3 June 2011 - Case #208
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Javier Ortiz, Pablo Sousa, Margarita Lopez Candocia, Marta Rodriguez, and Agustn Bullin, Hospital Universitario de Salamanca and Hospital Virgen Vega de Salamanca, Spain.

AccuCore Group invites you to a free 45 minute webinar:
Best Practices for Anatomic Pathology Quality Management
June 16th at 12:00pm Eastern
Webinar Agenda:
Sponsored by AccuPathology: Pathology Quality Management Software
AccuCore Group
(267) 564-5015
http://www.accucoregroup.com
Advertisement
Case #208
Clinical history:
A 66 year old man was admitted for the subacute onset of mild disequilibrium and vertigo. He had a previous history of peptic ulcer and smoking. CT scan and MRI revealed a well defined solid mass lesion in the fourth ventricle extending into the foramen magnum. Clinical testing for metastatic disease was negative.
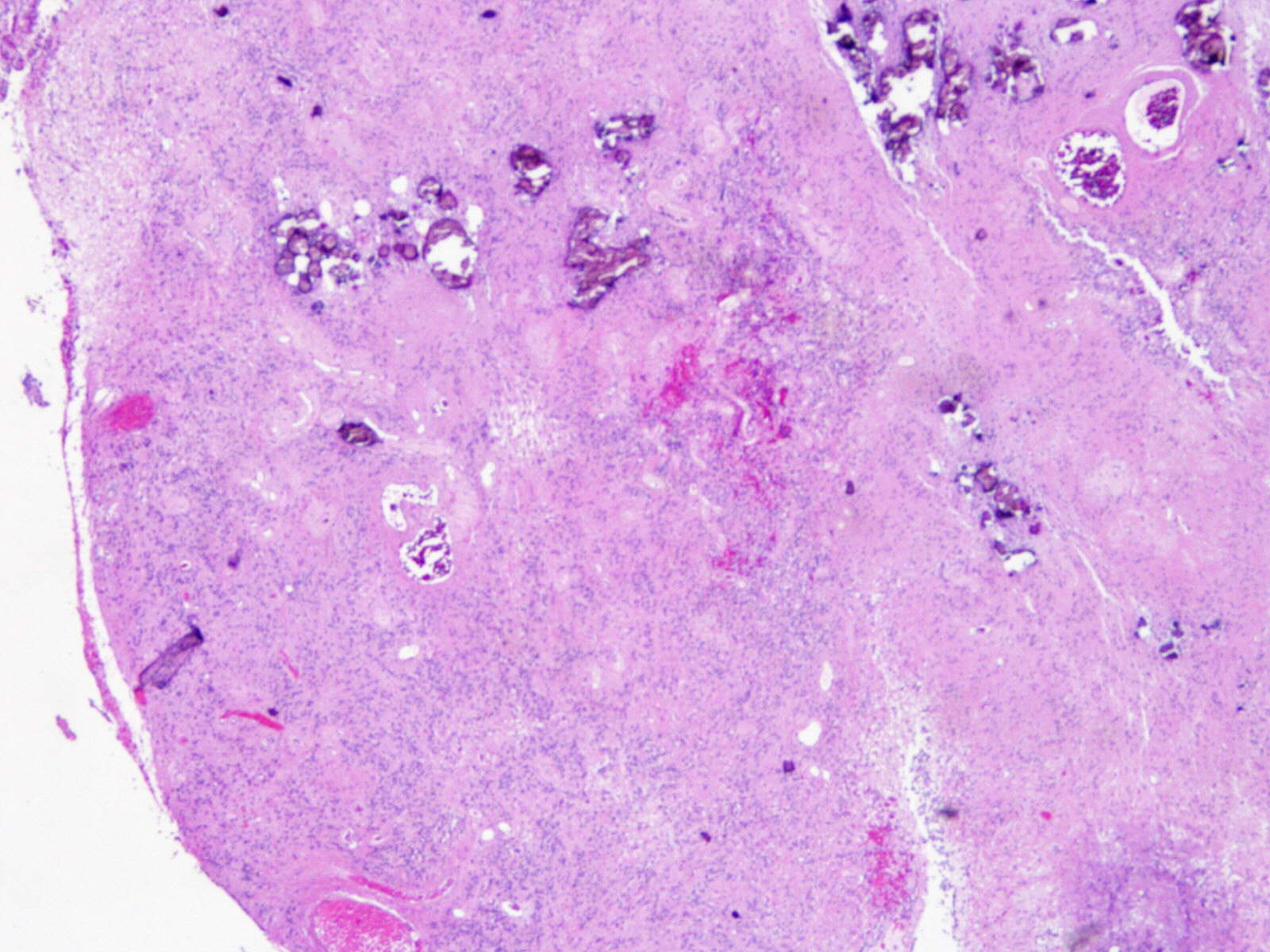
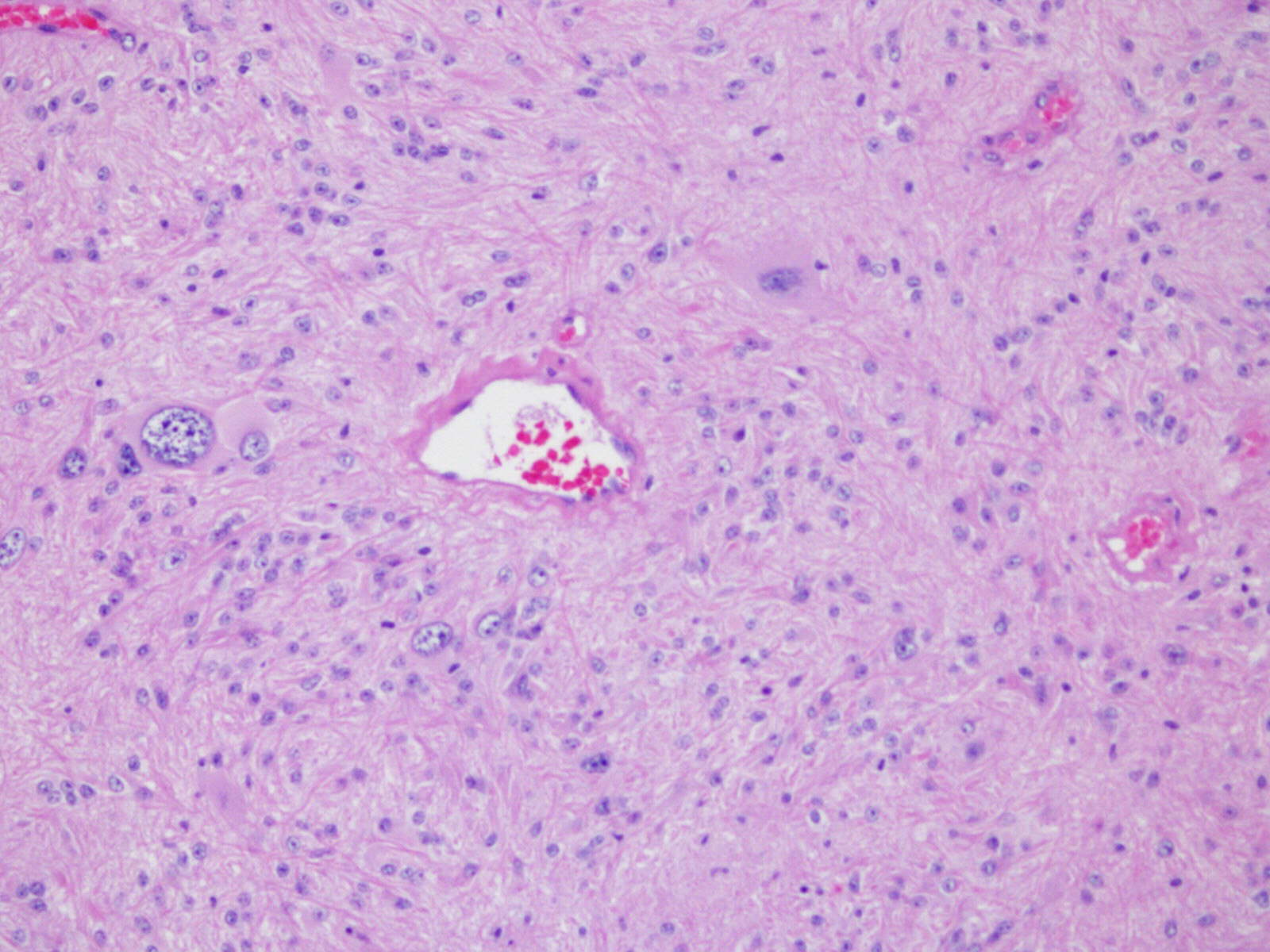
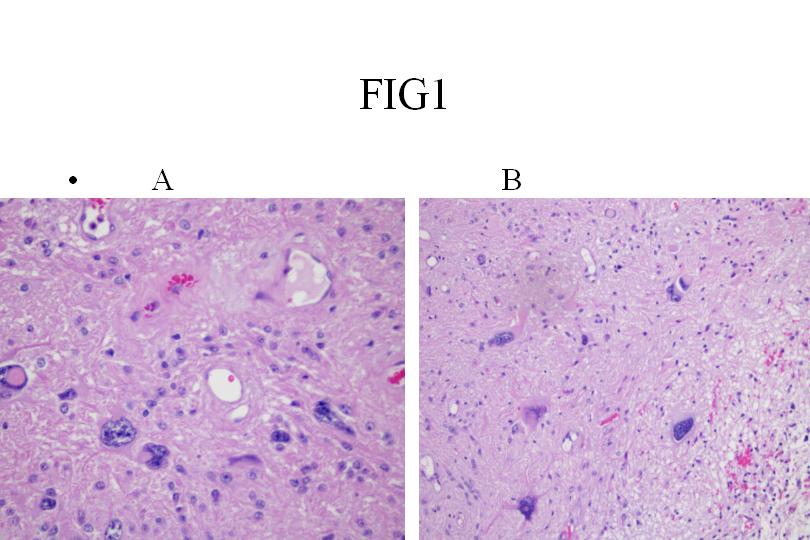
Microscopic images:
What is your diagnosis?
