1 November 2007 - Case #99
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Keloth E. Pradeep, Wrexham Maelor Hospital, United Kingdom.

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your client’s EMR systems securely and accurately.
For more information, contact www.lifepoint.com or call 866-LABTEST.
Advertisement
Case #99
Clinical history:
A 70 year old man had a calcified mediastinal mass on chest Xray. A core needle biopsy was taken.
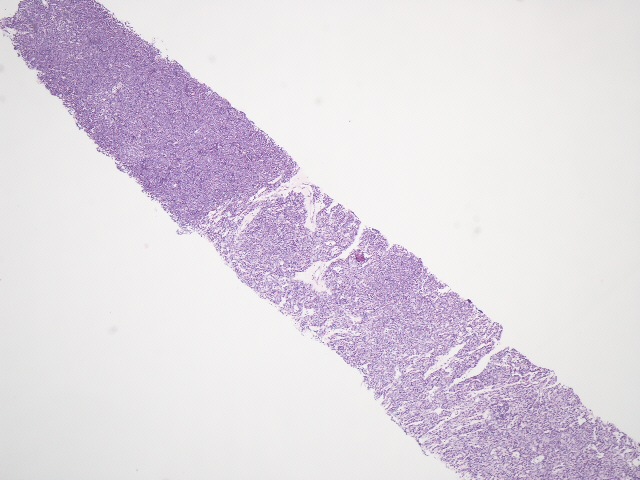
