20 September 2007 - Case #96
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Jamie Shutter, University of South Florida, Tampa, Florida (USA), for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Case #96
Clinical history:
The patient was a 55 year woman with a 24 cm pelvic mass, massive ascites and a diffusely nodular omentum. The mass was excised.
Gross image:
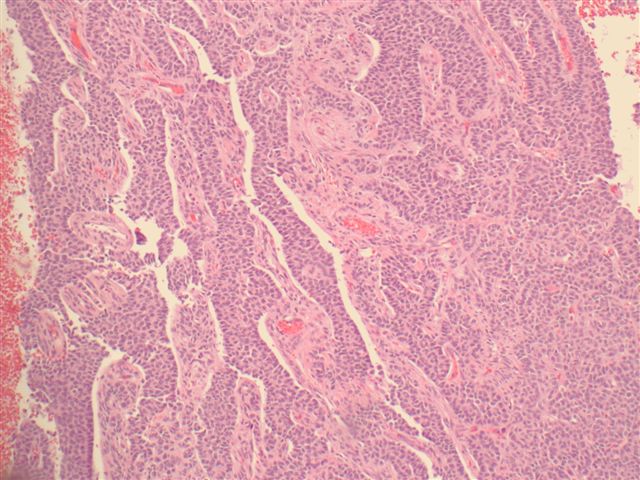
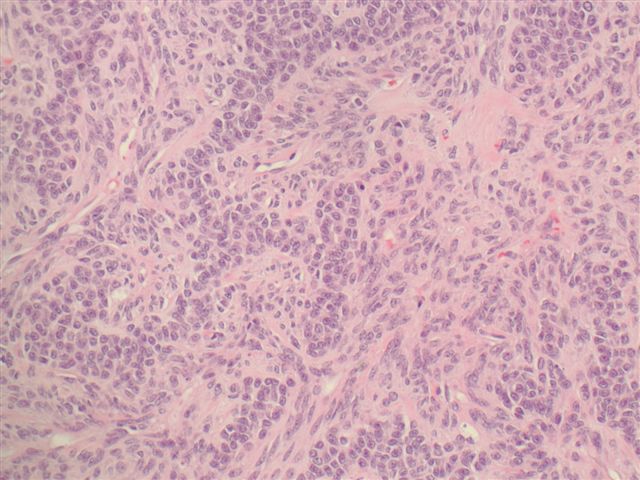
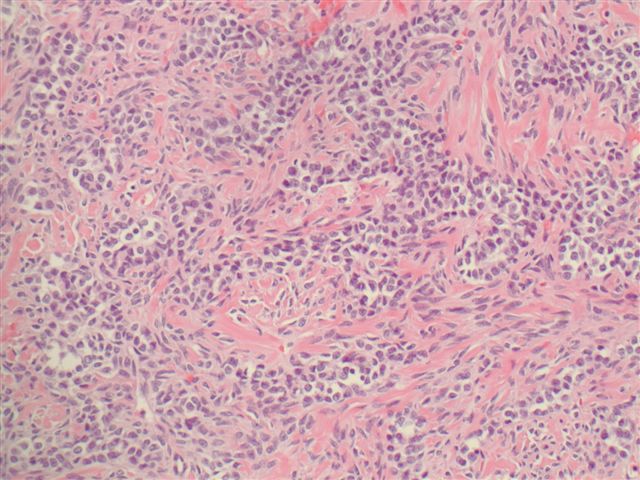
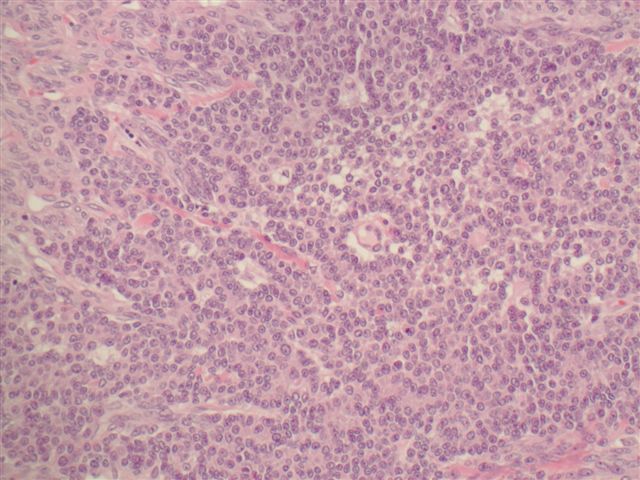
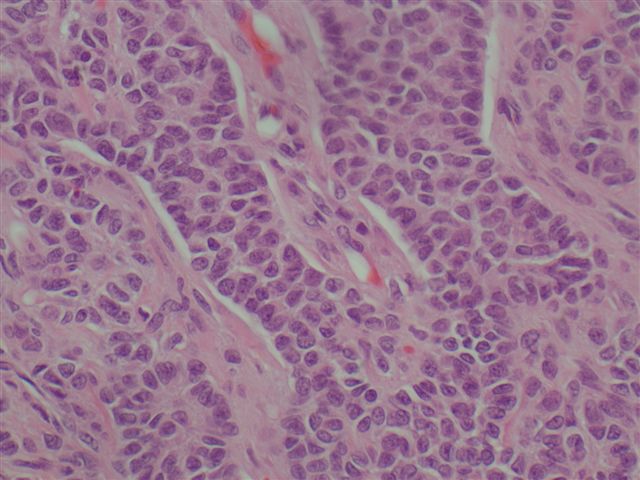
Microscopic images:
What is your diagnosis?
Diagnosis: Granulosa cell tumor, adult type
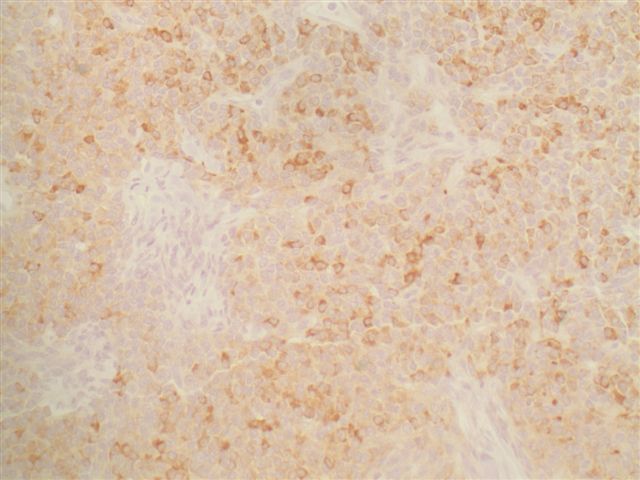
Immunostains:
Discussion:
This is a relatively straight forward case of a common tumor in women. Most (75%) cases are associated with hyperestrogenism. In children, these tumors may cause precocious puberty and in adults, they may be associated with metrorrhagia or endometrial hyperplasia / carcinoma.
The tumor grossly is an encapsulated cystic or solid tumor with straw colored or mucoid fluid. Microscopically there are small, bland, cuboidal to polygonal cells in various patterns, including Call-Exner bodies (small follicle-like structures containing eosinophilic material), macrofollicular, trabecular, solid or insular (island-like) patterns. Focal luteinization (plump cells with abundant cytoplasm) may be present, particularly during pregnancy. The tumor cells often have distinctive coffee bean shaped nuclei (also called folded nuclei or nuclear grooves).
These tumors have a good prognosis, with a 10 year survival over 90%. However, they may recur late, even after 20 years and 5 - 25% may have malignant behavior, which cannot be predicted from morphology. In the present case, the omental nodules were only reactive mesothelial hyperplasia and not metastases.
