14 January 2010 - Case #165
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Karen Fritchie, University of North Carolina at Chapel Hill (USA).


This 20-hour workshop is designed to address the activities and issues faced by the surgical pathologist.
The 24th Annual Surgical Pathology Workshop consists of short lectures and case-oriented discussions. Microscopes will be available. Participants will be asked to examine microscopic images and formulate a diagnosis and patient management strategy. The faculty pathologist will then discuss the diagnosis, differential diagnosis, patient management, and other pertinent features. Cases will be selected to represent common and/or difficult diagnostic problems.
This workshop will be held at The Canyons in Park City, Utah. Bring the family and have an incredible winter getaway!
Advertisement
Case #165
Clinical history:
A 4 month old child was found to have a midline skull lesion. She was the product of an uneventful pregnancy and she had no other medical issues. The lesion was excised.
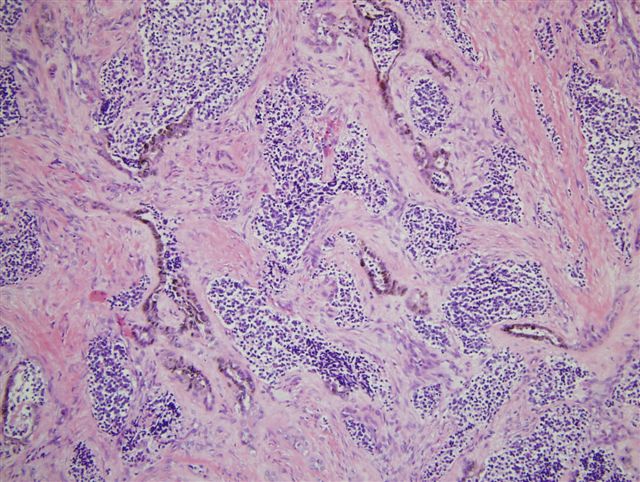
Microscopic images:
What is your diagnosis?
Diagnosis: Pigmented neuroectodermal tumor of infancy
Discussion:
Pigmented neuroectodermal tumor of infancy is an uncommon, rapidly growing mesenchymal tumor that typically occurs in the bones of the jaw or skull in infants in their first year of life (eMedicine: Melanotic Neuroectodermal Tumor of Infancy [Accessed 25 April 2024]). It is a biphasic tumor with tubular or alveolar patterns. It consists of large melanin containing cells with abundant cytoplasm and pale nuclei, surrounding nests of smaller neuroblast-like cells possessing scant or fibrillar cytoplasm. There is usually minimal mitotic activity and no atypia.
The large cells are immunoreactive for keratin and HMB45. The smaller cells are usually immunoreactive for CD57 / Leu7 and NSE. Although the tumor is of neuroectodermal origin, both cell types are usually negative for S100 (Am J Surg Pathol 1993;17:566). Ultrastructurally, the pigmented cells contain melanosomes and the neuroblast-like cells contain neurosecretory granules and cytoplasmic processes.
Pigmented neuroectodermal tumor of infancy was historically called melanotic progonoma or retinal anlage tumor based on the suspected cell of origin. In 1966, Borello and Gorelin reported a patient with this tumor and high urinary excretion of vanilmandelic acid, suggesting a neuroectodermal origin, which has subsequently been confirmed (Cancer 1966;19:196).
The differential diagnosis includes neuroblastoma and other small round blue cell tumors, as well as melanoma. These malignant tumors typically lack the clinical presentation of a jaw or skull tumor in infants, exhibit prominent necrosis, atypia, mitotic figures and lack the biphasic pattern of pigmented neuroectodermal tumor of infancy.
Treatment is excision with negative margins. Recurrence has been reported in 37% of cases, with metastases in 7%, although no prognostic factors have been identified (Fetal Pediatr Pathol 2006;25:59).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Karen Fritchie, University of North Carolina at Chapel Hill (USA).


This 20-hour workshop is designed to address the activities and issues faced by the surgical pathologist.
The 24th Annual Surgical Pathology Workshop consists of short lectures and case-oriented discussions. Microscopes will be available. Participants will be asked to examine microscopic images and formulate a diagnosis and patient management strategy. The faculty pathologist will then discuss the diagnosis, differential diagnosis, patient management, and other pertinent features. Cases will be selected to represent common and/or difficult diagnostic problems.
This workshop will be held at The Canyons in Park City, Utah. Bring the family and have an incredible winter getaway!
Website news:
(1) We are updating the staging sections of all of our chapters based on AJCC Cancer Staging Manual (7th ed).
(2) Visit us at USCAP in Washington, D.C., booth #1303. We are proud to be a sponsor of USCAP, specifically of the Speaker Preview Room. Stop by our booth and let us know how we can make PathologyOutlines.com more useful to you.
Visit and follow our Blog to see recent updates to the website.
(1) We are updating the staging sections of all of our chapters based on AJCC Cancer Staging Manual (7th ed).
(2) Visit us at USCAP in Washington, D.C., booth #1303. We are proud to be a sponsor of USCAP, specifically of the Speaker Preview Room. Stop by our booth and let us know how we can make PathologyOutlines.com more useful to you.
Visit and follow our Blog to see recent updates to the website.
Case #165
Clinical history:
A 4 month old child was found to have a midline skull lesion. She was the product of an uneventful pregnancy and she had no other medical issues. The lesion was excised.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Pigmented neuroectodermal tumor of infancy
Discussion:
Pigmented neuroectodermal tumor of infancy is an uncommon, rapidly growing mesenchymal tumor that typically occurs in the bones of the jaw or skull in infants in their first year of life (eMedicine: Melanotic Neuroectodermal Tumor of Infancy [Accessed 25 April 2024]). It is a biphasic tumor with tubular or alveolar patterns. It consists of large melanin containing cells with abundant cytoplasm and pale nuclei, surrounding nests of smaller neuroblast-like cells possessing scant or fibrillar cytoplasm. There is usually minimal mitotic activity and no atypia.
The large cells are immunoreactive for keratin and HMB45. The smaller cells are usually immunoreactive for CD57 / Leu7 and NSE. Although the tumor is of neuroectodermal origin, both cell types are usually negative for S100 (Am J Surg Pathol 1993;17:566). Ultrastructurally, the pigmented cells contain melanosomes and the neuroblast-like cells contain neurosecretory granules and cytoplasmic processes.
Pigmented neuroectodermal tumor of infancy was historically called melanotic progonoma or retinal anlage tumor based on the suspected cell of origin. In 1966, Borello and Gorelin reported a patient with this tumor and high urinary excretion of vanilmandelic acid, suggesting a neuroectodermal origin, which has subsequently been confirmed (Cancer 1966;19:196).
The differential diagnosis includes neuroblastoma and other small round blue cell tumors, as well as melanoma. These malignant tumors typically lack the clinical presentation of a jaw or skull tumor in infants, exhibit prominent necrosis, atypia, mitotic figures and lack the biphasic pattern of pigmented neuroectodermal tumor of infancy.
Treatment is excision with negative margins. Recurrence has been reported in 37% of cases, with metastases in 7%, although no prognostic factors have been identified (Fetal Pediatr Pathol 2006;25:59).