Diagnosis: Giant cell ependymoma
Discussion:
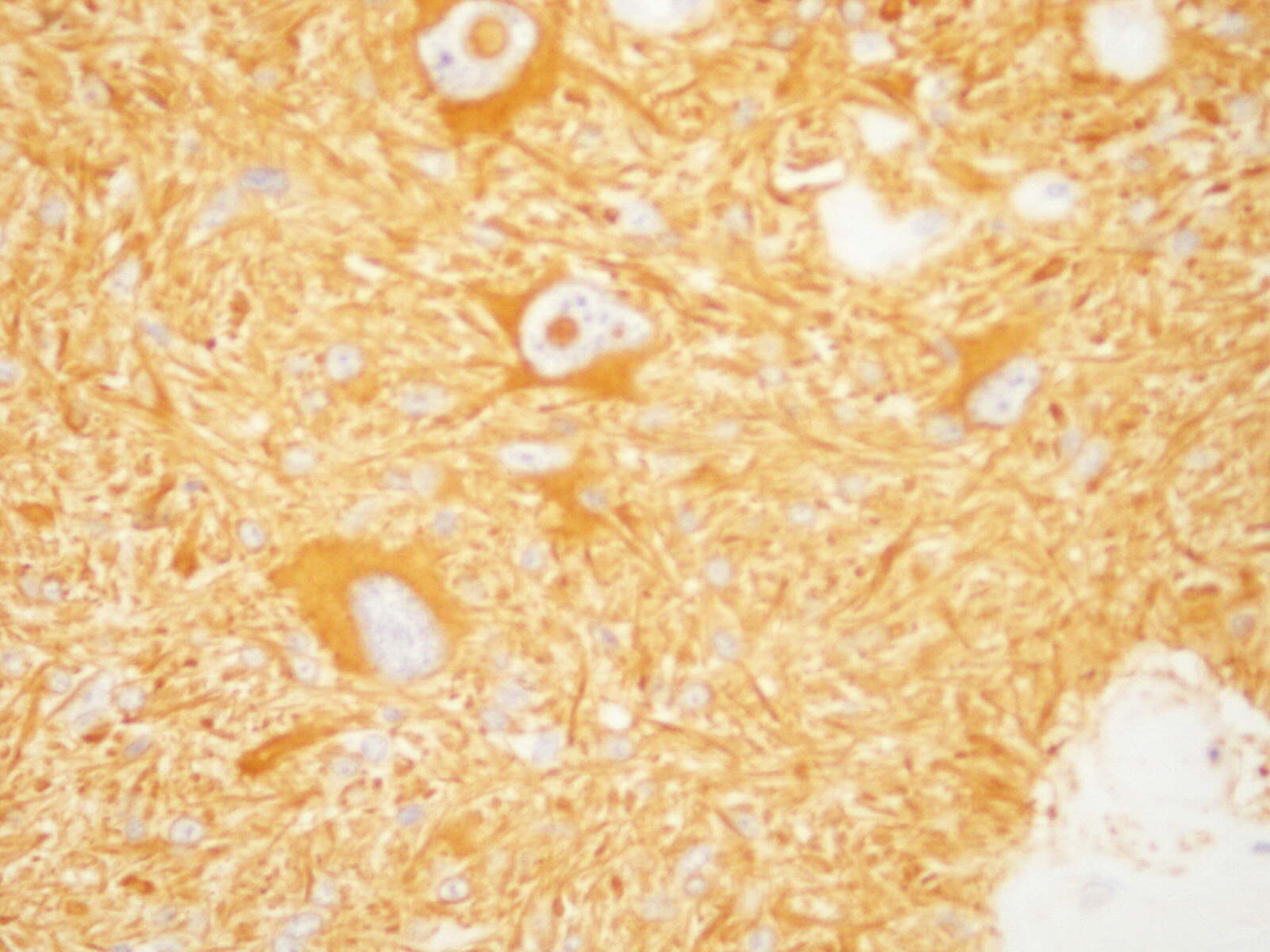
Histological examination showed a neoplasm with unipolar processes extending from elongated tumor cells toward blood vessels in perivascular rosettes, typical of ependymoma. Multiple giant tumor cells are also present, usually with well defined borders, eosinophilic cytoplasm and bizarre, hyperchromatic nuclei. No areas of vascular proliferation, glomeruli-like structures or necrosis were seen. The tumor cells had low proliferative activity by Ki67 staining (< 1%). Most tumor cells (classic ependymoma and giant cells) were strongly immunoreactive for GFAP and negative for epithelial (AE1 / AE3 and CAM5.2), melanocytic (HMB45 and MelanA) and histiocytic markers (CD68). There was focal perinculear staining for EMA. In contrast to previous reports, inmunostaining for CD99 was not observed in this case (Medscape J Med 2008;10:41). The reticulin stain showed minimal reticular architecture, in agreement with the soft appearance of the neoplasm.
