31 January 2007 - Case #72
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Adrian A. Suarez, National Children’s Hospital, San Jose, Costa Rica.

This Case is sponsored by Milestone Medical, the technological leader in Microwave Accelerated Tissue Processing. Milestone manufactures instrumentation and accessories that enable Histologists and Pathologists to achieve the highest level of productivity, while maintaining their flexibility and safety. Milestone’s family of rapid microwave lab stations allow tissue samples to be processed in a fraction of the time as compared to conventional methods, allowing for same-day diagnosis. They also offer a line of digital imaging equipment for grossing stations and autopsy rooms. These systems serve as a comprehensive method of storing macroscopic images of all specimens examined in the laboratory, providing an invaluable diagnostic database for routine grossing, teaching, and research.
For more information, please visit our website by clicking here.
Advertisement
Case #72
Clinical history:
A 2 year old boy had a tender, palpable mass in his right parietal region. Physical exam showed no skin lesions or enlarged organs and there were no neurological abnormalities. Xray films and CT scans of his skull showed lytic masses involving both parietal bones and extending into adjacent soft tissues. The base of the skull was spared. Blood chemistries were within reference values.
As is usual at our Institution, a fine needle aspiration biopsy was performed.
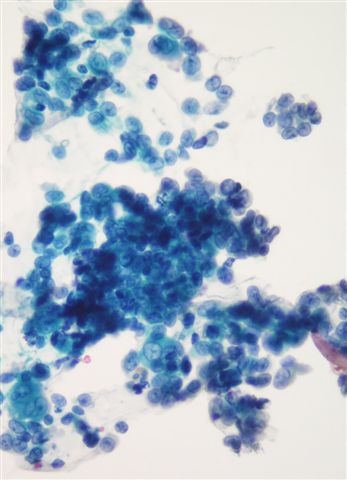
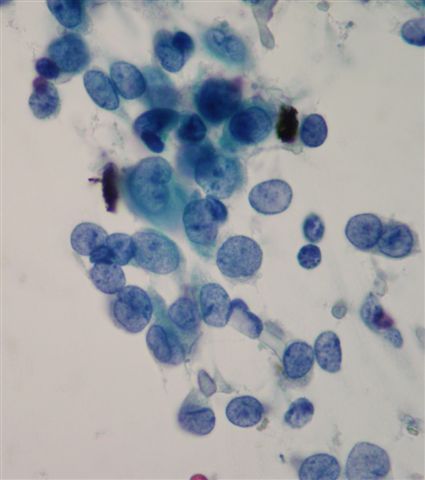
Smears were fixed in 95% ethanol and stained with Papanicolau. They were highly cellular and showed a predominantly non-cohesive population of medium sized cells with mild pleomorphism. Some cells were multinucleated. Nuclei were round, oval or bean shaped with prominent longitudinal grooves. Chromatin was fine and even. A rare mitotic figure was seen. The background was clean and included only a rare eosinophil and no lymphoglandular bodies.
Radiology images:
Clinical images:
Microscopic images:
What is your diagnosis?
Diagnosis: Langerhans cell histiocytosis
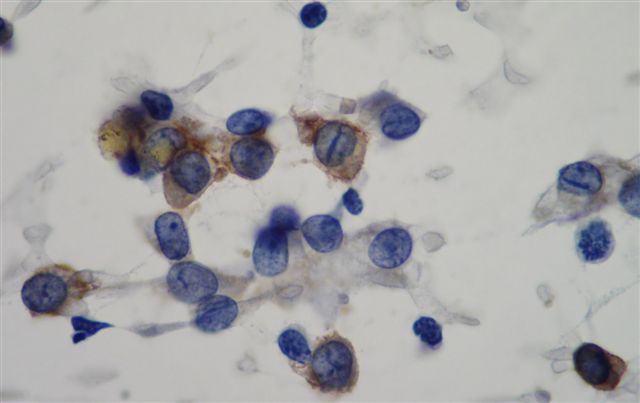
Immunostains:
Discussion:
The diagnosis was confirmed by a strongly positive CD1a stain.
Langerhans cell histiocytosis, formerly called histiocytosis X, is a neoplasm of Langerhans cells, which are antigen presenting cells. It typically involves children or adolescents and presents with solitary bone involvement (formerly called eosinophilic granuloma), multiple bone involvement or multiple organ involvement.
Grossly, it is a sharply circumscribed mass, often involving the skull, jaw, humerus, ribs or femur. Microscopically, there is infiltration by Langerhans cells, which may be accompanied by other inflammatory cells, fibrosis and necrosis. Langerhans cells, by both H&E and cytology smears, are large polygonal cells with abundant eosinophilic cytoplasm. They have distinctive oval nuclei with longitudinal grooves resembling coffee beans and no prominent nucleoli.
