19 December 2007 - Case #105
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Margarita De La Ossa, St. Jude Children’s Research Hospital, Tennessee (USA).

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your client’s EMR systems securely and accurately.
For more information, contact www.lifepoint.com or call 866-LABTEST.
Advertisement
Case #105
Clinical history:
A 6 year old boy who was postchemotherapy for metastatic neuroblastoma developed new bilateral pulmonary infiltrates. He was clinically stable with no respiratory distress. His complete blood count was: WBC 28.9, Hb 8.8, Hct 24.7, platelets 165. His peripheral blood differential count was: neutrophils 53%, bands 11%, lymphocytes 9%, monocytes 8%, eosinophils 2%, myelocytes 8%, metamyelocytes 7%, blasts 2%.
A core biopsy was obtained from the lung.
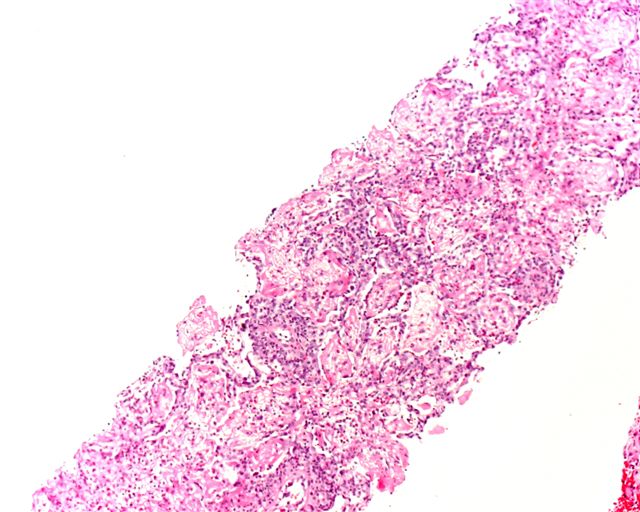
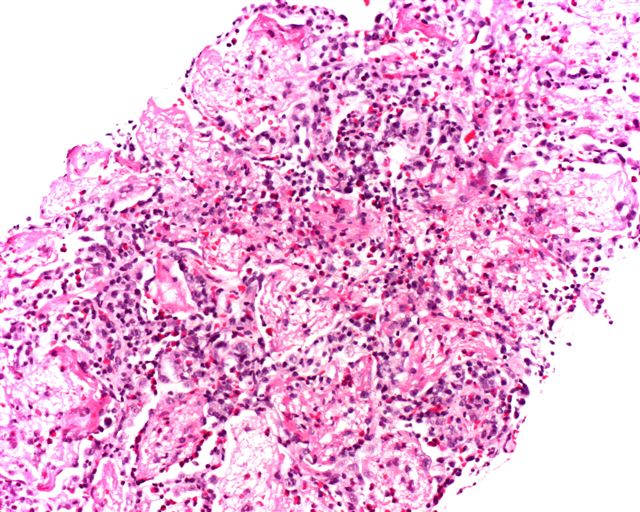
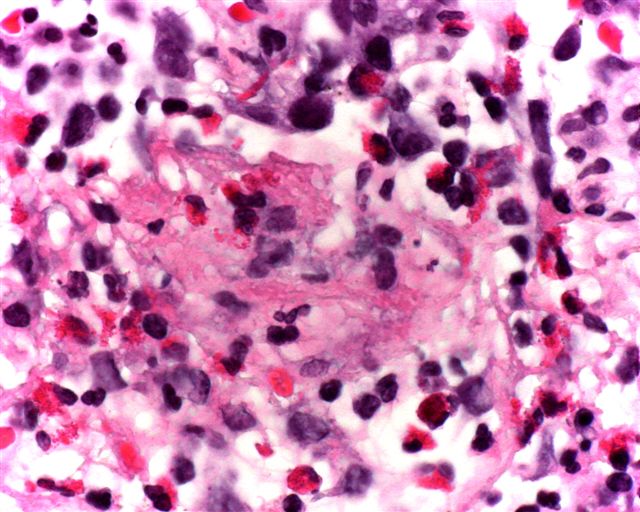
Microscopic images:
What is your diagnosis?
Diagnosis: Acute eosinophilic pneumonia
Discussion:
The lung biopsies show prominent eosinophilic infiltrates with focal diffuse alveolar damage exemplified by hyaline membranes and alveolar edema. No vasculitis is identified in these sections.
The eosinophilic pneumonias are disorders of both known and unknown etiology, characterized by eosinophils in alveolar and interstitial spaces, usually accompanied by blood eosinophilia (Travis: Non-Neoplastic Disorders of the Lower Respiratory Tract, 1st Edition, 2002).
