6 December 2007 - Case #103
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Renuka Agrawal, Loma Linda University Medical Center, California (USA).

ARUP Laboratories’ Surgical Pathology Workshop is scheduled for January 27 to February 1, 2008 at the Shadow Ridge Resort Hotel in Park City, Utah.
This five-day course is designed to address the activities and issues faced by the surgical pathologist – featuring short lectures and case-oriented discussions led by distinguished faculty from the University of Utah and ARUP Laboratories.
University of Utah School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to sponsor continuing medical education for physicians.
Advertisement
Case #103
Clinical history:
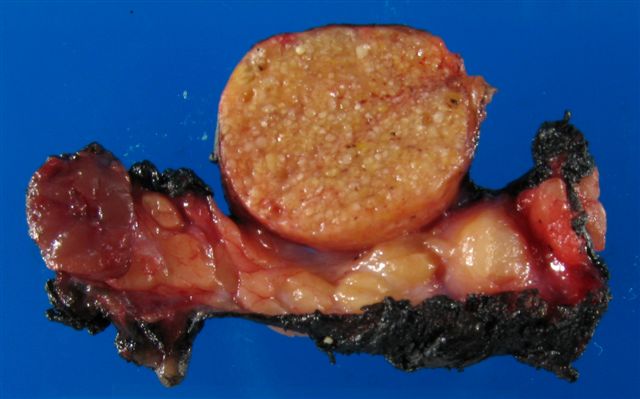
An 86 year old man had a stable parotid mass for 20 years, which was excised. On gross examination, there was a 3 cm well circumscribed tan nodule and a smaller, 7 mm brown-red nodule.
Gross image:
Cytology image:
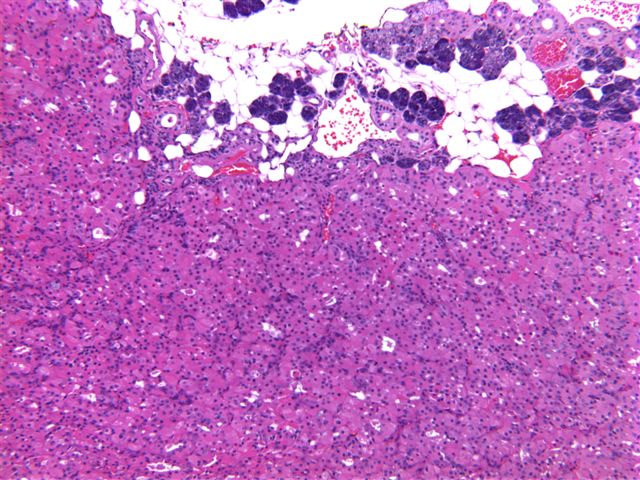
Microscopic images:
What is your diagnosis?
Diagnosis: Sebaceous lymphadenoma and small oncocytoma / oncocytic nodule
Discussion:
Sebaceous lymphadenoma is a rare, benign tumor with nests and islands of bland epithelium composed in part of sebaceous elements, in a prominent lymphoid stroma. Over 90% occur in or near the parotid gland. It is not usually diagnosed prior to excision (Acta Otorhinolaryngol Ital 2007;27:144).