Adult granulosa cell tumors are usually immunoreactive for inhibin, calretinin, vimentin and smooth muscle actin (Am J Surg Pathol 2002;26:1477). However, reliance of immunostains for diagnosis is dangerous, as these tumors may also be immunoreactive for CD99, S100 (50%) and keratin (Mod Pathol 1998;11:769). This is a particular problem for tumors resembling poorly differentiated surface epithelial carcinoma, which is also keratin positive, although with diffuse staining, in contrast to the dot-like keratin staining of granulosa cell tumors (Virchows Arch A Pathol Anat Histopathol 1989;414:439, Am J Surg Pathol 1992;16:962). The differential diagnosis of granulosa cell tumors also includes endometrial stromal sarcoma, endometrioid carcinoma, small cell carcinoma of hypercalcemic type and pregnancy related granulosa cell proliferation (Hum Pathol 1988;19:657).
Distinctive nuclear grooves are not specific to granulosa cell tumors, as indicated in the table below. The table would be even larger if it included entities with nuclear folds, slight nuclear grooving, tumor cells with nuclear irregularities or grooves in cytologic specimens (Acta Cytol 2001;45:48).
Nuclear grooves and other nuclear envelope irregularities may be physiologic (normal cells) or due to altered expression of cytoplasmic intermediate filaments, actin or tubulin (tumor cells). For example, disruption of vimentin intermediate filaments causes nuclear folds or invaginations in cell lines (J Cell Sci 1994;107:1593). The RET / PTC oncogene, associated with papillary thyroid carcinoma, can rapidly induce nuclear envelope irregularities, perhaps by generating external forces on the nuclear envelope via intermediate filaments (Am J Pathol 2003;163:1091).
The function of nuclear grooves is not understood. In plants, they provide an increased nuclear surface area that may promote transport across the nuclear membrane (Plant Cell 2000;12:2425). Whether this occurs in humans is unknown.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Jamie Shutter, University of South Florida, Tampa, Florida (USA), for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Website news:
(1) We recently updated CD Markers CD240 to CD249 in the chapter CD Markers, CD100 to CD400. This includes CD240CE (Rh CE antigens), CD240D (Rh D antigen) and CD241 (Rh AG), important for transfusion medicine; CD243 (MDR-1), which has prognostic value in various malignancies; and CD246 (ALK1), which has diagnostic importance for anaplastic large cell lymphoma and inflammatory myofibroblastic tumor. We check each of our 30,000+ links monthly, and have fixed almost all of the bad links to WebPathology, WebPath and elsewhere. To reduce the number of bad links, we are obtaining more donated images and using more images from the AFIP Fascicles, third series.
Visit and follow our Blog to see recent updates to the website.
(1) We recently updated CD Markers CD240 to CD249 in the chapter CD Markers, CD100 to CD400. This includes CD240CE (Rh CE antigens), CD240D (Rh D antigen) and CD241 (Rh AG), important for transfusion medicine; CD243 (MDR-1), which has prognostic value in various malignancies; and CD246 (ALK1), which has diagnostic importance for anaplastic large cell lymphoma and inflammatory myofibroblastic tumor. We check each of our 30,000+ links monthly, and have fixed almost all of the bad links to WebPathology, WebPath and elsewhere. To reduce the number of bad links, we are obtaining more donated images and using more images from the AFIP Fascicles, third series.
Visit and follow our Blog to see recent updates to the website.
Case #96
Clinical history:
The patient was a 55 year woman with a 24 cm pelvic mass, massive ascites and a diffusely nodular omentum. The mass was excised.
Gross image:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Granulosa cell tumor, adult type
Immunostains:
Discussion:
This is a relatively straight forward case of a common tumor in women. Most (75%) cases are associated with hyperestrogenism. In children, these tumors may cause precocious puberty and in adults, they may be associated with metrorrhagia or endometrial hyperplasia / carcinoma.
The tumor grossly is an encapsulated cystic or solid tumor with straw colored or mucoid fluid. Microscopically there are small, bland, cuboidal to polygonal cells in various patterns, including Call-Exner bodies (small follicle-like structures containing eosinophilic material), macrofollicular, trabecular, solid or insular (island-like) patterns. Focal luteinization (plump cells with abundant cytoplasm) may be present, particularly during pregnancy. The tumor cells often have distinctive coffee bean shaped nuclei (also called folded nuclei or nuclear grooves).