This uncommon ependymoma variant can occur throughout the neuraxis, with some preference for filum terminale and spinal cord. Histologically, it is characterized by bizarre giant cells coexisting with areas of typical ependymoma (Folia Neuropathol 2008;46:220, Eur Spine J 2009;18 Suppl 2:186, Brain Tumor Pathol 2009;26:79).
The differential diagnosis of giant cell ependymoma includes not only anaplastic ependymoma and other glial lesions (pleomorphic xanthoastrocytoma and giant cell astrocytoma) but also nonglial neoplasms that may show bizarre tumor cells, including schwannoma, fibrous histiocytoma, metastatic carcinoma and metastatic melanoma.
This case did not satisfy the WHO criteria for anaplastic ependymoma, due to the absence of increased cellularity, brisk mitotic activity, microvascular proliferation and pseudopalisading necrosis. Features inconsistent with pleomorphic xanthoastrocytoma include this tumor's infratentorial location, scarce reticulin pattern and the absence of intracellular lipidic material. Giant cell astrocytoma is associated with tuberous sclerosis and has cells resembling ganglion cells (Neuropathology 2009;29:181). Schwannomas are S100 positive and GFAP negative. Melanomas are positive for HMB45 and MelanA and metastatic carcinoma is positive for keratins (Hum Pathol 2009;40:578, Neuropathology 2010;30:71).
Despite the apparent anaplastic appearance, giant cell ependymoma usually shows a behavior similar to other WHO grade II ependymomas. This patient was disease free 18 months postsurgery.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Javier Ortiz, Pablo Sousa, Margarita Lopez Candocia, Marta Rodriguez, and Agustn Bullin, Hospital Universitario de Salamanca and Hospital Virgen Vega de Salamanca, Spain.

Best Practices for Anatomic Pathology Quality Management
June 16th at 12:00pm Eastern
Webinar Agenda:
- Anatomic Pathology issues and needs around QA and Peer Review
- External Demands: Standards Bodies (CAP and The Joint Commission) compliance
- Internal Demands: CMOs, Regulatory Affairs and PI demands for quality data
- Accurate Peer Reviews: Vetted details and automation
- QA for PAs, Histotechs, Transcriptionists, etc.