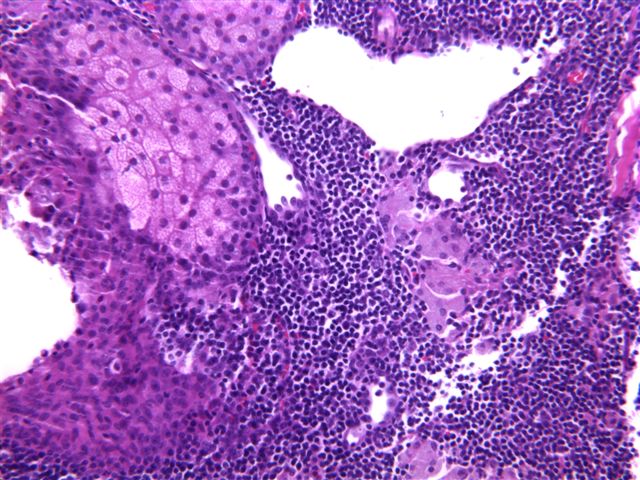
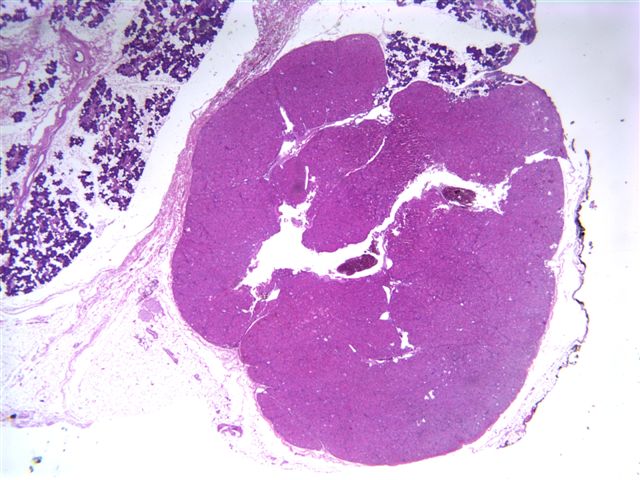
On gross examination, there is a solid or cystic, well circumscribed, tan-yellow mass, up to 3 cm, with variable encapsulation. Microscopically, there are nests and islands of benign squamous cells, often lining a cyst. The epithelial nests have focal areas of sebaceous differentiation. The background is a prominent lymphoid infiltrate, often with germinal centers. There may be an associated foreign body reaction, collections of histiocytes or oncocytic change.
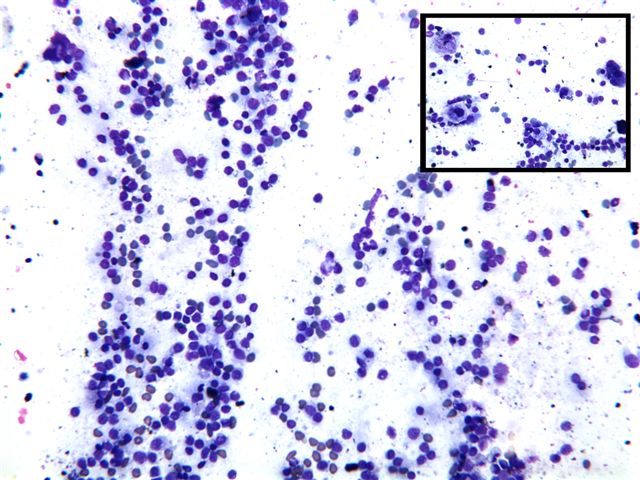
Fine needle aspiration shows a mixed population of large and small lymphocytes, plasma cells and occasional tingible body macrophages. There are also 3 dimensional, cohesive aggregates of epithelial cells, often with cytoplasmic vacuoles characteristic of sebaceous differentiation, surrounded by layers of basaloid cells (Acta Cytol 2004;48:551).
The differential diagnosis includes normal sebaceous glands (present in 10% of parotid glands but not forming a mass), Warthin tumor and low grade mucoepidermoid carcinoma. Warthin tumor has prominent cysts and lymphoid stroma but the cysts have a bilayered oncocytic epithelium, not present in sebaceous lymphadenoma. However, sebaceous lymphadenoma may have collections of oncocytes or a distinct oncocytic nodule as in this case and both tumors may arise from salivary duct inclusions within a parotid lymph node (Am J Clin Pathol 1980;74:683).
Low grade mucoepidermoid carcinoma may also be cystic and contains epithelial islands and mucinous cells that may resemble sebaceous glands. However, in mucoepidermoid carcinoma, the epithelial islands, ducts and cysts tend to be haphazardly distributed with variable shapes and sizes. There is usually infiltration of connective tissue or parenchyma and the cells have some atypia. Mucin stains are positive within the cells, in contrast to sebaceous lymphadenoma.
Excision of sebaceous lymphadenoma is curative, with no recurrences. Only rarely does it undergo malignant transformation (Eur Arch Otorhinolaryngol 2006;263:940).
