29 July 2011 - Case #211
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Ashish Bansal, Betsi Cadwaladr University Health Board (North Wales, U.K.), for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
CancerTYPE ID is a standardized, objective molecular test based on the differential expression of 92 genes, that classifies tumors by matching the gene expression pattern of a patients tumor tissue to a database of known tumor types and histological subtypes.
CancerTYPE IDs database includes 2,206 tumors from multiple tumor banks, selected to provide broader and deeper representation of the heterogeneity of tumors. The 92-gene assay does not overlap with IHC markers, providing complementary data to standard tumor diagnosis.
CancerTYPE ID uses real-time reverse transcription polymerase chain reaction (RT-PCR). A very low copy number of RNA molecules can be detected, thus reducing the sample tissue required for testing. Testing is conducted and results are generated at bioTheranostics' CAP-accredited, CLIA-certified laboratory.
Advertisement
Case #211
Clinical history:
A 57 year old woman presented with post-menopausal bleeding. An endometrial polyp was removed piecemeal at hysteroscopy, the largest fragment was 18 mm.
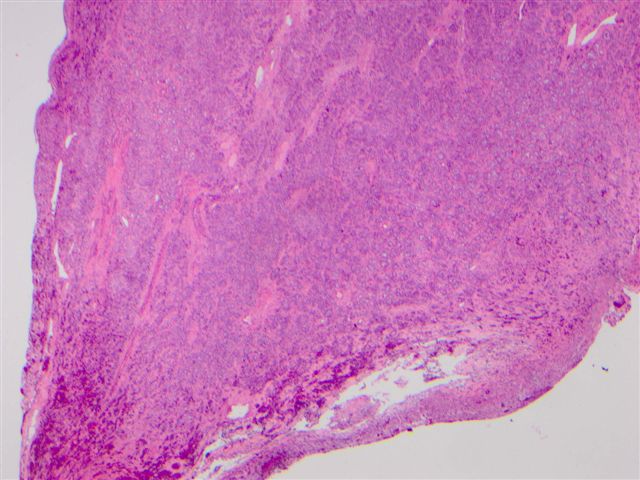
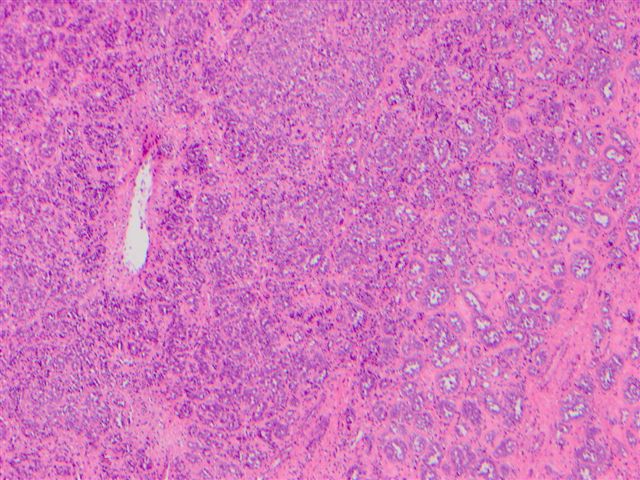
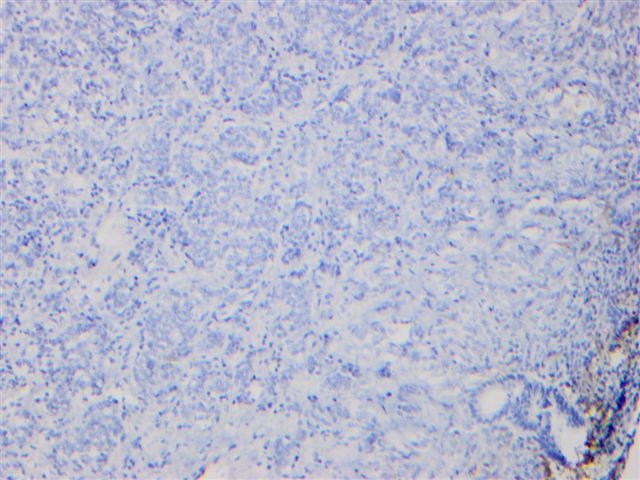
Microscopic images:
What is your diagnosis?
