11 October 2007 - Case #95
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Michael W. Robles, AmeriPath North Texas (USA).

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your client’s EMR systems securely and accurately. For more information, contact www.lifepoint.com or call 866-LABTEST.
Advertisement
Case #95
Clinical history:
The patient was a 55 year old man with a history of colon polyps, diverticulosis and hypertrophy of the anal papillae. At routine colonoscopy, no polyps were found but there was a 2 cm nodular patch in the cecum, which was biopsied.
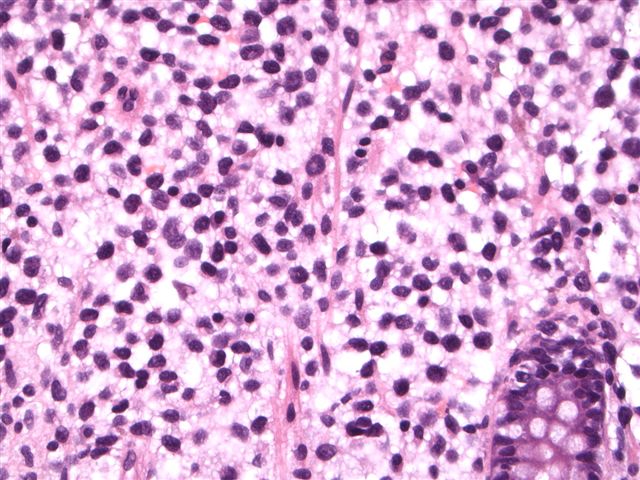
Microscopic images:
What is your diagnosis?
Diagnosis: Consistent with hairy cell leukemia
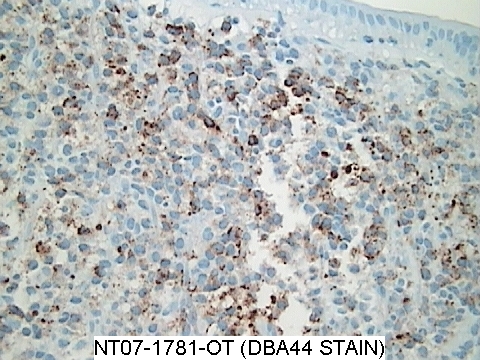
Immunostains
Discussion:
Multiple fragments of nodular colonic mucosa demonstrate mucosal and submucosal infiltrates of small and medium lymphocytes with abundant pale cytoplasm and oval, indented nuclei. The lymphocytes were immunoreactive for CD20, DBA-44, CD68, cyclin D1 / BCL1 (patchy) and Ki67 (mildly increased proliferation index). They were negative for CD5. After the biopsy was submitted, the pathologist learned that the patient had a history of hairy cell leukemia.
Hairy cell leukemia is a rare, chronic B cell lymphoproliferative disorder, usually affecting older white men (mean age 52 years), who present with massive splenomegaly with red pulp involvement and obliteration of the white pulp. There is often pancytopenia (50%) and infections (30%) but usually minimal lymphadenopathy. Bone marrow aspiration biopsies are often unsuccessful due to marrow fibrosis. The peripheral blood shows only rare leukemic cells. Occasional cases may involve the skin or other organs. GI involvement is rare.
The distinctive hairy cell is seen in bone marrow biopsies. It has clear to lightly eosinophilic or basophilic cytoplasm, with surface projections that may be delicate or broad. There may be cytoplasmic vacuoles or azurophilic granules. The nuclei are oval or indented. Formalin fixed tissue often has a perinuclear halo.
Besides the markers indicated above, the hairy cells are also positive for B cell markers CD19, CD22, CD79a and PAX5, as well as TRAP, CD25 and CD103. Recommended combinations of markers to order include DBA-44 and TRAP and flow cytometry with CD11c, CD20, CD25 and CD103 (Arch Pathol Lab Med 2007;131:383). Of note, atypical immunophenotyping has been reported in 34% of cases and a variant type has also been described (Am J Clin Pathol 2006;125:251, Am J Clin Pathol 2005;123:132).
