4 January 2008 - Case #106
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Drs. Angie M. Schultz and Paul F. Mellen, Ball Memorial Hospital, Muncie, Indiana (USA).

ARUP Laboratories First Annual Winter Update in Clinical and Laboratory Medicine is scheduled for March 3-7, 2008 at The Canyons, in Park City, Utah.
This 22.5 hour review and update in the areas of clinical chemistry, immunology, microbiology, and molecular medicine is intended to improve knowledge about the pathogenesis and clinical manifestations of a wide variety of metabolic infectious, immunologic, and genetic disorders along with the selection, performance, and interpretation of clinical laboratory tests.
This course will provide a forum for the exchange of ideas among clinicians, clinical and anatomic pathologists, and laboratory scientists on new developments diagnosing these disorders. Ample discussion time will be provided to address controversial issues.
Advertisement
Case #106
Clinical history:
At 35 weeks gestational age, this female fetus had evidence of intrauterine distress and underwent emergent delivery. The abdomen was markedly distended and the fetus did not survive delivery.
Autopsy showed a slightly large for gestational age, well developed fetus. The general external appearance was unremarkable except for abdominal distension. The placenta was unremarkable. The pertinent findings were limited to the abdominal cavity.
Gross images:
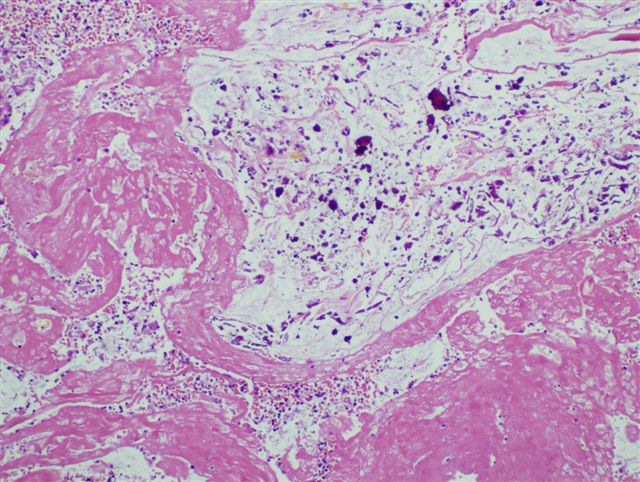
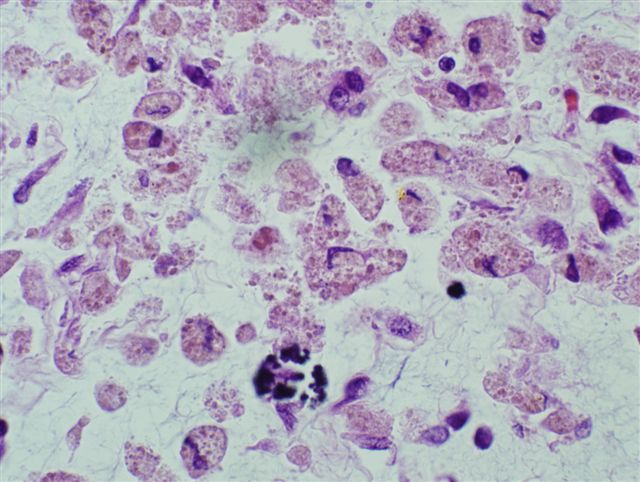
Microscopic images:
What is your diagnosis?
Diagnosis: Meconium peritonitis, associated with intrauterine small intestinal volvulus
Discussion:
Meconium peritonitis is a rare prenatal complication, occurring in 1 per 30,000 live births (Clin Radiol 1997;52:477). Gastrointestinal perforation releases meconium into the abdominal cavity, inducing a sterile inflammatory reaction and calcium deposition. Perforation may be due to meconium ileus, atresia, stenosis, internal hernia, Hirschprungs disease, volvulus, congenital bands, anoxia leading to bowel ischemia or idiopathic (J Perinatol 2000;3:193).
The presenting symptoms include fetal distress, maternal polyhydramnios, abdominal distention or a mass (JAMA 1953;152:582). Prenatal ultrasound shows bowel dilatation, ascites, polyhydramnios and intra-abdominal calcifications with acoustic shadowing (J Pediatr Surg 1995;30:979, Prenat Diagn 2005;25:676).
