7 April 2010 - Case #176
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Renuka Agrawal, City of Hope National Medical Center, Duarte, California (USA), for contributing this case and the discussion.
bioTheranostics announces the launch of an expanded tumor-type database for its flagship product, CancerTYPE ID, and the launch of KRAS mutational testing.
CancerTYPE ID predicts cancer origin in patients whose primary cancer was initially unknown or uncertain using conventional diagnostics. Knowing the site where the cancer originated impacts physicians therapeutic decisions, and the results of the CancerTYPE ID assay can help physicians select optimal therapies earlier in the diagnostic process. This new database enhances the ability of the CancerTYPE ID assay to discriminate between clinically relevant metastatic tumors occurring within the GI tract, head and neck, lung (squamous, non-squamous adenocarcinoma, and mesothelioma), and intestine, while incorporating coverage of certain tumor types that frequently present diagnostic challenges such as cholangiocarcinoma, ovarian-mucinous adenocarcinoma, and small intestinal carcinoma.
bioTheranostics is working on developing additional tests including prostate cancer prognosis and drug-response profiling.
Advertisement
Case #176
Clinical history:
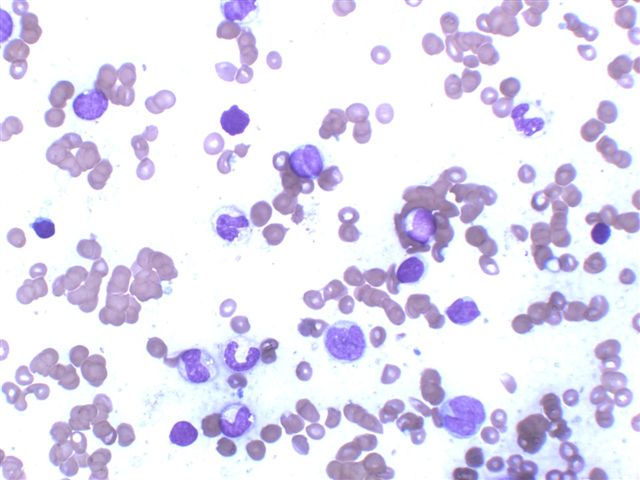
A 66 year old man presented with increasing left upper quadrant abdominal pain of two weeks duration. Physical examination showed splenomegaly and multiple violaceous, indurated, non-erythematous cutaneous nodules on the back and torso, ranging from 3 to 6 cm in diameter. A CT scan showed splenomegaly and mild abdominal lymphadenopathy, as well as scattered small lymph nodes in the pretracheal region, suspicious for lymphoma. The patient had pancytopenia with 6% atypical mononuclear cells in the peripheral blood. Skin and bone marrow biopsies were obtained.
Clinical images:
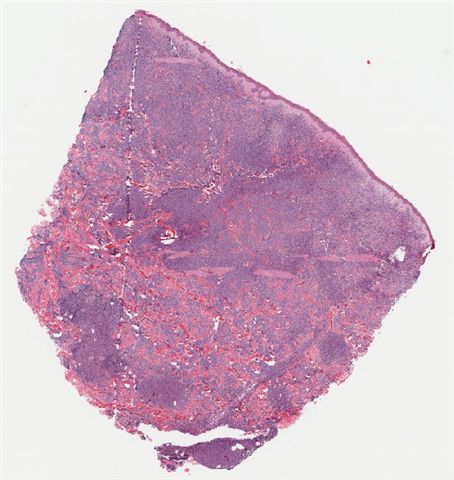
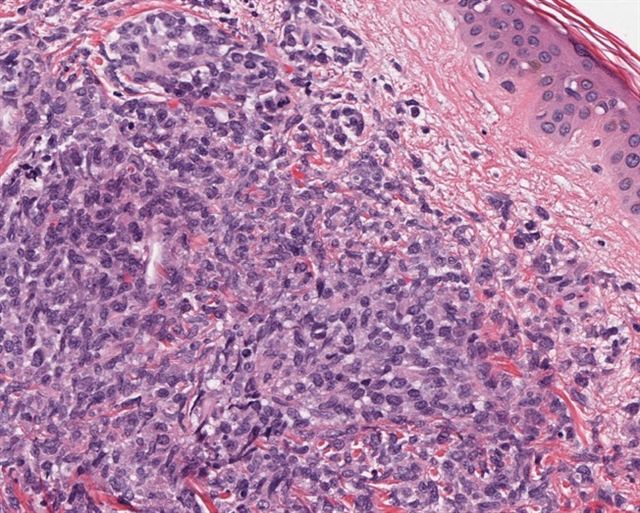
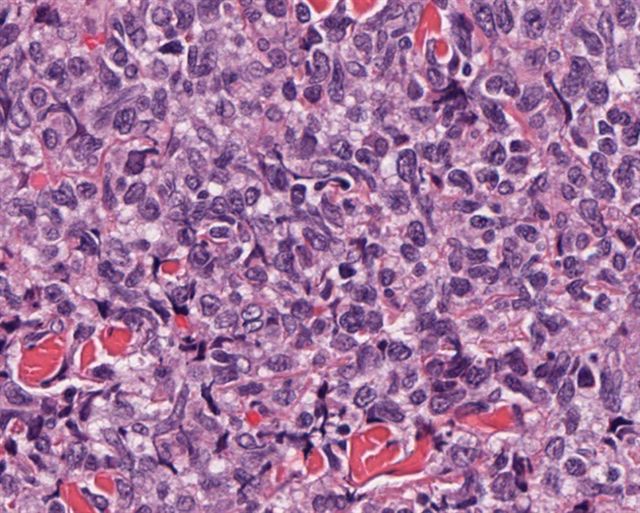
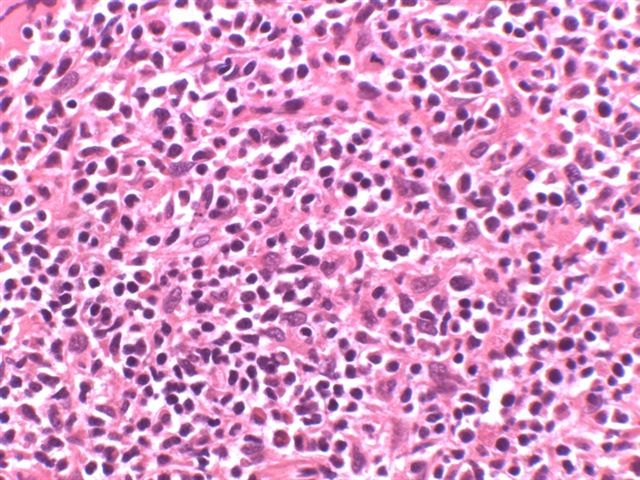
Microscopic images:
What is your diagnosis?
Diagnosis: Blastic plasmacytoid dendritic cell neoplasm (formerly called CD4+ / CD56+ hematodermic neoplasm)
Discussion:
Blastic plasmacytoid dendritic cell neoplasm, called CD4+ CD56+ hematodermic neoplasm prior to 2008, is a rare malignancy, first described in 1994 (Am J Hematol 1994;47:278). It typically affects middle aged or elderly patients, usually men, who present with widespread skin infiltration (purplish papules, nodules or bruise-like skin lesions), that have a predilection for the trunk but also involve the extremities and the head and neck. This is closely followed by lymph node, spleen and bone marrow involvement, often terminating in the leukemic phase with a fatal course.
