20 January 2010 - Case #166
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Mohammed Sami Saeed, College of Medicine, University of Mosul, Mosul, Iraq, for contributing this case.



This 24.25 hour review and update in the areas of clinical chemistry, immunology, microbiology, and molecular medicine is intended to improve knowledge about the pathogenesis and clinical manifestations of a wide variety of metabolic, infectious, immunologic, and genetic disorders along with the selection, performance, and interpretation of clinical laboratory tests.
Course Directors: Harry R. Hill, MD, Elaine Lyon, PhD and William L. Roberts, MD, PhD
Special Guests: Robert Christenson, PhD, DABCC, FACB, Andrea Ferreira-Gonzalez, PhD and Steven M. Holland, MD
Advertisement
Case #166
Clinical history:
An 8 month old infant presented with difficulty in feeding and shortness of breath. Xray findings showed a right upper lobe lung mass.
The mass was a large, solid, firm, whitish gray lobulated tumor measuring 13 x 8 x 7 cm and weighing 280 g. Cut sections showed foci of necrosis and cystic spaces.
Gross images:
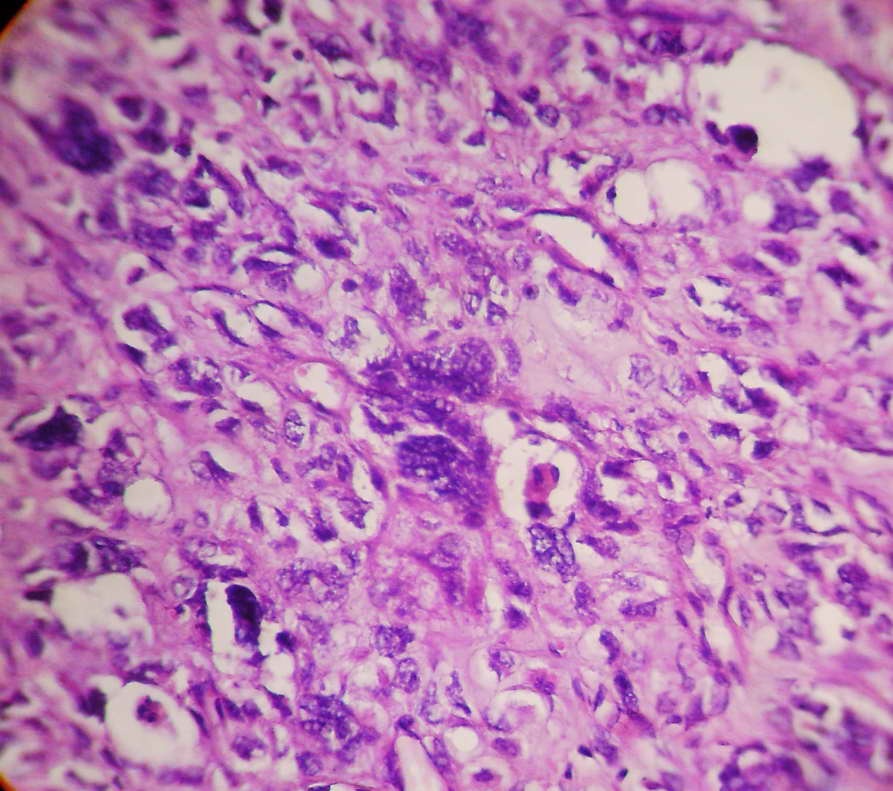
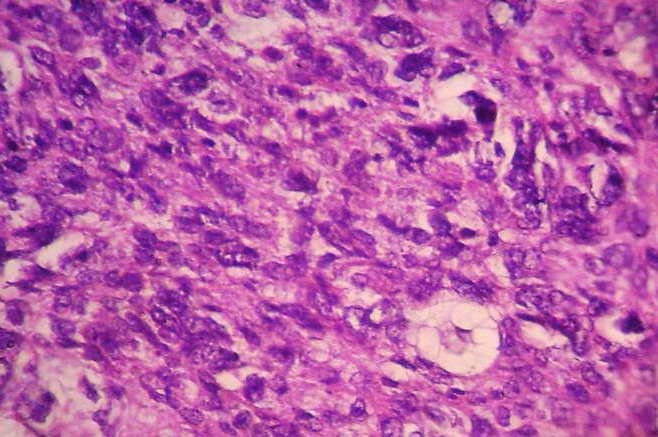
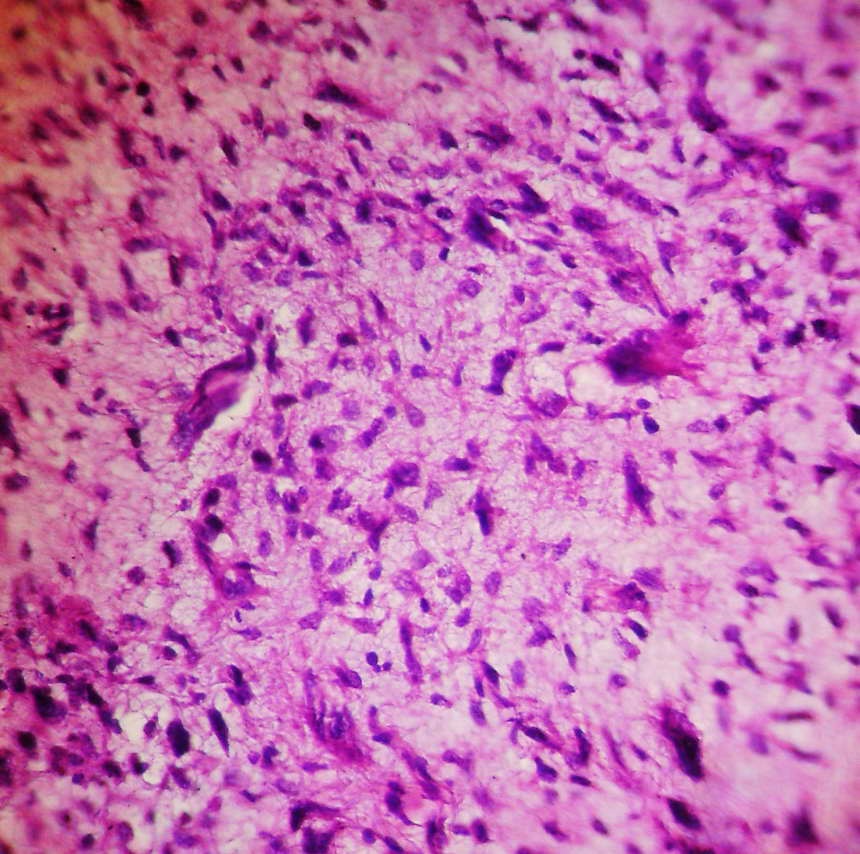
Microscopic images:
What is your diagnosis?
Diagnosis: Type III pleuropulmonary blastoma
Discussion:
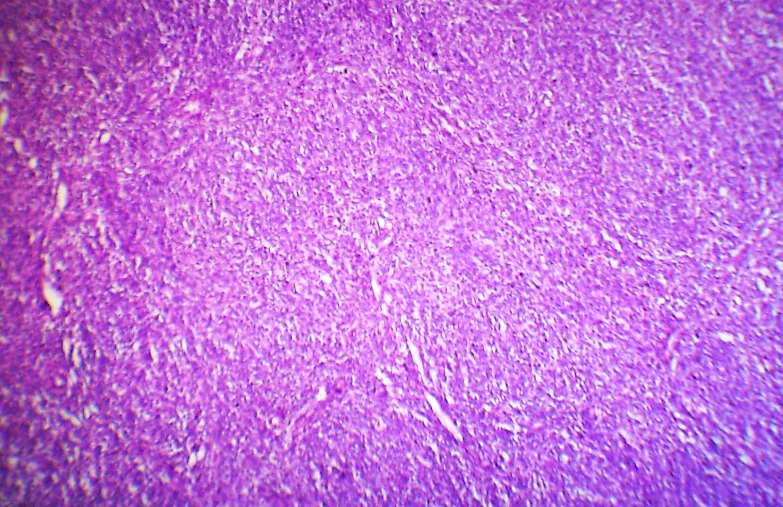
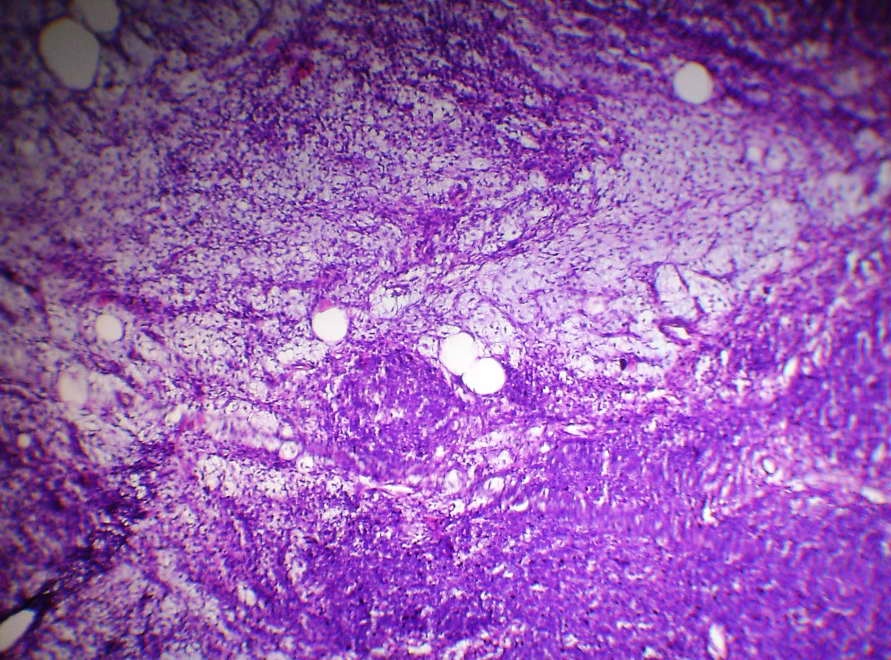
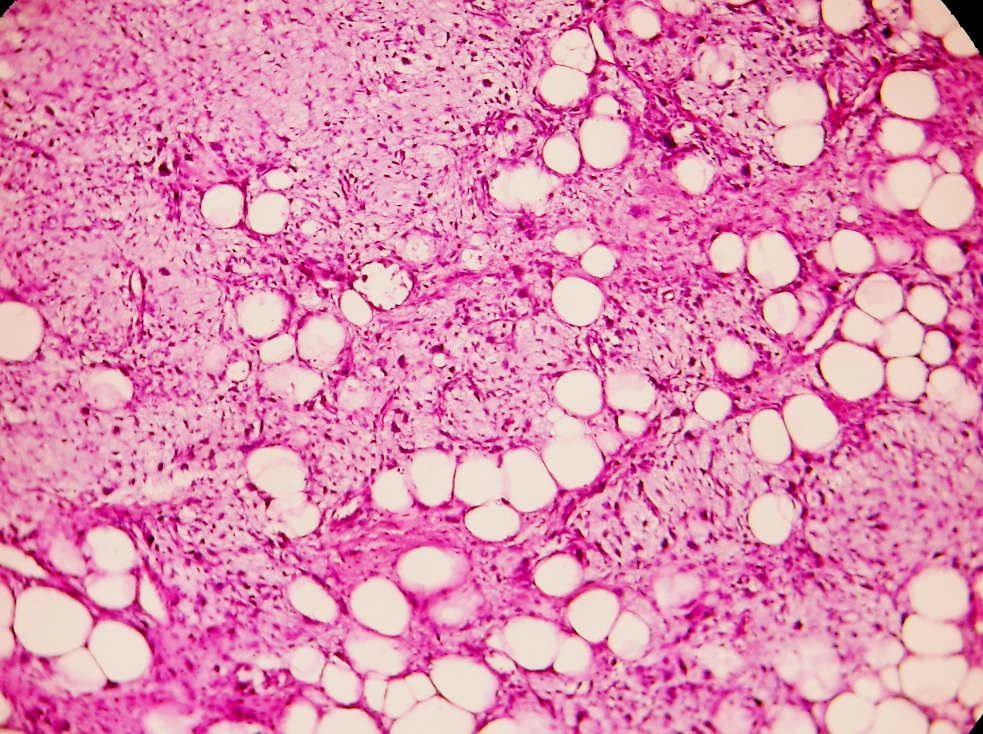
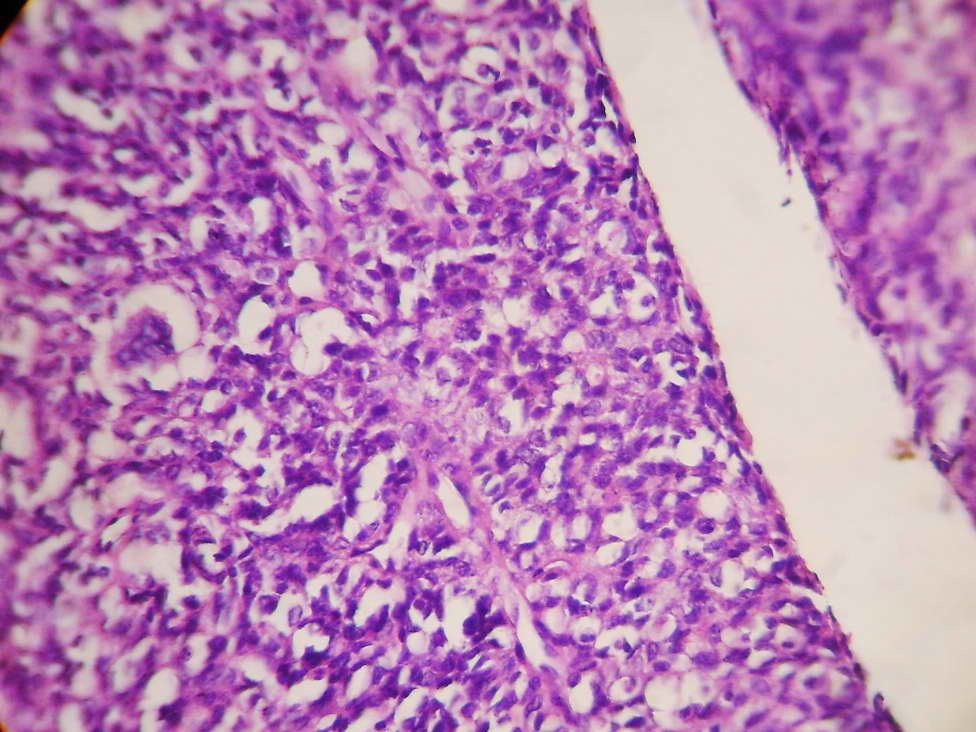
Microscopically, the tumor was composed of primitive, undifferentiated blastema cells and sarcomatous elements of different types of differentiation, including lipoblastic, chondroblastic, rhabdomyoblastic and giant cell undifferentiated sarcomas. Cystic and slit-like spaces lined by the primitive or sarcomatous cells were identified. Multiple foci of necrosis were present. These features are consistent with type III pleuropulmonary blastoma.