Diagnosis: Uterine tumour resembling ovarian sex cord tumors (UTROSCT)
Discussion:
Tumors of the uterus resembling ovarian sex cord tumors were first described by Clement and Scully (Am J Clin Pathol 1976;66:512). They are divided into 2 groups. Group 1: endometrial stromal tumors with sex cord-like elements (ESTSCLE) now referred to as endometrial stromal sarcoma with sex cord-like differentiation. Group 2: uterine tumor resembling ovarian sex cord tumor (UTROSCT). In group 1 tumors, the sex cord component constitutes a minor portion of an endometrial stromal neoplasm. In group 2 tumors, it is the predominant or exclusive component of a uterine wall lesion composed of various mesenchymal elements.
UTROSCT generally arise in the fourth to sixth decade of life. Grossly, they are polypoid or nodular, typically in the myometrium. Histologically, they are well circumscribed, polyphenotypic neoplasms, with a predominant, if not exclusive, pattern of cords, nests and trabeculae containing epitheloid cells resembling granulosa or Sertoli cell tumors of the ovary. True Leydig cell differentiation is rare (Mod Pathol 2006;19:17).
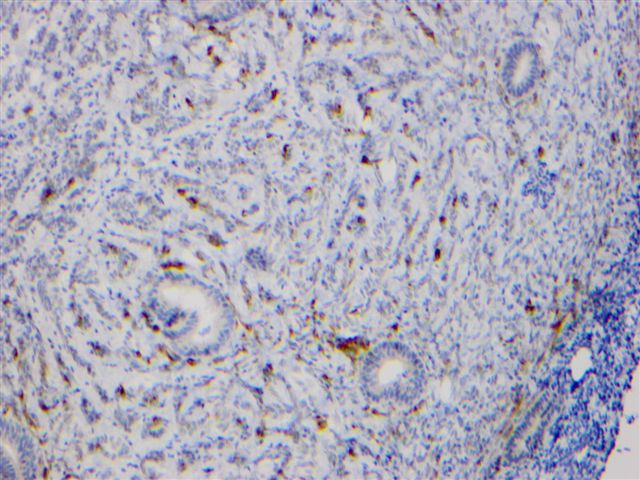
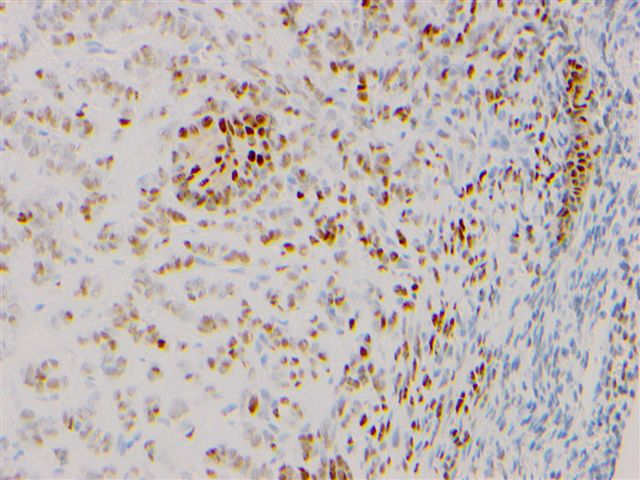
These tumors typically express at least 2 sex cord markers of calretinin, inhibin, CD99 and MelanA, although a recent study substituting WT1 for CD99 found less frequent immunoreactivity (Int J Gynecol Pathol 2008;27:229, Am J Surg Pathol 2010;34:1749). They also express myoid markers, epithelial markers and hormone receptors.
The origin of these tumors is uncertain. They may derive from an uncommitted cell with the capacity to differentiate along several lines (J Clin Pathol 2007;60:1148). Although these tumors often express smooth muscle markers, there are no ultrastructural features of smooth muscle differentiation (Ultrastruct Pathol 2010;34:16). Although they resemble ESTSCLE, they lack the JAZF1::JJAZ1 translocation frequently associated with endometrial stromal tumors (Am J Surg Pathol 2009;33:1206).
The differential diagnosis includes metastatic ovarian sex cord tumors (different clinical history) and mixed Müllerian tumors. If one inappropriately focuses on immunohistochemistry results, an erroneous diagnosis of a myoid tumor (such as vascular plexiform leiomyoma) or an epithelial tumor may occur (Ann Diagn Pathol 2010;14:355).
Excision by hysterectomy is usually curative, although some recommend fertility sparing surgery in select patients, with careful follow up. Tumors of the uterus resembling ovarian sex cord tumors typically have benign behavior, although metastases have rarely been reported (Gynecol Oncol 2009;114:140, Int J Gynecol Pathol 2008;27:58).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Ashish Bansal, Betsi Cadwaladr University Health Board (North Wales, U.K.), for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
CancerTYPE ID is a standardized, objective molecular test based on the differential expression of 92 genes, that classifies tumors by matching the gene expression pattern of a patients tumor tissue to a database of known tumor types and histological subtypes.
