23 June 2005 - Case #11
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Hind Warzecha (formerly Nassar), Wayne State University Department of Pathology, Detroit, Michigan, USA.
Case #11
Clinical history:
Clinical information was not available, but a typical patient is a woman in her 60s with a breast mass.
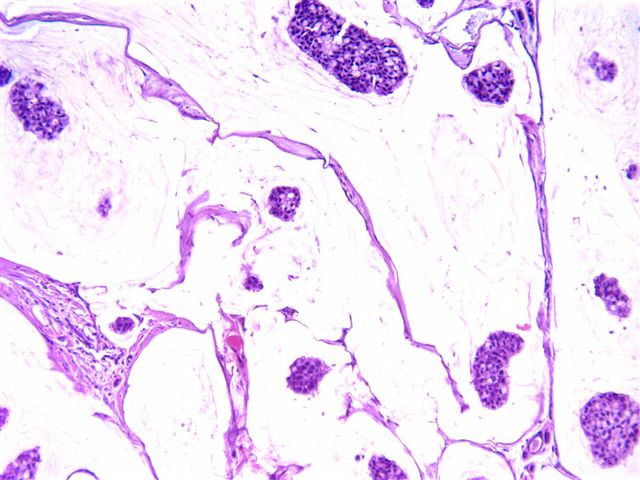
Microscopic images:
What is your diagnosis?
Diagnosis: Colloid (mucinous) carcinoma of the breast
Discussion:
Colloid carcinoma of the breast, also known as mucinous carcinoma, represents approximately 3% of breast carcinomas. It typically affects elderly women, has slow growth and a ten year survival of 90% or greater. Nodal metastases occur in only 2 - 4% of patients. The tumors grossly are soft, pale, gray-blue with a gelatin-like consistency. Hemorrhagic foci are common. Microscopically, the tumors consist of well circumscribed lakes of lightly staining extracellular mucin that dissect tissue spaces and contain individual or small clusters of malignant cells with low grade features and a low mitotic rate. There is usually no in situ component. These tumors are usually immunoreactive for estrogen and progesterone receptors, and 25 - 50% have neuroendocrine features. They are usually negative for HER2 and p53.
Most authors require these tumors to have the above histologic features in > 90% of the tumor (100% for some authors). If these features are present in 75 - 90% of the tumor, it may be considered a variant of colloid (mucinous) carcinoma, with a prognosis worse than pure colloid carcinoma and dependent on the grade of the remaining carcinoma component. It is important to limit the use of the terminology of colloid or mucinous carcinoma to neoplasms which have these features almost exclusively (> 90%) to preserve the clinical characteristics associated with these tumors.
Recent articles have indicated that the favorable prognosis of these tumors in the breast, as well as in the pancreas, may be due to inverse polarization of the cells, leading to mucin secretion towards the stroma (not just to the luminal surface) and extracellular mucin accumulation, which may act as a containing factor to prevent spread of the tumor cells. These tumors are also immunoreactive for MUC2, which is only rarely found in infiltrating ductal carcinomas (Am J Surg Pathol 2003;27:571, Histopathology 2003;42:26, Hum Pathol 1998;29:1517). Of note, the reversal of cell orientation for MUC1 (not MUC2) is an important factor in the morphogenesis and possibly the pathogenesis of invasive micropapillary carcinoma of the breast (Case #4).
The differential diagnosis of colloid carcinoma includes signet ring cell carcinoma, which has intracellular but not extracellular mucin and infiltrating ductal carcinoma with focal mucinous change.
With fine needle aspiration, colloid carcinoma is typically moderate to markedly cellular with mild to moderate atypia and no oval bare nuclei. There are also thin walled capillaries. Marked atypia is not present in pure cases but may be present in tumors with mixed colloid and infiltrating ductal carcinoma histology. The differential diagnosis of tumors with abundant extracellular mucin includes myxoid fibroadenomas, infiltrating ductal carcinoma and fibrocystic changes. Myxoid fibroadenomas may also be markedly cellular with dyscohesion and variable atypia but they have stromal fragments and oval bare nuclei in every case. Infiltrating ductal adenocarcinoma shows marked atypia (Am J Clin Pathol 2003;120:194)
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Hind Warzecha (formerly Nassar), Wayne State University Department of Pathology, Detroit, Michigan, USA.