Pleuropulmonary blastoma (PPB) is a childhood tumor of the lung or pleura that usually occurs in children age 4 years or younger. Although rare overall, it is one of the most common primary lung malignancies in children (Arch Pathol Lab Med 2008;132:1079, The International Pleuropulmonary Blastoma/DICER1 Registry [Accessed 25 April 2024]).
It was first described in 1988 and is classified into 3 types (Cancer 1988;62:1516):
Children usually present with difficulty breathing or other respiratory problems. MRI or CT can help diagnose, though biopsy is suggested (Pediatr Radiol 2007;37:337). Microscopically, PPB shows mixed blastematous and sarcomatous appearance and primitive cells (Singapore Med J 2007;48:e190).
The differential diagnosis for type III cases is broad, because of the histologic variability. Many tumors may resemble embryonal rhabdomyosarcoma but PPB also has cystic architectural, blastema tissue and other mesenchymal components such as cartilage. In addition, primary pulmonary or pleural rhabdomyosarcoma is extremely rare. Other tumors to consider include monophasic synovial sarcoma, malignant peripheral nerve sheath tumor, mesothelioma, malignant teratoma and undifferentiated sarcoma. Immunostains are typically not helpful in differentiating these entities. A recent finding that may prove helpful is the frequent presence of gains in chromosome 8q in PPB (Mod Pathol 2007;20:1191).
Treatment is radical surgery to excise the cyst or mass, with extensive follow up to detect relapses. Chemotherapy is usually provided for types II and III. Half of patients eventually develop cerebral metastases (Pediatr Blood Cancer 2007;49:266).
Reference: J Pediatr Oncol Nurs 2008;25:295
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Mohammed Sami Saeed, College of Medicine, University of Mosul, Mosul, Iraq, for contributing this case.



This 24.25 hour review and update in the areas of clinical chemistry, immunology, microbiology, and molecular medicine is intended to improve knowledge about the pathogenesis and clinical manifestations of a wide variety of metabolic, infectious, immunologic, and genetic disorders along with the selection, performance, and interpretation of clinical laboratory tests.