Langerhans cells are immunoreactive for S100, CD1a, vimentin and langerin, with variable CD68 staining. They are negative for HAM56, CD21 and CD35. Electron microscopy shows prominent electron dense cross striations, also called Birbeck granules.
CD1a is a T cell surface antigen important in dendritic cell presentation of glycolipids and lipopeptide antigens and its presence is fairly specific for Langerhans cell histiocytosis. However, it is also positive in T cell disorders, including cutaneous T cell lymphoma and T-ALL, as well as some other conditions.
The differential diagnosis includes other histiocytic disorders, including sinus histiocytosis with massive lymphadenopathy, monocytic leukemia and mastocytosis.
Excision is usually curative for solitary lesions but they may recur (reactivate) in up to 37% of cases with single system multifocal disease, usually within 2 years (Pediatr Blood Cancer 2007;48:696).
Reference: eMedicine: Langerhans Cell Histiocytosis [Accessed 3 June 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Adrian A. Suarez, National Children’s Hospital, San Jose, Costa Rica.

This Case is sponsored by Milestone Medical, the technological leader in Microwave Accelerated Tissue Processing. Milestone manufactures instrumentation and accessories that enable Histologists and Pathologists to achieve the highest level of productivity, while maintaining their flexibility and safety. Milestone’s family of rapid microwave lab stations allow tissue samples to be processed in a fraction of the time as compared to conventional methods, allowing for same-day diagnosis. They also offer a line of digital imaging equipment for grossing stations and autopsy rooms. These systems serve as a comprehensive method of storing macroscopic images of all specimens examined in the laboratory, providing an invaluable diagnostic database for routine grossing, teaching, and research.
For more information, please visit our website by clicking here.
Case #72
Clinical history:
A 2 year old boy had a tender, palpable mass in his right parietal region. Physical exam showed no skin lesions or enlarged organs and there were no neurological abnormalities. Xray films and CT scans of his skull showed lytic masses involving both parietal bones and extending into adjacent soft tissues. The base of the skull was spared. Blood chemistries were within reference values.
As is usual at our Institution, a fine needle aspiration biopsy was performed.
Smears were fixed in 95% ethanol and stained with Papanicolau. They were highly cellular and showed a predominantly non-cohesive population of medium sized cells with mild pleomorphism. Some cells were multinucleated. Nuclei were round, oval or bean shaped with prominent longitudinal grooves. Chromatin was fine and even. A rare mitotic figure was seen. The background was clean and included only a rare eosinophil and no lymphoglandular bodies.
Radiology images:
Clinical images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Langerhans cell histiocytosis
Immunostains:
Discussion:
The diagnosis was confirmed by a strongly positive CD1a stain.
Langerhans cell histiocytosis, formerly called histiocytosis X, is a neoplasm of Langerhans cells, which are antigen presenting cells. It typically involves children or adolescents and presents with solitary bone involvement (formerly called eosinophilic granuloma), multiple bone involvement or multiple organ involvement.
Grossly, it is a sharply circumscribed mass, often involving the skull, jaw, humerus, ribs or femur. Microscopically, there is infiltration by Langerhans cells, which may be accompanied by other inflammatory cells, fibrosis and necrosis. Langerhans cells, by both H&E and cytology smears, are large polygonal cells with abundant eosinophilic cytoplasm. They have distinctive oval nuclei with longitudinal grooves resembling coffee beans and no prominent nucleoli.
Langerhans cells are immunoreactive for S100, CD1a, vimentin and langerin, with variable CD68 staining. They are negative for HAM56, CD21 and CD35. Electron microscopy shows prominent electron dense cross striations, also called Birbeck granules.
CD1a is a T cell surface antigen important in dendritic cell presentation of glycolipids and lipopeptide antigens and its presence is fairly specific for Langerhans cell histiocytosis. However, it is also positive in T cell disorders, including cutaneous T cell lymphoma and T-ALL, as well as some other conditions.
The differential diagnosis includes other histiocytic disorders, including sinus histiocytosis with massive lymphadenopathy, monocytic leukemia and mastocytosis.
Excision is usually curative for solitary lesions but they may recur (reactivate) in up to 37% of cases with single system multifocal disease, usually within 2 years (Pediatr Blood Cancer 2007;48:696).
Reference: eMedicine: Langerhans Cell Histiocytosis [Accessed 3 June 2024]