9 March 2007 - Case #76
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. J. Ross Slemmer, SkyRidge Medical Center, Cleveland, Tennessee (USA).
Case #76
Clinical history:
A 49 year old man had a left inguinal mass. A CT scan revealed bulky retroperitoneal lymphadenopathy and his serum PSA was 6.5. Serum CA125 was not obtained. He had a 2 year history of sporadic hematuria, but cystoscopy showed only a slight irregularity or granularity of the prostatic urethra and his serum PSA was normal.
At pelvic ultrasound, the urologist reported that he could not identify the prostate, which was apparently obliterated by a neoplastic process. He obtained blind core biopsies for frozen section to determine if he was in or near the prostate. An enlarged femoral lymph node was also excised and sent for frozen section.
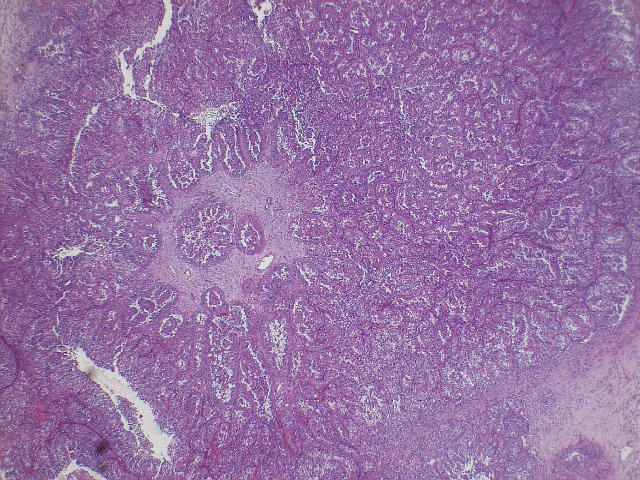
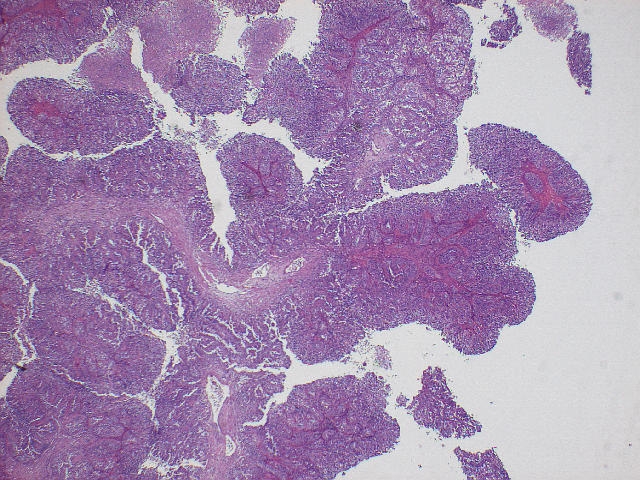
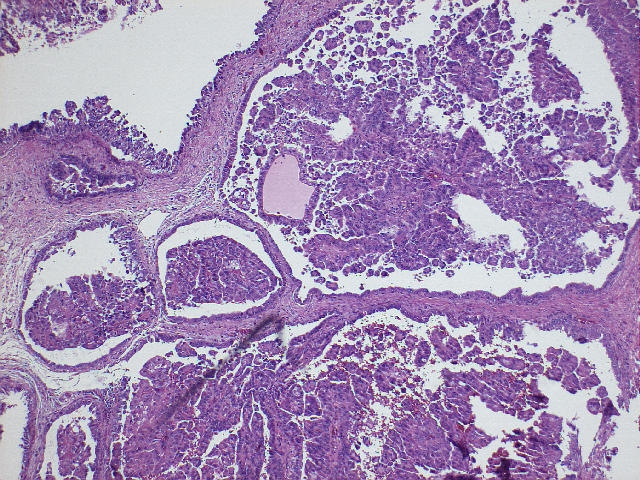
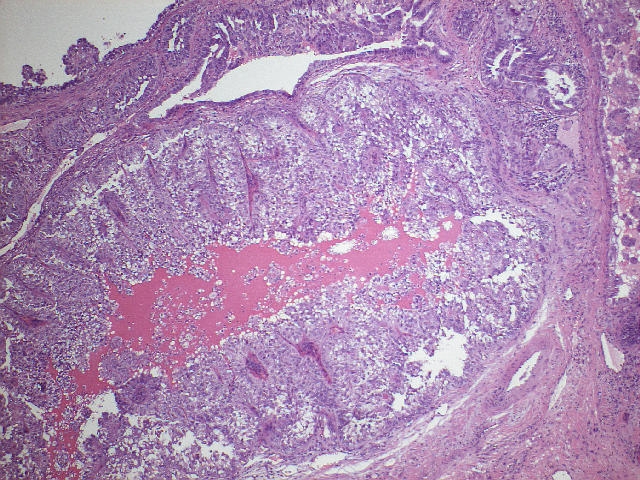
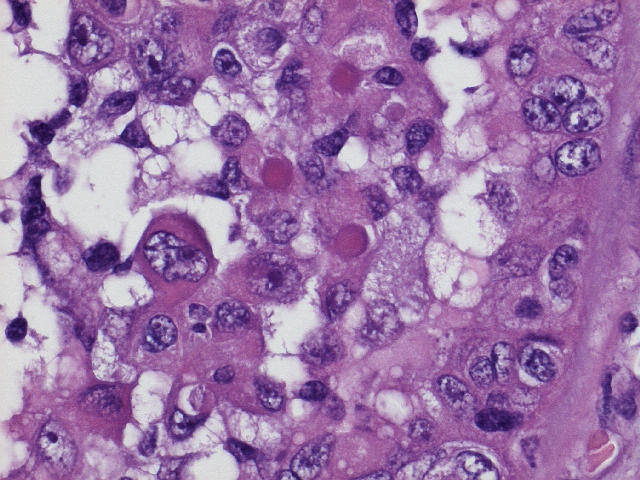
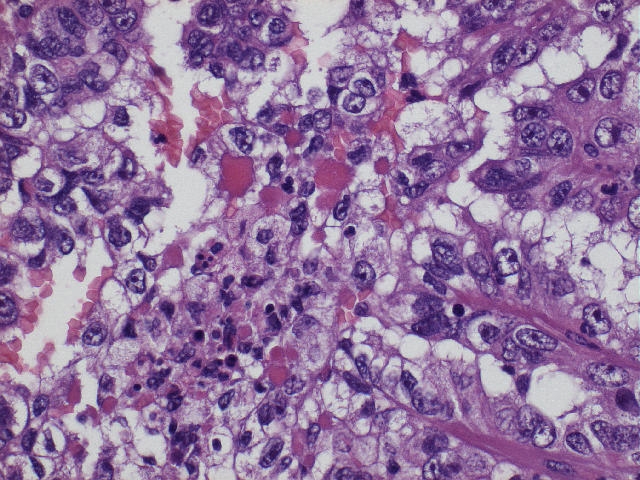
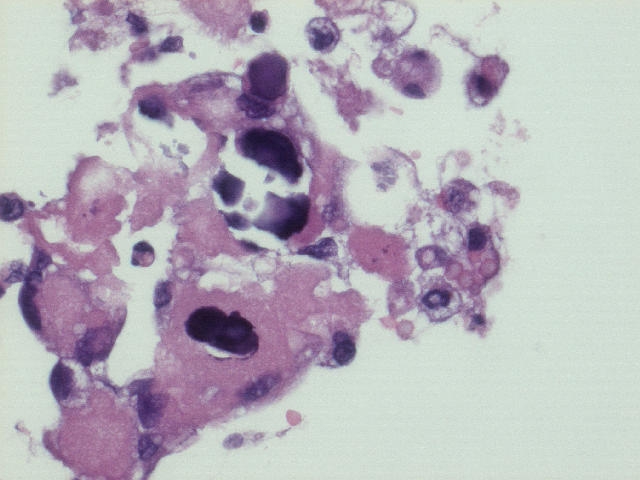
Microscopic images:
What is your diagnosis?