The differential diagnosis includes splenic marginal zone lymphoma and mastocytosis. Splenic marginal zone lymphoma, like hairy cell leukemia, typically involves the spleen and may have circulating cells with abundant cytoplasm and cytoplasmic processes. In contrast to hairy cell leukemia, the cytoplasmic processes are usually polar, not circumferential and there is a nodular pattern of splenic white pulp involvement, not obliteration of the white pulp. The cells usually do not express DBA-44, TRAP or CD103. Mastocytosis often involves the spleen, and mast cells also have abundant clear cytoplasm. However, they are negative for B cell markers and positive for toluidine blue, Giemsa, tryptase and CD117.
Treatment of hairy cell leukemia with purine analogs and interferon frequently causes complete responses and a markedly improved disease free survival (Hematol Oncol Clin North Am 2006;20:1153). Due to frequent aberrant staining, it is important to order an adequate number of immunostains and to correlate histologic, immunohistochemical and clinical findings to ensure the correct diagnosis.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Michael W. Robles, AmeriPath North Texas (USA).

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your client’s EMR systems securely and accurately. For more information, contact www.lifepoint.com or call 866-LABTEST.
Case #95
Clinical history:
The patient was a 55 year old man with a history of colon polyps, diverticulosis and hypertrophy of the anal papillae. At routine colonoscopy, no polyps were found but there was a 2 cm nodular patch in the cecum, which was biopsied.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Consistent with hairy cell leukemia
Immunostains
Discussion:
Multiple fragments of nodular colonic mucosa demonstrate mucosal and submucosal infiltrates of small and medium lymphocytes with abundant pale cytoplasm and oval, indented nuclei. The lymphocytes were immunoreactive for CD20, DBA-44, CD68, cyclin D1 / BCL1 (patchy) and Ki67 (mildly increased proliferation index). They were negative for CD5. After the biopsy was submitted, the pathologist learned that the patient had a history of hairy cell leukemia.
Hairy cell leukemia is a rare, chronic B cell lymphoproliferative disorder, usually affecting older white men (mean age 52 years), who present with massive splenomegaly with red pulp involvement and obliteration of the white pulp. There is often pancytopenia (50%) and infections (30%) but usually minimal lymphadenopathy. Bone marrow aspiration biopsies are often unsuccessful due to marrow fibrosis. The peripheral blood shows only rare leukemic cells. Occasional cases may involve the skin or other organs. GI involvement is rare.
The distinctive hairy cell is seen in bone marrow biopsies. It has clear to lightly eosinophilic or basophilic cytoplasm, with surface projections that may be delicate or broad. There may be cytoplasmic vacuoles or azurophilic granules. The nuclei are oval or indented. Formalin fixed tissue often has a perinuclear halo.
Besides the markers indicated above, the hairy cells are also positive for B cell markers CD19, CD22, CD79a and PAX5, as well as TRAP, CD25 and CD103. Recommended combinations of markers to order include DBA-44 and TRAP and flow cytometry with CD11c, CD20, CD25 and CD103 (Arch Pathol Lab Med 2007;131:383). Of note, atypical immunophenotyping has been reported in 34% of cases and a variant type has also been described (Am J Clin Pathol 2006;125:251, Am J Clin Pathol 2005;123:132).
The differential diagnosis includes splenic marginal zone lymphoma and mastocytosis. Splenic marginal zone lymphoma, like hairy cell leukemia, typically involves the spleen and may have circulating cells with abundant cytoplasm and cytoplasmic processes. In contrast to hairy cell leukemia, the cytoplasmic processes are usually polar, not circumferential and there is a nodular pattern of splenic white pulp involvement, not obliteration of the white pulp. The cells usually do not express DBA-44, TRAP or CD103. Mastocytosis often involves the spleen, and mast cells also have abundant clear cytoplasm. However, they are negative for B cell markers and positive for toluidine blue, Giemsa, tryptase and CD117.
Treatment of hairy cell leukemia with purine analogs and interferon frequently causes complete responses and a markedly improved disease free survival (Hematol Oncol Clin North Am 2006;20:1153). Due to frequent aberrant staining, it is important to order an adequate number of immunostains and to correlate histologic, immunohistochemical and clinical findings to ensure the correct diagnosis.