Website news:
(1) This week's case is sponsored by Invitrogen. The Zymed EGFr antibody clone 31G7 is the most widely referenced clone and the industry standard for EGFr detection in formalin-fixed, paraffin embedded (FFPE) tissue samples. Zymed's 31G7 antibody is extremely specific for EGFr and does not react with the highly homologous c-erbB-2 (HER2) protein. Invitrogen now offers the Zymed 31G7 antibody clone as part of a convenient, standardized immunohistochemical kit for the detection of EGFr protein expression in normal and neoplastic tissue. Invitrogen's Zymed EGFr Kit is compatible with manual or automated immunostainers and offers the greatest flexibility with FFPE tissue samples. For more information, visit www.invitrogen.com/antibodies. Note: sponsors do NOT have access in any manner to email addresses or other personal information in the possession of PathologyOutlines.com.
Visit and follow our Blog to see recent updates to the website.
(1) This week's case is sponsored by Invitrogen. The Zymed EGFr antibody clone 31G7 is the most widely referenced clone and the industry standard for EGFr detection in formalin-fixed, paraffin embedded (FFPE) tissue samples. Zymed's 31G7 antibody is extremely specific for EGFr and does not react with the highly homologous c-erbB-2 (HER2) protein. Invitrogen now offers the Zymed 31G7 antibody clone as part of a convenient, standardized immunohistochemical kit for the detection of EGFr protein expression in normal and neoplastic tissue. Invitrogen's Zymed EGFr Kit is compatible with manual or automated immunostainers and offers the greatest flexibility with FFPE tissue samples. For more information, visit www.invitrogen.com/antibodies. Note: sponsors do NOT have access in any manner to email addresses or other personal information in the possession of PathologyOutlines.com.
Visit and follow our Blog to see recent updates to the website.
Case #11
Clinical history:
Clinical information was not available, but a typical patient is a woman in her 60s with a breast mass.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Colloid (mucinous) carcinoma of the breast
Discussion:
Colloid carcinoma of the breast, also known as mucinous carcinoma, represents approximately 3% of breast carcinomas. It typically affects elderly women, has slow growth and a ten year survival of 90% or greater. Nodal metastases occur in only 2 - 4% of patients. The tumors grossly are soft, pale, gray-blue with a gelatin-like consistency. Hemorrhagic foci are common. Microscopically, the tumors consist of well circumscribed lakes of lightly staining extracellular mucin that dissect tissue spaces and contain individual or small clusters of malignant cells with low grade features and a low mitotic rate. There is usually no in situ component. These tumors are usually immunoreactive for estrogen and progesterone receptors, and 25 - 50% have neuroendocrine features. They are usually negative for HER2 and p53.
Most authors require these tumors to have the above histologic features in > 90% of the tumor (100% for some authors). If these features are present in 75 - 90% of the tumor, it may be considered a variant of colloid (mucinous) carcinoma, with a prognosis worse than pure colloid carcinoma and dependent on the grade of the remaining carcinoma component. It is important to limit the use of the terminology of colloid or mucinous carcinoma to neoplasms which have these features almost exclusively (> 90%) to preserve the clinical characteristics associated with these tumors.
Recent articles have indicated that the favorable prognosis of these tumors in the breast, as well as in the pancreas, may be due to inverse polarization of the cells, leading to mucin secretion towards the stroma (not just to the luminal surface) and extracellular mucin accumulation, which may act as a containing factor to prevent spread of the tumor cells. These tumors are also immunoreactive for MUC2, which is only rarely found in infiltrating ductal carcinomas (Am J Surg Pathol 2003;27:571, Histopathology 2003;42:26, Hum Pathol 1998;29:1517). Of note, the reversal of cell orientation for MUC1 (not MUC2) is an important factor in the morphogenesis and possibly the pathogenesis of invasive micropapillary carcinoma of the breast (Case #4).
The differential diagnosis of colloid carcinoma includes signet ring cell carcinoma, which has intracellular but not extracellular mucin and infiltrating ductal carcinoma with focal mucinous change.
With fine needle aspiration, colloid carcinoma is typically moderate to markedly cellular with mild to moderate atypia and no oval bare nuclei. There are also thin walled capillaries. Marked atypia is not present in pure cases but may be present in tumors with mixed colloid and infiltrating ductal carcinoma histology. The differential diagnosis of tumors with abundant extracellular mucin includes myxoid fibroadenomas, infiltrating ductal carcinoma and fibrocystic changes. Myxoid fibroadenomas may also be markedly cellular with dyscohesion and variable atypia but they have stromal fragments and oval bare nuclei in every case. Infiltrating ductal adenocarcinoma shows marked atypia (Am J Clin Pathol 2003;120:194)