These disorders may be caused by infections (parasites, HIV or fungi, particularly Aspergillus), drug reactions (antibiotics, cytotoxic or anti-inflammatory drugs), immune disorders (Churg-Strauss syndrome, collagen vascular disease, asthma or hypereosinophilic syndrome) or tobacco (flavored cigars, new onset of smoking (Chest 2007;131:1234, JAMA 2004;292:2997). Idiopathic eosinophilic pneumonia is classified as simple, acute or chronic.
Simple eosinophilic pneumonia, also called Loeffler syndrome, is a self limited disorder with no / minimal symptoms and often transient peripheral eosinophilia and radiographic opacities.
Acute eosinophilic pneumonia has its onset in 1 - 4 days and is accompanied by fever, cough, dyspnea and chest pain. Prominent eosinophils are present in bronchoalveolar lavage fluid and diffuse alveolar damage is identified at biopsy (Am J Respir Crit Care Med 2002;166:1235).
Chronic eosinophilic pneumonia resembles the acute form but with an insidious onset, usually in months and additional symptoms of weight loss and drenching night sweats. It is often associated with asthma, a high peripheral eosinophil count and distinct radiographic findings (Orphanet J Rare Dis 2006;1:11). Biopsy shows tissue eosinophilia and possibly fibrin but no diffuse alveolar damage. Both acute and chronic eosinophilic pneumonia respond dramatically to corticosteroids.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Margarita De La Ossa, St. Jude Children’s Research Hospital, Tennessee (USA).

This Case is sponsored by Lifepoint informatics, which provides a complete turnkey suite of IT connectivity products for Anatomic Pathology, Hospital, Reference and Independent Laboratories. Our Labtest.com on-line ordering and resulting system helps your lab connect, compete and comply. Our Lifepoint InfoHub connects your LIS/AP system to your client’s EMR systems securely and accurately.
For more information, contact www.lifepoint.com or call 866-LABTEST.
Website news:
(1) Are you making online purchases at Amazon.com? If so, please enter their websites through our Amazon page. Your purchases through this page help improve our free website.
Visit and follow our Blog to see recent updates to the website.
(1) Are you making online purchases at Amazon.com? If so, please enter their websites through our Amazon page. Your purchases through this page help improve our free website.
Visit and follow our Blog to see recent updates to the website.
Case #105
Clinical history:
A 6 year old boy who was postchemotherapy for metastatic neuroblastoma developed new bilateral pulmonary infiltrates. He was clinically stable with no respiratory distress. His complete blood count was: WBC 28.9, Hb 8.8, Hct 24.7, platelets 165. His peripheral blood differential count was: neutrophils 53%, bands 11%, lymphocytes 9%, monocytes 8%, eosinophils 2%, myelocytes 8%, metamyelocytes 7%, blasts 2%.
A core biopsy was obtained from the lung.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Acute eosinophilic pneumonia
Discussion:
The lung biopsies show prominent eosinophilic infiltrates with focal diffuse alveolar damage exemplified by hyaline membranes and alveolar edema. No vasculitis is identified in these sections.
The eosinophilic pneumonias are disorders of both known and unknown etiology, characterized by eosinophils in alveolar and interstitial spaces, usually accompanied by blood eosinophilia (Travis: Non-Neoplastic Disorders of the Lower Respiratory Tract, 1st Edition, 2002).
These disorders may be caused by infections (parasites, HIV or fungi, particularly Aspergillus), drug reactions (antibiotics, cytotoxic or anti-inflammatory drugs), immune disorders (Churg-Strauss syndrome, collagen vascular disease, asthma or hypereosinophilic syndrome) or tobacco (flavored cigars, new onset of smoking (Chest 2007;131:1234, JAMA 2004;292:2997). Idiopathic eosinophilic pneumonia is classified as simple, acute or chronic.
Simple eosinophilic pneumonia, also called Loeffler syndrome, is a self limited disorder with no / minimal symptoms and often transient peripheral eosinophilia and radiographic opacities.
Acute eosinophilic pneumonia has its onset in 1 - 4 days and is accompanied by fever, cough, dyspnea and chest pain. Prominent eosinophils are present in bronchoalveolar lavage fluid and diffuse alveolar damage is identified at biopsy (Am J Respir Crit Care Med 2002;166:1235).
Chronic eosinophilic pneumonia resembles the acute form but with an insidious onset, usually in months and additional symptoms of weight loss and drenching night sweats. It is often associated with asthma, a high peripheral eosinophil count and distinct radiographic findings (Orphanet J Rare Dis 2006;1:11). Biopsy shows tissue eosinophilia and possibly fibrin but no diffuse alveolar damage. Both acute and chronic eosinophilic pneumonia respond dramatically to corticosteroids.