Histologically, these tumors involve the dermis and sometimes the subcutaneous tissue but show no epidermotropism. The infiltrates are composed of monotonous, medium sized mononuclear cells, with sparse cytoplasm and finely dispersed chromatin and absent or indistinct nucleoli resembling lymphoblasts or myeloblasts. Frequent mitotic figures may be seen but there is generally no necrosis or angioinvasion.
The cell of origin is believed to be a plasmacytoid dendritic cell precursor which appears to be related to plasmacytoid monocytes, because it also expresses CD68 and bright levels of CD123 (Hum Pathol 2005;36:1020, Am J Surg Pathol 2002;26:852). Expression of high levels of CD123 (IL3 receptor alpha chain) is a distinctive characteristic of plasmacytoid monocytes and HDN and may have prognostic significance. The tumor cells usually have a CD4+, CD56+, CD8-, CD7 variable, CD2 variable, CD43+, CD45RA+ phenotype and do not express surface and cytoplasmic CD3 or cytotoxic proteins. TdT may be positive. These tumors were initially called blastic NK lymphomas, because their phenotype is similar to NK cells (CD4+, CD56+), then CD4+ CD56+ hematodermic neoplasms and in 2008, received their present name from the WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Arch Pathol Lab Med 2007;131:149, Blood 2005;105:3768, IARC: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue, 4th Edition, 2008)
As lymphoblastic and myeloblastic neoplasms can also be positive for CD56, stains for CD3 and myeloperoxidase should always be performed to exclude them. Rarely, myelomonocytic cells coexpress CD4, CD56 and CD123 but they also stain for myeloperoxidase, in contrast to HDN.
Blastic plasmacytoid dendritic cell neoplasm is characterized by highly aggressive behavior and poor prognosis with a median survival time of 14 months. Patients are best treated with regimes used in acute leukemias. Although chemotherapy usually results in complete remission, there is almost always a quick relapse unresponsive to further chemotherapy (Blood 2002;99:1556).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Renuka Agrawal, City of Hope National Medical Center, Duarte, California (USA), for contributing this case and the discussion.
bioTheranostics announces the launch of an expanded tumor-type database for its flagship product, CancerTYPE ID, and the launch of KRAS mutational testing.
