11 October 2007 - Case #97
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Hanni Gulwani, Sir Ganga Ram Hospital, New Delhi (India).

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your clients EMR systems securely and accurately. For more information, contact www.lifepoint.com or call 866-LABTEST.
Advertisement
Case #97
Clinical history:
A 29 year old man from India presented with progressively increasing nasal obstruction for 6 months. A mass was excised.
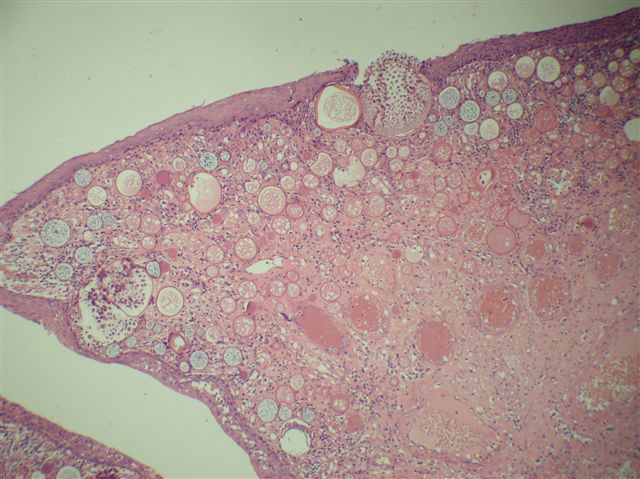
Microscopic images:
What is your diagnosis?
Diagnosis: Rhinosporidiosis
Discussion:
Rhinosporidiosis is caused by Rhinosporidium seeberi, traditionally thought to be a fungus but actually an aquatic protistan parasite (J Clin Microbiol 1999;37:2750, Emerg Infect Dis 2000;6:273, Indian J Med Microbiol 2002;20:119). It is endemic in southern India and Sri Lanka and occurs in emigrants from this region but a few indigenous cases in the U.S. have also been reported (Diagn Pathol 2006;1:25, Singapore Med J 2004;45:224, South Med J 1996;89:65). Rhinosporidium seeberi has a natural aquatic habitat and is transmitted through traumatized epithelium, most commonly in the nose and eye but also in the skin, ear, genitals and rectum. Bathing or working in stagnant water is a risk factor. It rarely presents with disseminated skin disease (Indian J Dermatol Venereol Leprol 2007;73:185, Indian J Dermatol Venereol Leprol 2001;67:332). It is not transmitted person to person.
In the nose, it presents as hyperplastic, polypoid, red, granular masses. Yellow pinhead spots represent mature sporangia. Superficial mucus is common. Microscopically, there are large (100 - 450 microns), thick walled sporangia containing over 1000 endospores that are each 6 - 10 microns, accompanied by a mixed inflammatory infiltrate. These structures may not be present in all portions of the tissue and additional sampling may be needed for diagnosis. The organisms are stained by GMS and PAS.
The differential diagnosis includes myospherulosis and other fungi. Myospherulosis is an iatrogenic lipogranuloma caused by hemostatic packing of the nasal cavity or paranasal sinuses with a petrolatum based ointment and gauze. Histologically, large tissue spaces are identified with saclike structures containing brown spherules that resemble prototheca but are actually clumped red blood cells which do not stain with GMS. Coccidiodes immitis also has spherules and endospores but they are smaller (spherules: 30 - 60 microns, endospores: 2 - 5 microns); arthroconidia and hyphae may also be found.
Treatment is surgical excision but recurrences are common. There is currently no effective medical treatment.
References: eMedicine: Rhinosporidiosis [Accessed 16 May 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Hanni Gulwani, Sir Ganga Ram Hospital, New Delhi (India).

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your clients EMR systems securely and accurately. For more information, contact www.lifepoint.com or call 866-LABTEST.
Case #97
Clinical history:
A 29 year old man from India presented with progressively increasing nasal obstruction for 6 months. A mass was excised.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Rhinosporidiosis
Discussion:
Rhinosporidiosis is caused by Rhinosporidium seeberi, traditionally thought to be a fungus but actually an aquatic protistan parasite (J Clin Microbiol 1999;37:2750, Emerg Infect Dis 2000;6:273, Indian J Med Microbiol 2002;20:119). It is endemic in southern India and Sri Lanka and occurs in emigrants from this region but a few indigenous cases in the U.S. have also been reported (Diagn Pathol 2006;1:25, Singapore Med J 2004;45:224, South Med J 1996;89:65). Rhinosporidium seeberi has a natural aquatic habitat and is transmitted through traumatized epithelium, most commonly in the nose and eye but also in the skin, ear, genitals and rectum. Bathing or working in stagnant water is a risk factor. It rarely presents with disseminated skin disease (Indian J Dermatol Venereol Leprol 2007;73:185, Indian J Dermatol Venereol Leprol 2001;67:332). It is not transmitted person to person.
In the nose, it presents as hyperplastic, polypoid, red, granular masses. Yellow pinhead spots represent mature sporangia. Superficial mucus is common. Microscopically, there are large (100 - 450 microns), thick walled sporangia containing over 1000 endospores that are each 6 - 10 microns, accompanied by a mixed inflammatory infiltrate. These structures may not be present in all portions of the tissue and additional sampling may be needed for diagnosis. The organisms are stained by GMS and PAS.
The differential diagnosis includes myospherulosis and other fungi. Myospherulosis is an iatrogenic lipogranuloma caused by hemostatic packing of the nasal cavity or paranasal sinuses with a petrolatum based ointment and gauze. Histologically, large tissue spaces are identified with saclike structures containing brown spherules that resemble prototheca but are actually clumped red blood cells which do not stain with GMS. Coccidiodes immitis also has spherules and endospores but they are smaller (spherules: 30 - 60 microns, endospores: 2 - 5 microns); arthroconidia and hyphae may also be found.
Treatment is surgical excision but recurrences are common. There is currently no effective medical treatment.
References: eMedicine: Rhinosporidiosis [Accessed 16 May 2024]