- Optimize your ability to provide accurate and timely diagnoses while improving QA
- Pathology Quality and Peer Review Mgmt. Best Practice: Example
- Discussion
Sponsored by AccuPathology: Pathology Quality Management Software
AccuCore Group
(267) 564-5015
http://www.accucoregroup.com
Website news:
(1) Congratulations to Dr. Pelin Bagci, Emory University (Atlanta, Georgia) and Dr. Teresita Zdunek, St. Joseph Hospital (Chicago, Illinois) for winning our Promotions contest. Each received a $25 Amazon.com gift card.
(2) For a "printer friendly page" of any part of our website, we recommend visiting http://www.printfriendly.com, which has options to print with or without images. As this works better than our "printer friendly" versions of chapters, we are removing the printer friendly versions as we update each chapter.
Visit and follow our Blog to see recent updates to the website.
(1) Congratulations to Dr. Pelin Bagci, Emory University (Atlanta, Georgia) and Dr. Teresita Zdunek, St. Joseph Hospital (Chicago, Illinois) for winning our Promotions contest. Each received a $25 Amazon.com gift card.
(2) For a "printer friendly page" of any part of our website, we recommend visiting http://www.printfriendly.com, which has options to print with or without images. As this works better than our "printer friendly" versions of chapters, we are removing the printer friendly versions as we update each chapter.
Visit and follow our Blog to see recent updates to the website.
Case #208
Clinical history:
A 66 year old man was admitted for the subacute onset of mild disequilibrium and vertigo. He had a previous history of peptic ulcer and smoking. CT scan and MRI revealed a well defined solid mass lesion in the fourth ventricle extending into the foramen magnum. Clinical testing for metastatic disease was negative.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Giant cell ependymoma
Discussion:
Histological examination showed a neoplasm with unipolar processes extending from elongated tumor cells toward blood vessels in perivascular rosettes, typical of ependymoma. Multiple giant tumor cells are also present, usually with well defined borders, eosinophilic cytoplasm and bizarre, hyperchromatic nuclei. No areas of vascular proliferation, glomeruli-like structures or necrosis were seen. The tumor cells had low proliferative activity by Ki67 staining (< 1%). Most tumor cells (classic ependymoma and giant cells) were strongly immunoreactive for GFAP and negative for epithelial (AE1 / AE3 and CAM5.2), melanocytic (HMB45 and MelanA) and histiocytic markers (CD68). There was focal perinculear staining for EMA. In contrast to previous reports, inmunostaining for CD99 was not observed in this case (Medscape J Med 2008;10:41). The reticulin stain showed minimal reticular architecture, in agreement with the soft appearance of the neoplasm.
This uncommon ependymoma variant can occur throughout the neuraxis, with some preference for filum terminale and spinal cord. Histologically, it is characterized by bizarre giant cells coexisting with areas of typical ependymoma (Folia Neuropathol 2008;46:220, Eur Spine J 2009;18 Suppl 2:186, Brain Tumor Pathol 2009;26:79).
The differential diagnosis of giant cell ependymoma includes not only anaplastic ependymoma and other glial lesions (pleomorphic xanthoastrocytoma and giant cell astrocytoma) but also nonglial neoplasms that may show bizarre tumor cells, including schwannoma, fibrous histiocytoma, metastatic carcinoma and metastatic melanoma.
This case did not satisfy the WHO criteria for anaplastic ependymoma, due to the absence of increased cellularity, brisk mitotic activity, microvascular proliferation and pseudopalisading necrosis. Features inconsistent with pleomorphic xanthoastrocytoma include this tumor's infratentorial location, scarce reticulin pattern and the absence of intracellular lipidic material. Giant cell astrocytoma is associated with tuberous sclerosis and has cells resembling ganglion cells (Neuropathology 2009;29:181). Schwannomas are S100 positive and GFAP negative. Melanomas are positive for HMB45 and MelanA and metastatic carcinoma is positive for keratins (Hum Pathol 2009;40:578, Neuropathology 2010;30:71).
Despite the apparent anaplastic appearance, giant cell ependymoma usually shows a behavior similar to other WHO grade II ependymomas. This patient was disease free 18 months postsurgery.