References: Ellis: Tumors of the Salivary Glands, 1996, Arch Pathol Lab Med 2005;129:e171, University of Pittsburgh: Case 281 [Accessed 15 May 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Renuka Agrawal, Loma Linda University Medical Center, California (USA).

ARUP Laboratories’ Surgical Pathology Workshop is scheduled for January 27 to February 1, 2008 at the Shadow Ridge Resort Hotel in Park City, Utah.
This five-day course is designed to address the activities and issues faced by the surgical pathologist – featuring short lectures and case-oriented discussions led by distinguished faculty from the University of Utah and ARUP Laboratories.
University of Utah School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to sponsor continuing medical education for physicians.
Website news:
(1) Visit our newly updated Breast-nonmalignant chapter. It contains extensive information about 102 topics, including embryology, congenital anomalies, procedures, inflammatory disorders, fibrocystic changes, adenosis, benign tumors / changes and ADH / ALH. If it has been described, we probably have information about it. There are also 969 relevant image links, 712 references, 25 virtual slides and even 9 videos of slides being examined.
Visit and follow our Blog to see recent updates to the website.
(1) Visit our newly updated Breast-nonmalignant chapter. It contains extensive information about 102 topics, including embryology, congenital anomalies, procedures, inflammatory disorders, fibrocystic changes, adenosis, benign tumors / changes and ADH / ALH. If it has been described, we probably have information about it. There are also 969 relevant image links, 712 references, 25 virtual slides and even 9 videos of slides being examined.
Visit and follow our Blog to see recent updates to the website.
Case #103
Clinical history:
An 86 year old man had a stable parotid mass for 20 years, which was excised. On gross examination, there was a 3 cm well circumscribed tan nodule and a smaller, 7 mm brown-red nodule.
Gross image:
Cytology image:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Sebaceous lymphadenoma and small oncocytoma / oncocytic nodule
Discussion:
Sebaceous lymphadenoma is a rare, benign tumor with nests and islands of bland epithelium composed in part of sebaceous elements, in a prominent lymphoid stroma. Over 90% occur in or near the parotid gland. It is not usually diagnosed prior to excision (Acta Otorhinolaryngol Ital 2007;27:144).
On gross examination, there is a solid or cystic, well circumscribed, tan-yellow mass, up to 3 cm, with variable encapsulation. Microscopically, there are nests and islands of benign squamous cells, often lining a cyst. The epithelial nests have focal areas of sebaceous differentiation. The background is a prominent lymphoid infiltrate, often with germinal centers. There may be an associated foreign body reaction, collections of histiocytes or oncocytic change.
Fine needle aspiration shows a mixed population of large and small lymphocytes, plasma cells and occasional tingible body macrophages. There are also 3 dimensional, cohesive aggregates of epithelial cells, often with cytoplasmic vacuoles characteristic of sebaceous differentiation, surrounded by layers of basaloid cells (Acta Cytol 2004;48:551).
The differential diagnosis includes normal sebaceous glands (present in 10% of parotid glands but not forming a mass), Warthin tumor and low grade mucoepidermoid carcinoma. Warthin tumor has prominent cysts and lymphoid stroma but the cysts have a bilayered oncocytic epithelium, not present in sebaceous lymphadenoma. However, sebaceous lymphadenoma may have collections of oncocytes or a distinct oncocytic nodule as in this case and both tumors may arise from salivary duct inclusions within a parotid lymph node (Am J Clin Pathol 1980;74:683).
Low grade mucoepidermoid carcinoma may also be cystic and contains epithelial islands and mucinous cells that may resemble sebaceous glands. However, in mucoepidermoid carcinoma, the epithelial islands, ducts and cysts tend to be haphazardly distributed with variable shapes and sizes. There is usually infiltration of connective tissue or parenchyma and the cells have some atypia. Mucin stains are positive within the cells, in contrast to sebaceous lymphadenoma.
Excision of sebaceous lymphadenoma is curative, with no recurrences. Only rarely does it undergo malignant transformation (Eur Arch Otorhinolaryngol 2006;263:940).
References: Ellis: Tumors of the Salivary Glands, 1996, Arch Pathol Lab Med 2005;129:e171, University of Pittsburgh: Case 281 [Accessed 15 May 2024]