Diagnosis: Clear cell adenocarcinoma of prostate with tubulocystic growth and metastasis to femoral lymph node
Discussion:
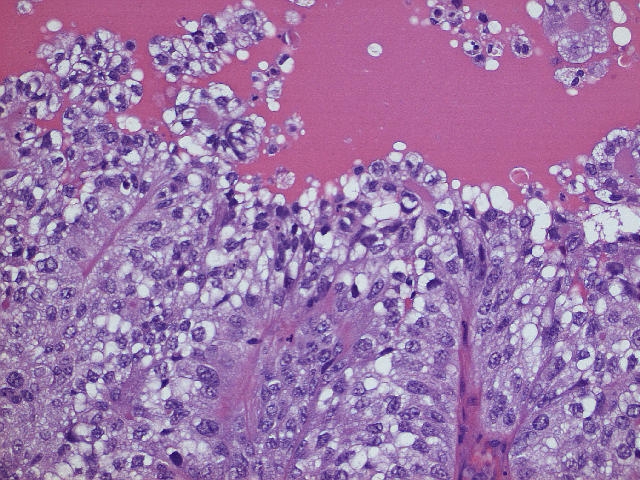
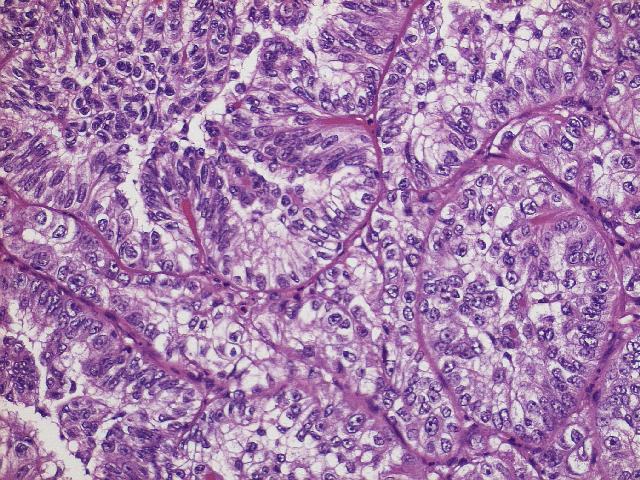
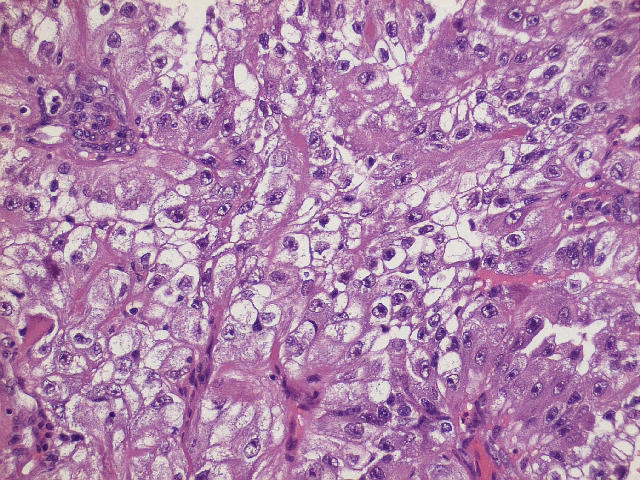
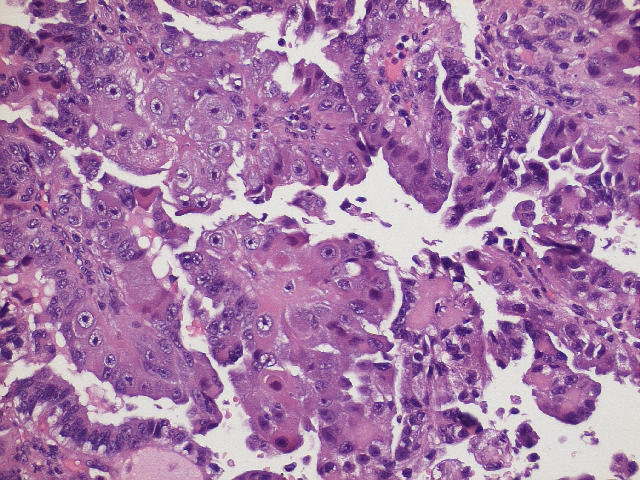
This is a very rare tumor of the prostate, whose diagnosis was confirmed by Dr. Jonathan Epstein. A similar case was reported from Taiwan, published by Dr. Epstein et. al. (Am J Surg Pathol 2000;24:1433). In both cases, the tumor was composed of papillary and tubulocystic glands lined by cuboidal and hobnail cells with clear to eosinophilic cytoplasm. The nuclei were mildly pleomorphic and had prominent nucleoli. Psammoma bodies were occasionally seen . There was no / minimal mitotic activity. Hyaline globules were present in this case but not reported in the published case.
