IHC markers, providing complementary data to standard tumor diagnosis.
CancerTYPE ID uses real-time reverse transcription polymerase chain reaction (RT-PCR). A very low copy number of RNA molecules can be detected, thus reducing the sample tissue required for testing. Testing is conducted and results are generated at bioTheranostics' CAP-accredited, CLIA-certified laboratory.
Advertisment
Case #214
Clinical history:
A 44 year old man had a parotid gland mass, which was excised.
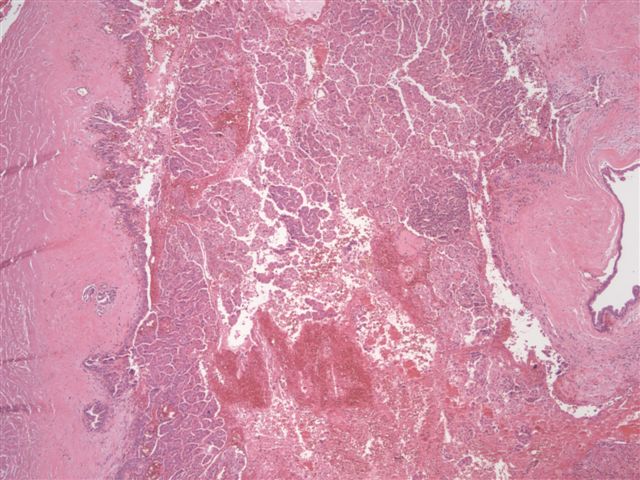
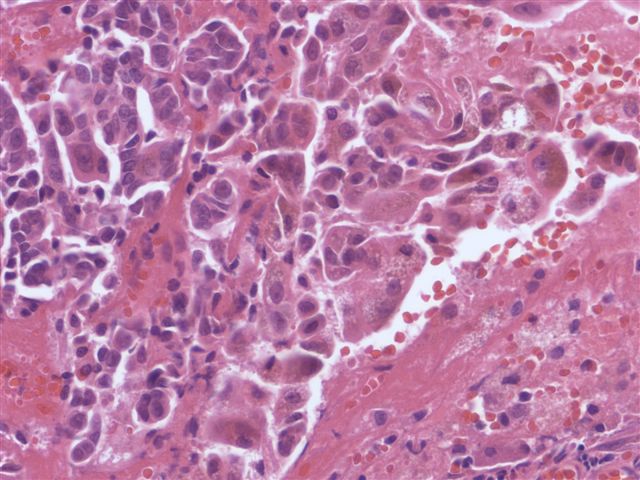
Microscopic images:
What is your diagnosis?
Diagnosis: Low grade cribriform cystadenocarcinoma
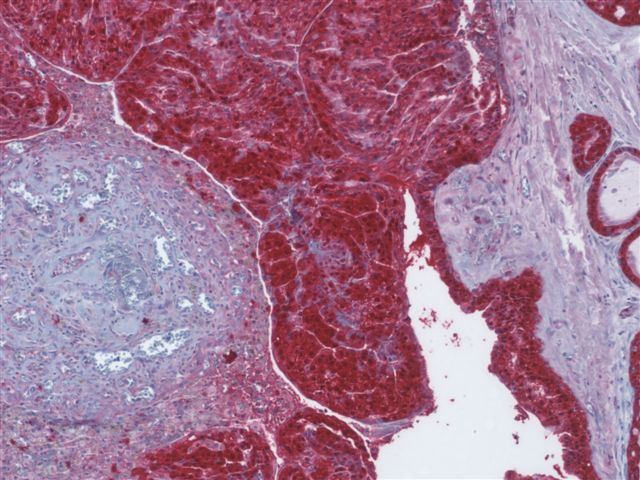
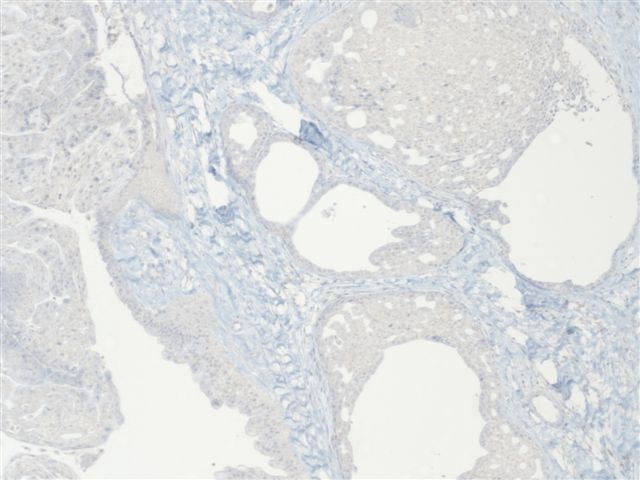
Immunostains:
Discussion:
Low grade cribriform cystadenocarcinoma (LGCCC) is a rare salivary gland tumor with a striking resemblance to atypical ductal hyperplasia and ductal carcinoma in situ of the breast and an excellent prognosis (Cancer 1996;78:958, Am J Surg Pathol 2004;28:1040). It also been called low grade salivary duct carcinoma, but this designation was abandoned in the WHO classification to avoid confusion with salivary duct carcinoma, which has a very poor prognosis. However, some authors believe there may be overlap because there are reported cases with adjacent high grade salivary duct carcinoma.