These tumors have a good prognosis, with a 10 year survival over 90%. However, they may recur late, even after 20 years and 5 - 25% may have malignant behavior, which cannot be predicted from morphology. In the present case, the omental nodules were only reactive mesothelial hyperplasia and not metastases.
Adult granulosa cell tumors are usually immunoreactive for inhibin, calretinin, vimentin and smooth muscle actin (Am J Surg Pathol 2002;26:1477). However, reliance of immunostains for diagnosis is dangerous, as these tumors may also be immunoreactive for CD99, S100 (50%) and keratin (Mod Pathol 1998;11:769). This is a particular problem for tumors resembling poorly differentiated surface epithelial carcinoma, which is also keratin positive, although with diffuse staining, in contrast to the dot-like keratin staining of granulosa cell tumors (Virchows Arch A Pathol Anat Histopathol 1989;414:439, Am J Surg Pathol 1992;16:962). The differential diagnosis of granulosa cell tumors also includes endometrial stromal sarcoma, endometrioid carcinoma, small cell carcinoma of hypercalcemic type and pregnancy related granulosa cell proliferation (Hum Pathol 1988;19:657).
Distinctive nuclear grooves are not specific to granulosa cell tumors, as indicated in the table below. The table would be even larger if it included entities with nuclear folds, slight nuclear grooving, tumor cells with nuclear irregularities or grooves in cytologic specimens (Acta Cytol 2001;45:48).
| Cells or diseases with distinctive nuclear grooves (partial list) |
| Normal or reactive Lymphoblasts and lymphocytes (centrocytes) Histiocytes (normal and inflammatory conditions) Osteoblasts Granulosa cells, Sertoli cells Melanocytes, sebaceous glands, Langerhans cells Prostate basal cells (some) Mesothelial hyperplasia Urothelial metaplasia |
| Hematopoietic malignancies Leukemia: AML-M3, M4, M5 Lymphoblastic leukemia / lymphoma Granulocytic sarcoma Hairy cell leukemia Histiocytic sarcoma Diffuse large B cell lymphoma (occasionally) Mantle cell lymphoma, blastoid variant |
| Bone and soft tissue tumors Liposarcoma, myxoid / round cell Giant cell tumor of tendon sheath Adamantinoma Chondroblastoma Desmoplastic small round cell tumor Epithelioid hemangioendothelioma Epithelioid angiosarcoma |
| Papillary tumors Papillary thyroid carcinoma Papillary tumor of pineal region Solid pseudopapillary neoplasm of the pancreas Other papillary tumors |
| Gynecologic Granulosa cell tumor Sex cord tumor with annular tubules Brenner tumor Fallopian tube Walthard cell nests Cervix, normal cells, ASCUS, dysplasia |
| Other Hyalinizing trabecular adenoma of thyroid gland Pleomorphic adenoma of salivary gland Langerhans cell histiocytosis Breast myofibroblastoma Clear cell sarcoma of kidney Epithelioid GI stromal tumor Ependymoma Melanocytoma of CNS |
Nuclear grooves and other nuclear envelope irregularities may be physiologic (normal cells) or due to altered expression of cytoplasmic intermediate filaments, actin or tubulin (tumor cells). For example, disruption of vimentin intermediate filaments causes nuclear folds or invaginations in cell lines (J Cell Sci 1994;107:1593). The RET / PTC oncogene, associated with papillary thyroid carcinoma, can rapidly induce nuclear envelope irregularities, perhaps by generating external forces on the nuclear envelope via intermediate filaments (Am J Pathol 2003;163:1091).
The function of nuclear grooves is not understood. In plants, they provide an increased nuclear surface area that may promote transport across the nuclear membrane (Plant Cell 2000;12:2425). Whether this occurs in humans is unknown.