Course Directors: Harry R. Hill, MD, Elaine Lyon, PhD and William L. Roberts, MD, PhD
Special Guests: Robert Christenson, PhD, DABCC, FACB, Andrea Ferreira-Gonzalez, PhD and Steven M. Holland, MD
Website news:
(1) We are updating the staging sections of all of our chapters based on AJCC Cancer Staging Manual (7th Edition).
(2) Visit us at USCAP in Washington, D.C., booth #1303. We are proud to be a sponsor of USCAP, specifically of the Speaker Preview Room. Stop by our booth and let us know how we can make PathologyOutlines.com more useful to you.
(3) We posted a new article, Underpayment of Pathology Technical Component, by Mick Raich, Vachette Pathology, on our Management Page.
(4) In the past week, we have been reading about and watching the news about the devastation in Haiti. As Pathologists and Laboratory Professionals, we know the great need for medical supplies and the medical care that is going to be required now and in the months to come.
Visit and follow our Blog to see recent updates to the website.
(1) We are updating the staging sections of all of our chapters based on AJCC Cancer Staging Manual (7th Edition).
(2) Visit us at USCAP in Washington, D.C., booth #1303. We are proud to be a sponsor of USCAP, specifically of the Speaker Preview Room. Stop by our booth and let us know how we can make PathologyOutlines.com more useful to you.
(3) We posted a new article, Underpayment of Pathology Technical Component, by Mick Raich, Vachette Pathology, on our Management Page.
(4) In the past week, we have been reading about and watching the news about the devastation in Haiti. As Pathologists and Laboratory Professionals, we know the great need for medical supplies and the medical care that is going to be required now and in the months to come.
Visit and follow our Blog to see recent updates to the website.
Case #166
Clinical history:
An 8 month old infant presented with difficulty in feeding and shortness of breath. Xray findings showed a right upper lobe lung mass.
The mass was a large, solid, firm, whitish gray lobulated tumor measuring 13 x 8 x 7 cm and weighing 280 g. Cut sections showed foci of necrosis and cystic spaces.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Type III pleuropulmonary blastoma
Discussion:
Microscopically, the tumor was composed of primitive, undifferentiated blastema cells and sarcomatous elements of different types of differentiation, including lipoblastic, chondroblastic, rhabdomyoblastic and giant cell undifferentiated sarcomas. Cystic and slit-like spaces lined by the primitive or sarcomatous cells were identified. Multiple foci of necrosis were present. These features are consistent with type III pleuropulmonary blastoma.
Pleuropulmonary blastoma (PPB) is a childhood tumor of the lung or pleura that usually occurs in children age 4 years or younger. Although rare overall, it is one of the most common primary lung malignancies in children (Arch Pathol Lab Med 2008;132:1079, The International Pleuropulmonary Blastoma/DICER1 Registry [Accessed 25 April 2024]).
It was first described in 1988 and is classified into 3 types (Cancer 1988;62:1516):
- Type I is multicystic, and may progress into types II or III
- Type II shows thickened areas within the cysts
- Type III shows solid masses
Children usually present with difficulty breathing or other respiratory problems. MRI or CT can help diagnose, though biopsy is suggested (Pediatr Radiol 2007;37:337). Microscopically, PPB shows mixed blastematous and sarcomatous appearance and primitive cells (Singapore Med J 2007;48:e190).
The differential diagnosis for type III cases is broad, because of the histologic variability. Many tumors may resemble embryonal rhabdomyosarcoma but PPB also has cystic architectural, blastema tissue and other mesenchymal components such as cartilage. In addition, primary pulmonary or pleural rhabdomyosarcoma is extremely rare. Other tumors to consider include monophasic synovial sarcoma, malignant peripheral nerve sheath tumor, mesothelioma, malignant teratoma and undifferentiated sarcoma. Immunostains are typically not helpful in differentiating these entities. A recent finding that may prove helpful is the frequent presence of gains in chromosome 8q in PPB (Mod Pathol 2007;20:1191).
Treatment is radical surgery to excise the cyst or mass, with extensive follow up to detect relapses. Chemotherapy is usually provided for types II and III. Half of patients eventually develop cerebral metastases (Pediatr Blood Cancer 2007;49:266).
Reference: J Pediatr Oncol Nurs 2008;25:295