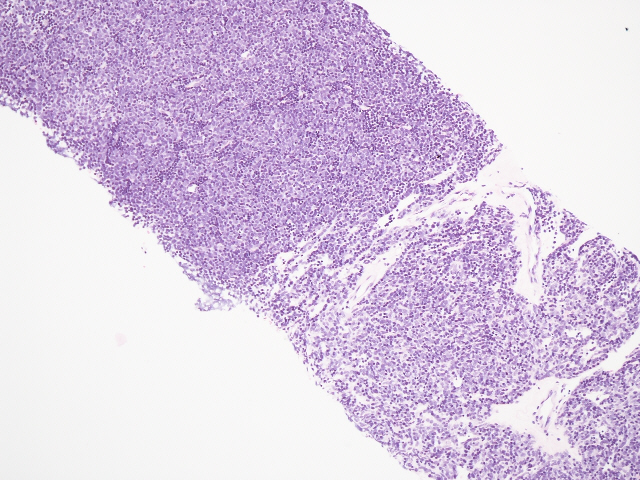
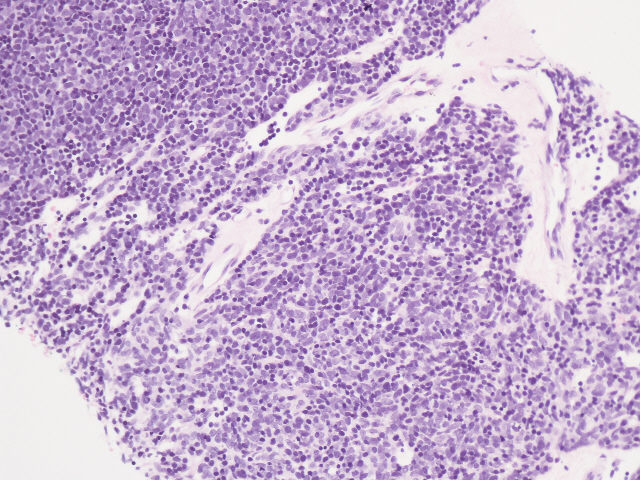
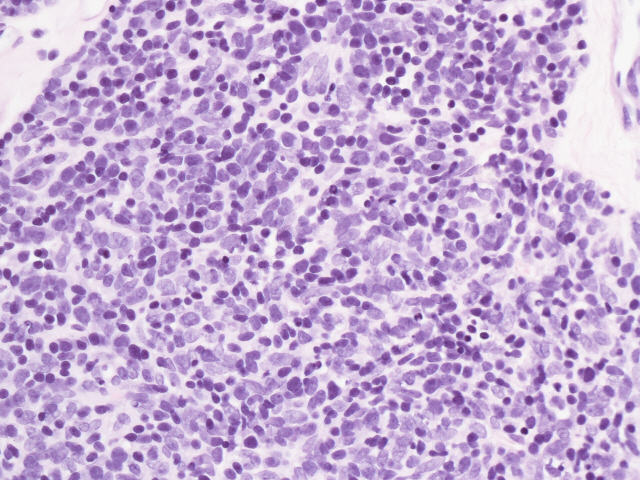
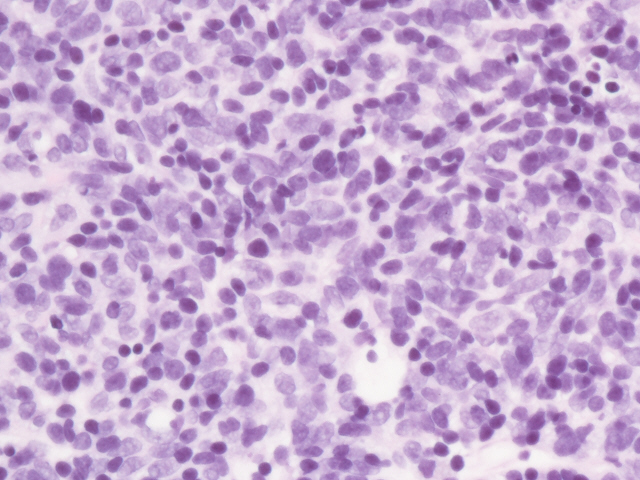
Microscopic images:
What is your diagnosis?
Diagnosis: Thymoma, B1 type
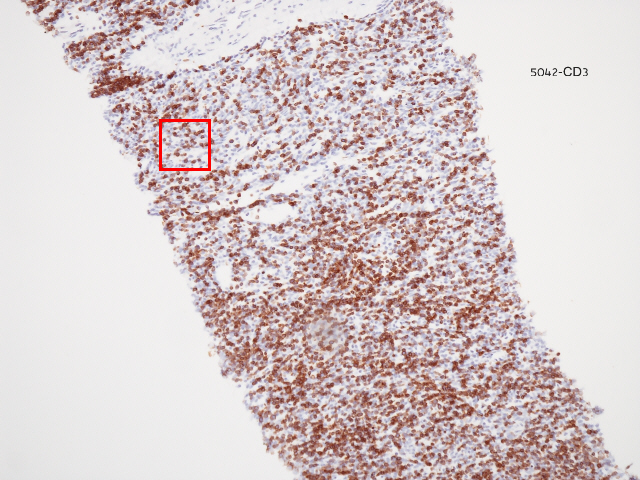
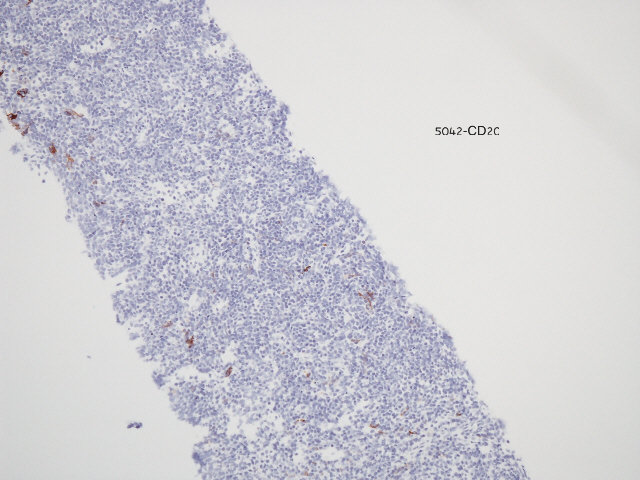
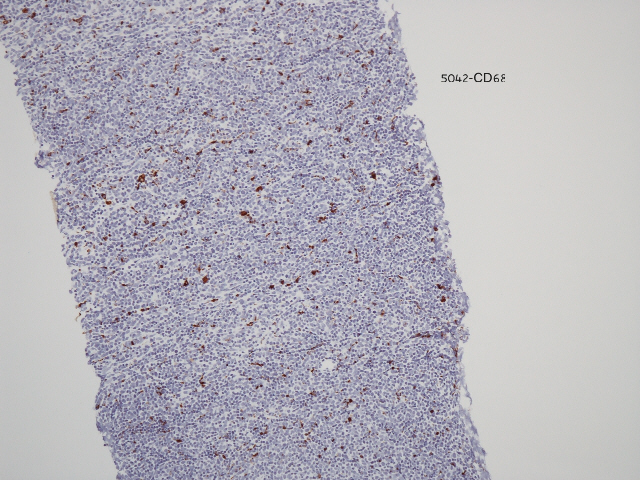
Immunostains:
Discussion:
Thymoma is the most common primary anterior mediastinal neoplasm. It is often associated with myasthenia gravis and other immune mediated disorders.