Grossly, there is an organized peritonitis with fibrosis, calcifications and dense intestinal adhesions. A fibrous wall, called a meconium pseudocyst, may form around the meconium (J Ultrasound Med 1982;1:333).
Microscopically, the peritoneal surface shows a fibrinous exudate with microcalcifications, bile pigment-like debris, histiocytes and chronic inflammatory cells.
Treatment for meconium peritonitis is surgical and prognosis varies greatly depending on pre versus postnatal diagnosis. Gestational age at diagnosis does not predict postnatal outcome (J Pediatr Surg 1995;30:979). However, some prenatal ultrasound findings have been shown to correlate with neonatal outcome in several studies (J Pediatr Surg 1995;30:979, Fetal Diagn Ther 2003;18:255, J Chin Med Assoc 2003;66:355, Prenat Diagn 2007;27:960).
Since patients in the Western hemisphere with meconium peritonitis often have cystic fibrosis and meconium ileus, newborns with this diagnosis should be evaluated for cystic fibrosis (Husain: Stocker and Dehner's Pediatric Pathology, 5th Edition, 2021, Pediatr Surg Int 2003;19:75).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Drs. Angie M. Schultz and Paul F. Mellen, Ball Memorial Hospital, Muncie, Indiana (USA).

ARUP Laboratories First Annual Winter Update in Clinical and Laboratory Medicine is scheduled for March 3-7, 2008 at The Canyons, in Park City, Utah.
This 22.5 hour review and update in the areas of clinical chemistry, immunology, microbiology, and molecular medicine is intended to improve knowledge about the pathogenesis and clinical manifestations of a wide variety of metabolic infectious, immunologic, and genetic disorders along with the selection, performance, and interpretation of clinical laboratory tests.
This course will provide a forum for the exchange of ideas among clinicians, clinical and anatomic pathologists, and laboratory scientists on new developments diagnosing these disorders. Ample discussion time will be provided to address controversial issues.
Case #106
Clinical history:
At 35 weeks gestational age, this female fetus had evidence of intrauterine distress and underwent emergent delivery. The abdomen was markedly distended and the fetus did not survive delivery.
Autopsy showed a slightly large for gestational age, well developed fetus. The general external appearance was unremarkable except for abdominal distension. The placenta was unremarkable. The pertinent findings were limited to the abdominal cavity.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Meconium peritonitis, associated with intrauterine small intestinal volvulus
Discussion:
Meconium peritonitis is a rare prenatal complication, occurring in 1 per 30,000 live births (Clin Radiol 1997;52:477). Gastrointestinal perforation releases meconium into the abdominal cavity, inducing a sterile inflammatory reaction and calcium deposition. Perforation may be due to meconium ileus, atresia, stenosis, internal hernia, Hirschprungs disease, volvulus, congenital bands, anoxia leading to bowel ischemia or idiopathic (J Perinatol 2000;3:193).
The presenting symptoms include fetal distress, maternal polyhydramnios, abdominal distention or a mass (JAMA 1953;152:582). Prenatal ultrasound shows bowel dilatation, ascites, polyhydramnios and intra-abdominal calcifications with acoustic shadowing (J Pediatr Surg 1995;30:979, Prenat Diagn 2005;25:676).
Grossly, there is an organized peritonitis with fibrosis, calcifications and dense intestinal adhesions. A fibrous wall, called a meconium pseudocyst, may form around the meconium (J Ultrasound Med 1982;1:333).
Microscopically, the peritoneal surface shows a fibrinous exudate with microcalcifications, bile pigment-like debris, histiocytes and chronic inflammatory cells.
Treatment for meconium peritonitis is surgical and prognosis varies greatly depending on pre versus postnatal diagnosis. Gestational age at diagnosis does not predict postnatal outcome (J Pediatr Surg 1995;30:979). However, some prenatal ultrasound findings have been shown to correlate with neonatal outcome in several studies (J Pediatr Surg 1995;30:979, Fetal Diagn Ther 2003;18:255, J Chin Med Assoc 2003;66:355, Prenat Diagn 2007;27:960).
Since patients in the Western hemisphere with meconium peritonitis often have cystic fibrosis and meconium ileus, newborns with this diagnosis should be evaluated for cystic fibrosis (Husain: Stocker and Dehner's Pediatric Pathology, 5th Edition, 2021, Pediatr Surg Int 2003;19:75).