CancerTYPE IDs database includes 2,206 tumors from multiple tumor banks, selected to provide broader and deeper representation of the heterogeneity of tumors. The 92-gene assay does not overlap with IHC markers, providing complementary data to standard tumor diagnosis.
CancerTYPE ID uses real-time reverse transcription polymerase chain reaction (RT-PCR). A very low copy number of RNA molecules can be detected, thus reducing the sample tissue required for testing. Testing is conducted and results are generated at bioTheranostics' CAP-accredited, CLIA-certified laboratory.
Website news:
(1) Our Buyer's Guide - Feature Page for July highlights Imaging / digital / photography, and includes Celestron, Leica, Milestone Medical, Olive Tree Media LLC, Optronics, Photodyne and SPOT Imaging Solutions.
(2) We are looking for reviewers for part/all of these chapters: Coagulation, Salivary Glands, Stains, Uterus; also Fallopian Tubes, Lung-tumor, Ureters, Urethra, Vagina, Vulva.
(3) We have now updated the Bladder chapter.
Visit and follow our Blog to see recent updates to the website.
(1) Our Buyer's Guide - Feature Page for July highlights Imaging / digital / photography, and includes Celestron, Leica, Milestone Medical, Olive Tree Media LLC, Optronics, Photodyne and SPOT Imaging Solutions.
(2) We are looking for reviewers for part/all of these chapters: Coagulation, Salivary Glands, Stains, Uterus; also Fallopian Tubes, Lung-tumor, Ureters, Urethra, Vagina, Vulva.
(3) We have now updated the Bladder chapter.
Visit and follow our Blog to see recent updates to the website.
Case #211
Clinical history:
A 57 year old woman presented with post-menopausal bleeding. An endometrial polyp was removed piecemeal at hysteroscopy, the largest fragment was 18 mm.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Uterine tumour resembling ovarian sex cord tumors (UTROSCT)
Discussion:
Tumors of the uterus resembling ovarian sex cord tumors were first described by Clement and Scully (Am J Clin Pathol 1976;66:512). They are divided into 2 groups. Group 1: endometrial stromal tumors with sex cord-like elements (ESTSCLE) now referred to as endometrial stromal sarcoma with sex cord-like differentiation. Group 2: uterine tumor resembling ovarian sex cord tumor (UTROSCT). In group 1 tumors, the sex cord component constitutes a minor portion of an endometrial stromal neoplasm. In group 2 tumors, it is the predominant or exclusive component of a uterine wall lesion composed of various mesenchymal elements.
UTROSCT generally arise in the fourth to sixth decade of life. Grossly, they are polypoid or nodular, typically in the myometrium. Histologically, they are well circumscribed, polyphenotypic neoplasms, with a predominant, if not exclusive, pattern of cords, nests and trabeculae containing epitheloid cells resembling granulosa or Sertoli cell tumors of the ovary. True Leydig cell differentiation is rare (Mod Pathol 2006;19:17).
These tumors typically express at least 2 sex cord markers of calretinin, inhibin, CD99 and MelanA, although a recent study substituting WT1 for CD99 found less frequent immunoreactivity (Int J Gynecol Pathol 2008;27:229, Am J Surg Pathol 2010;34:1749). They also express myoid markers, epithelial markers and hormone receptors.
The origin of these tumors is uncertain. They may derive from an uncommitted cell with the capacity to differentiate along several lines (J Clin Pathol 2007;60:1148). Although these tumors often express smooth muscle markers, there are no ultrastructural features of smooth muscle differentiation (Ultrastruct Pathol 2010;34:16). Although they resemble ESTSCLE, they lack the JAZF1::JJAZ1 translocation frequently associated with endometrial stromal tumors (Am J Surg Pathol 2009;33:1206).
The differential diagnosis includes metastatic ovarian sex cord tumors (different clinical history) and mixed Müllerian tumors. If one inappropriately focuses on immunohistochemistry results, an erroneous diagnosis of a myoid tumor (such as vascular plexiform leiomyoma) or an epithelial tumor may occur (Ann Diagn Pathol 2010;14:355).
Excision by hysterectomy is usually curative, although some recommend fertility sparing surgery in select patients, with careful follow up. Tumors of the uterus resembling ovarian sex cord tumors typically have benign behavior, although metastases have rarely been reported (Gynecol Oncol 2009;114:140, Int J Gynecol Pathol 2008;27:58).