CancerTYPE ID predicts cancer origin in patients whose primary cancer was initially unknown or uncertain using conventional diagnostics. Knowing the site where the cancer originated impacts physicians therapeutic decisions, and the results of the CancerTYPE ID assay can help physicians select optimal therapies earlier in the diagnostic process. This new database enhances the ability of the CancerTYPE ID assay to discriminate between clinically relevant metastatic tumors occurring within the GI tract, head and neck, lung (squamous, non-squamous adenocarcinoma, and mesothelioma), and intestine, while incorporating coverage of certain tumor types that frequently present diagnostic challenges such as cholangiocarcinoma, ovarian-mucinous adenocarcinoma, and small intestinal carcinoma.
bioTheranostics is working on developing additional tests including prostate cancer prognosis and drug-response profiling.
Website news:
(1) We are updating the Bladder and Breast-nonmalignant chapters.
(2) Thanks to all who have offered to review chapters, sections of chapters or topics. We have to review and organize all of the offers, and will respond within 1-2 weeks.
Visit and follow our Blog to see recent updates to the website.
(1) We are updating the Bladder and Breast-nonmalignant chapters.
(2) Thanks to all who have offered to review chapters, sections of chapters or topics. We have to review and organize all of the offers, and will respond within 1-2 weeks.
Visit and follow our Blog to see recent updates to the website.
Case #176
Clinical history:
A 66 year old man presented with increasing left upper quadrant abdominal pain of two weeks duration. Physical examination showed splenomegaly and multiple violaceous, indurated, non-erythematous cutaneous nodules on the back and torso, ranging from 3 to 6 cm in diameter. A CT scan showed splenomegaly and mild abdominal lymphadenopathy, as well as scattered small lymph nodes in the pretracheal region, suspicious for lymphoma. The patient had pancytopenia with 6% atypical mononuclear cells in the peripheral blood. Skin and bone marrow biopsies were obtained.
Clinical images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Blastic plasmacytoid dendritic cell neoplasm (formerly called CD4+ / CD56+ hematodermic neoplasm)
Discussion:
Blastic plasmacytoid dendritic cell neoplasm, called CD4+ CD56+ hematodermic neoplasm prior to 2008, is a rare malignancy, first described in 1994 (Am J Hematol 1994;47:278). It typically affects middle aged or elderly patients, usually men, who present with widespread skin infiltration (purplish papules, nodules or bruise-like skin lesions), that have a predilection for the trunk but also involve the extremities and the head and neck. This is closely followed by lymph node, spleen and bone marrow involvement, often terminating in the leukemic phase with a fatal course.
Histologically, these tumors involve the dermis and sometimes the subcutaneous tissue but show no epidermotropism. The infiltrates are composed of monotonous, medium sized mononuclear cells, with sparse cytoplasm and finely dispersed chromatin and absent or indistinct nucleoli resembling lymphoblasts or myeloblasts. Frequent mitotic figures may be seen but there is generally no necrosis or angioinvasion.
The cell of origin is believed to be a plasmacytoid dendritic cell precursor which appears to be related to plasmacytoid monocytes, because it also expresses CD68 and bright levels of CD123 (Hum Pathol 2005;36:1020, Am J Surg Pathol 2002;26:852). Expression of high levels of CD123 (IL3 receptor alpha chain) is a distinctive characteristic of plasmacytoid monocytes and HDN and may have prognostic significance. The tumor cells usually have a CD4+, CD56+, CD8-, CD7 variable, CD2 variable, CD43+, CD45RA+ phenotype and do not express surface and cytoplasmic CD3 or cytotoxic proteins. TdT may be positive. These tumors were initially called blastic NK lymphomas, because their phenotype is similar to NK cells (CD4+, CD56+), then CD4+ CD56+ hematodermic neoplasms and in 2008, received their present name from the WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Arch Pathol Lab Med 2007;131:149, Blood 2005;105:3768, IARC: WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue, 4th Edition, 2008)
As lymphoblastic and myeloblastic neoplasms can also be positive for CD56, stains for CD3 and myeloperoxidase should always be performed to exclude them. Rarely, myelomonocytic cells coexpress CD4, CD56 and CD123 but they also stain for myeloperoxidase, in contrast to HDN.
Blastic plasmacytoid dendritic cell neoplasm is characterized by highly aggressive behavior and poor prognosis with a median survival time of 14 months. Patients are best treated with regimes used in acute leukemias. Although chemotherapy usually results in complete remission, there is almost always a quick relapse unresponsive to further chemotherapy (Blood 2002;99:1556).