The tumor cells in the published case were immunoreactive for pancytokeratin, low molecular weight cytokeratin and EMA and focally positive for high molecular weight keratin (34betaE12). They were negative for PSA and PAP. The patient in the published case had an elevated serum CA125 but normal serum PSA and CEA.
Clear cell adenocarcinomas, although common in women, are very rare in the urinary tract of men and occur predominantly in the urethra or urinary bladder. Other reported cases in the prostate include a clear cell carcinoma of the prostatic utricle in a 16 year old boy reported from Uruguay and a renal cell type of prostatic carcinoma which lacked hobnail cells and had staining patterns similar to renal cell carcinoma (Ann Diagn Pathol 2005;9:153, Am J Surg Pathol 2003;27:407).
The differential diagnosis is limited. Some prostatic ductal carcinomas or Gleason pattern 4 adenocarcinomas have focal papillary formation. However, there are no tubulocystic or papillary structures lined by clear or hobnail cells. These tumors also have the usual staining pattern of PSA+, PAP+ for prostatic adenocarcinoma. Other clear cell tumors include nephrogenic adenoma, clear cell urothelial carcinoma and metastatic renal cell carcinoma (Hum Pathol 1994;25:390).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. J. Ross Slemmer, SkyRidge Medical Center, Cleveland, Tennessee (USA).
Case #76
Clinical history:
A 49 year old man had a left inguinal mass. A CT scan revealed bulky retroperitoneal lymphadenopathy and his serum PSA was 6.5. Serum CA125 was not obtained. He had a 2 year history of sporadic hematuria, but cystoscopy showed only a slight irregularity or granularity of the prostatic urethra and his serum PSA was normal.
At pelvic ultrasound, the urologist reported that he could not identify the prostate, which was apparently obliterated by a neoplastic process. He obtained blind core biopsies for frozen section to determine if he was in or near the prostate. An enlarged femoral lymph node was also excised and sent for frozen section.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Clear cell adenocarcinoma of prostate with tubulocystic growth and metastasis to femoral lymph node
Discussion:
This is a very rare tumor of the prostate, whose diagnosis was confirmed by Dr. Jonathan Epstein. A similar case was reported from Taiwan, published by Dr. Epstein et. al. (Am J Surg Pathol 2000;24:1433). In both cases, the tumor was composed of papillary and tubulocystic glands lined by cuboidal and hobnail cells with clear to eosinophilic cytoplasm. The nuclei were mildly pleomorphic and had prominent nucleoli. Psammoma bodies were occasionally seen . There was no / minimal mitotic activity. Hyaline globules were present in this case but not reported in the published case.
The tumor cells in the published case were immunoreactive for pancytokeratin, low molecular weight cytokeratin and EMA and focally positive for high molecular weight keratin (34betaE12). They were negative for PSA and PAP. The patient in the published case had an elevated serum CA125 but normal serum PSA and CEA.
Clear cell adenocarcinomas, although common in women, are very rare in the urinary tract of men and occur predominantly in the urethra or urinary bladder. Other reported cases in the prostate include a clear cell carcinoma of the prostatic utricle in a 16 year old boy reported from Uruguay and a renal cell type of prostatic carcinoma which lacked hobnail cells and had staining patterns similar to renal cell carcinoma (Ann Diagn Pathol 2005;9:153, Am J Surg Pathol 2003;27:407).
The differential diagnosis is limited. Some prostatic ductal carcinomas or Gleason pattern 4 adenocarcinomas have focal papillary formation. However, there are no tubulocystic or papillary structures lined by clear or hobnail cells. These tumors also have the usual staining pattern of PSA+, PAP+ for prostatic adenocarcinoma. Other clear cell tumors include nephrogenic adenoma, clear cell urothelial carcinoma and metastatic renal cell carcinoma (Hum Pathol 1994;25:390).