21 February 2008 - Case #111
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Moneil Patel, New York Medical College (USA).
Case #111
Clinical history:
A 71 year old man with a past medical history of hypertension presented with lower back pain. An MRI showed a T12 / L1 intradural tumor. The operative report described the mass as a gray vascular tumor that was mobile and attached to the filum terminale.
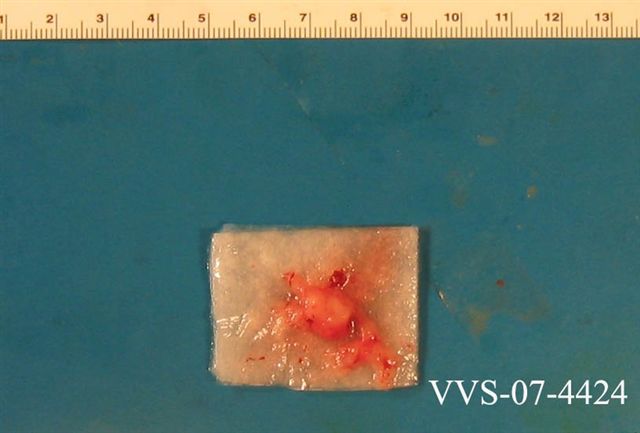
Gross image:
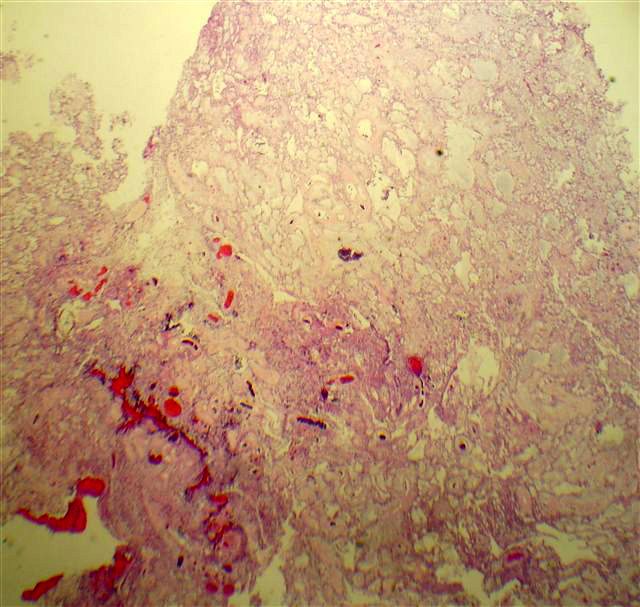
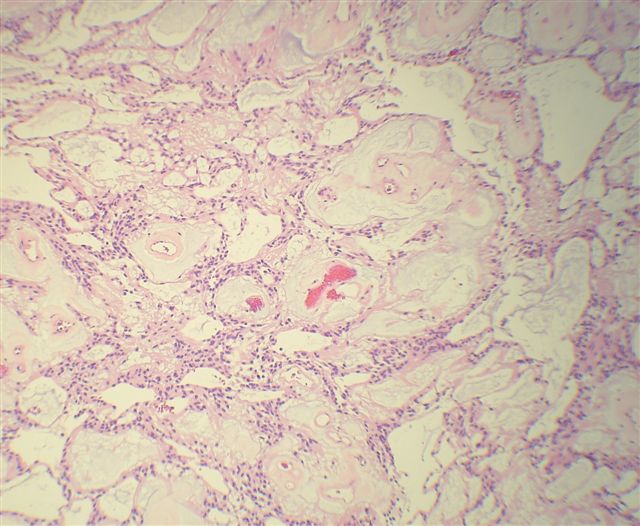
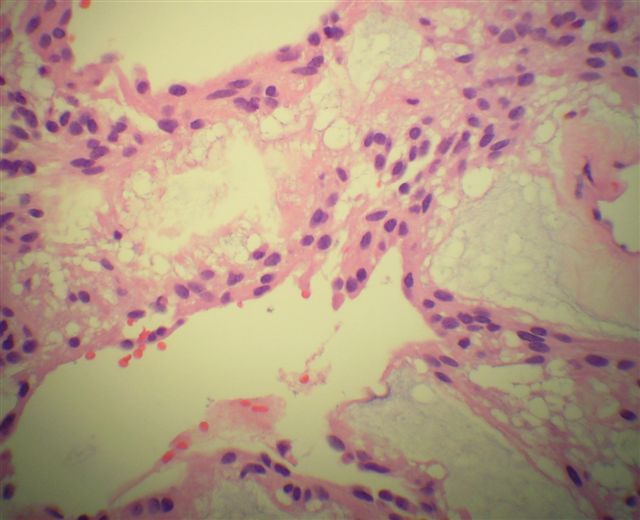
Microscopic images:
What is your diagnosis?
Diagnosis: Myxopapillary ependymoma
Discussion:
Myxopapillary ependymoma is a low grade tumor that typically occurs in the filum terminale, cauda equina, sacrum or adjacent soft tissue. It is considered grade I of IV (WHO) at these sites and grade II in the brain and spinal cord proper. However intracranial primaries are very rare (Neurosurgery 2004;55:981).
These tumors have a characteristic myxopapillary appearance with bland oval ependymal cells surrounding pseudopapilllary structures of myxoid material, with occasional central vessels. The neoplastic cells may also appear elongated with a glial quality and these tumors may resemble schwannoma.
The mucin is highlighted by PAS or Alcian blue. The tumor cells are GFAP and S100 positive. They are negative for cytokeratins.
The differential diagnosis includes chordoma (see Case #110), which has cords and lobules of bubbly physaliferous cells, which are keratin positive and GFAP negative. Some cases may resemble schwannoma focally, which is mucin negative.
Most myxopapillary ependymomas can be totally resected by severing the filum terminale from its origin and dissecting along nerve roots and gross total resection may be the most predictive factor for outcome (Clin Neuropathol 2008;27:21). However, incomplete removal may cause local or widespread dissemination and distant metastases.
References: Radiographics 2006;26 Suppl 1:S111
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Moneil Patel, New York Medical College (USA).
Case #111
Clinical history:
A 71 year old man with a past medical history of hypertension presented with lower back pain. An MRI showed a T12 / L1 intradural tumor. The operative report described the mass as a gray vascular tumor that was mobile and attached to the filum terminale.
Gross image:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Myxopapillary ependymoma
Discussion:
Myxopapillary ependymoma is a low grade tumor that typically occurs in the filum terminale, cauda equina, sacrum or adjacent soft tissue. It is considered grade I of IV (WHO) at these sites and grade II in the brain and spinal cord proper. However intracranial primaries are very rare (Neurosurgery 2004;55:981).
These tumors have a characteristic myxopapillary appearance with bland oval ependymal cells surrounding pseudopapilllary structures of myxoid material, with occasional central vessels. The neoplastic cells may also appear elongated with a glial quality and these tumors may resemble schwannoma.
The mucin is highlighted by PAS or Alcian blue. The tumor cells are GFAP and S100 positive. They are negative for cytokeratins.
The differential diagnosis includes chordoma (see Case #110), which has cords and lobules of bubbly physaliferous cells, which are keratin positive and GFAP negative. Some cases may resemble schwannoma focally, which is mucin negative.
Most myxopapillary ependymomas can be totally resected by severing the filum terminale from its origin and dissecting along nerve roots and gross total resection may be the most predictive factor for outcome (Clin Neuropathol 2008;27:21). However, incomplete removal may cause local or widespread dissemination and distant metastases.
References: Radiographics 2006;26 Suppl 1:S111