This tumor is now listed as a variant of cystadenocarcinoma. There is a female predominance and most patients are elderly. All but one reported case have occurred in the parotid gland.
Histologically, the tumor is unencapsulated and composed of single or multiple cysts with an intraductal proliferation. The cystic cavity is lined with cytologically bland apocrine ductal cells. The intraductal proliferation has a cribriform pattern with sieve-like spaces similar to breast proliferations. The majority of the tumor is intraductal; however, small areas of invasion may be present. The ductal cells have PAS positive / diastase resistant microvacuoles and yellow-brown, lipofuscin-like pigment. There is often associated hemorrhage, cholesterol clefts and hemosiderin laden macrophages due to cyst rupture.
LGCCC demonstrates strong diffuse S100 staining. Myoepithelial markers including p63, calponin and calmodulin decorate the flat cells lining the cystic spaces. If there are areas of invasion, the myoepithelial cells are typically absent. In contrast to salivary duct carcinoma, LGCCC is negative for HER2 / Neu and androgen receptor staining.
Differential diagnosis includes the papillary cystic variant of acinic cell carcinoma, which characteristically lacks the yellow-brown pigment and has finer PAS positive microvacuoles. Another differential consideration is cystadenocarcinoma, which has a more invasive growth pattern and lacks a prominent intraductal component.
Low grade cribriform cystadenocarcinoma has an excellent prognosis with no reported recurrences.
References: IARC: Pathology and Genetics of Head and Neck Tumours, 1st Edition, 2005
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Jessica Kozel, University of Missiouri and Dr. Leon Barnes, University of Pittsburgh (USA).
CancerTYPE ID is a standardized, objective molecular test based on the differential expression of 92 genes, that classifies tumors by matching the gene expression pattern of a patients tumor tissue to a database of known tumor types and histological subtypes.
CancerTYPE IDs database includes 2,206 tumors from multiple tumor banks, selected to provide broader and deeper representation of the heterogeneity of tumors. The 92-gene assay does not overlap with IHC markers, providing complementary data to standard tumor diagnosis.
CancerTYPE ID uses real-time reverse transcription polymerase chain reaction (RT-PCR). A very low copy number of RNA molecules can be detected, thus reducing the sample tissue required for testing. Testing is conducted and results are generated at bioTheranostics' CAP-accredited, CLIA-certified laboratory.
Website news:
(1) We have updated the Chronic Myeloid Neoplasms chapter based on a review by Nikhil Sangle, M.D., FRCPath.(Engl.), University of Utah Health Sciences Center and ARUP Laboratories.
(2) We are looking for good grossing videos to add to our online textbook. If you know of any that we can use, or are interested in creating one, please contact us.
Visit and follow our Blog to see recent updates to the website.
(1) We have updated the Chronic Myeloid Neoplasms chapter based on a review by Nikhil Sangle, M.D., FRCPath.(Engl.), University of Utah Health Sciences Center and ARUP Laboratories.
(2) We are looking for good grossing videos to add to our online textbook. If you know of any that we can use, or are interested in creating one, please contact us.
Visit and follow our Blog to see recent updates to the website.
Case #214
Clinical history:
A 44 year old man had a parotid gland mass, which was excised.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Low grade cribriform cystadenocarcinoma
Immunostains:
Discussion:
Low grade cribriform cystadenocarcinoma (LGCCC) is a rare salivary gland tumor with a striking resemblance to atypical ductal hyperplasia and ductal carcinoma in situ of the breast and an excellent prognosis (Cancer 1996;78:958, Am J Surg Pathol 2004;28:1040). It also been called low grade salivary duct carcinoma, but this designation was abandoned in the WHO classification to avoid confusion with salivary duct carcinoma, which has a very poor prognosis. However, some authors believe there may be overlap because there are reported cases with adjacent high grade salivary duct carcinoma.
This tumor is now listed as a variant of cystadenocarcinoma. There is a female predominance and most patients are elderly. All but one reported case have occurred in the parotid gland.
Histologically, the tumor is unencapsulated and composed of single or multiple cysts with an intraductal proliferation. The cystic cavity is lined with cytologically bland apocrine ductal cells. The intraductal proliferation has a cribriform pattern with sieve-like spaces similar to breast proliferations. The majority of the tumor is intraductal; however, small areas of invasion may be present. The ductal cells have PAS positive / diastase resistant microvacuoles and yellow-brown, lipofuscin-like pigment. There is often associated hemorrhage, cholesterol clefts and hemosiderin laden macrophages due to cyst rupture.
LGCCC demonstrates strong diffuse S100 staining. Myoepithelial markers including p63, calponin and calmodulin decorate the flat cells lining the cystic spaces. If there are areas of invasion, the myoepithelial cells are typically absent. In contrast to salivary duct carcinoma, LGCCC is negative for HER2 / Neu and androgen receptor staining.
Differential diagnosis includes the papillary cystic variant of acinic cell carcinoma, which characteristically lacks the yellow-brown pigment and has finer PAS positive microvacuoles. Another differential consideration is cystadenocarcinoma, which has a more invasive growth pattern and lacks a prominent intraductal component.
Low grade cribriform cystadenocarcinoma has an excellent prognosis with no reported recurrences.
References: IARC: Pathology and Genetics of Head and Neck Tumours, 1st Edition, 2005