Morphologically, thymoma is a combination of bland epithelial cells and nonneoplastic lymphocytes. This case was classified as type B1 (WHO) based on the large number of T lymphocytes (CD3+) mixed with epithelial cells (keratin+).
The numerous classification systems of thymoma have been extensively discussed, most recently by Suster and Moran (Am J Clin Pathol 2006;125:542). For prognostic purposes, it is important to distinguish thymoma types that typically have benign behavior (types A, AB, B, B1 and B2), from those with atypical behavior (type B3) and those that are cytologically malignant (type C, also called thymic carcinoma) (Ann Thorac Cardiovasc Surg 2005;11:367, Am J Surg Pathol 2002;26:1605).
The differential diagnosis of this lymphocyte rich type of thymoma is primarily lymphoblastic lymphoma and thymic lymphoid hyperplasia. Lymphoblastic lymphoma typically presents in teenagers or young adults. In contrast to thymoma, the lymphocytes are malignant and the epithelial component, if present, represents trapped normal epithelial cells. Careful use of immunostains is necessary to avoid misdiagnosis. Thymic lymphoid hyperplasia is also associated with myasthenia gravis but typically does not produce a mass. Lymphoid follicles are present with normal germinal centers but the pattern of epithelial cells may be disrupted. In some cases, the differential diagnosis of thymoma may also include thymic carcinoid tumor (if rosettes are present) or Castleman disease.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Keloth E. Pradeep, Wrexham Maelor Hospital, United Kingdom.

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your client’s EMR systems securely and accurately.
For more information, contact www.lifepoint.com or call 866-LABTEST.
Website news:
(1) As an aside, we are pleased that American Journal of Clinical Pathology is now providing articles that are free full text, no registration, after 1 year from publication. Other free full text, no registration pathology journals that we find particularly useful are Archives of Pathology and Laboratory Medicine (always free) and Modern Pathology (free after 1 year from publication).
Visit and follow our Blog to see recent updates to the website.
(1) As an aside, we are pleased that American Journal of Clinical Pathology is now providing articles that are free full text, no registration, after 1 year from publication. Other free full text, no registration pathology journals that we find particularly useful are Archives of Pathology and Laboratory Medicine (always free) and Modern Pathology (free after 1 year from publication).
Visit and follow our Blog to see recent updates to the website.
Case #99
Clinical history:
A 70 year old man had a calcified mediastinal mass on chest Xray. A core needle biopsy was taken.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Thymoma, B1 type
Immunostains:
Discussion:
Thymoma is the most common primary anterior mediastinal neoplasm. It is often associated with myasthenia gravis and other immune mediated disorders.
Morphologically, thymoma is a combination of bland epithelial cells and nonneoplastic lymphocytes. This case was classified as type B1 (WHO) based on the large number of T lymphocytes (CD3+) mixed with epithelial cells (keratin+).
The numerous classification systems of thymoma have been extensively discussed, most recently by Suster and Moran (Am J Clin Pathol 2006;125:542). For prognostic purposes, it is important to distinguish thymoma types that typically have benign behavior (types A, AB, B, B1 and B2), from those with atypical behavior (type B3) and those that are cytologically malignant (type C, also called thymic carcinoma) (Ann Thorac Cardiovasc Surg 2005;11:367, Am J Surg Pathol 2002;26:1605).
The differential diagnosis of this lymphocyte rich type of thymoma is primarily lymphoblastic lymphoma and thymic lymphoid hyperplasia. Lymphoblastic lymphoma typically presents in teenagers or young adults. In contrast to thymoma, the lymphocytes are malignant and the epithelial component, if present, represents trapped normal epithelial cells. Careful use of immunostains is necessary to avoid misdiagnosis. Thymic lymphoid hyperplasia is also associated with myasthenia gravis but typically does not produce a mass. Lymphoid follicles are present with normal germinal centers but the pattern of epithelial cells may be disrupted. In some cases, the differential diagnosis of thymoma may also include thymic carcinoid tumor (if rosettes are present) or Castleman disease.