16 September 2009 - Case #157
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Suhail Muzaffar and Dr. Bilal Karim Siddiqui, City Hospital, Sandwell & West Birmingham NHS Trust (United Kingdom).

We offer dermatopathology, head and neck and ophthalmic pathology consultations for pathology organizations worldwide. Visit our website or call (617) 549-1168 to find out how we can help your practice to establish, grow and promote your subspecialty outreach program and effectively compete with reference laboratories.
Our services, supported by custom-designed digital pathology-ready workflow solution, range from second opinion consultations on difficult cases to providing daily subspecialty signout and short-term coverage.
Find out how recognized experts in the field can support your practice at a fraction of the cost of hiring a full-time dermatopathologist.
Advertisement
Case #157
Clinical history:
A 20 year old Asian woman presented with dyspepsia. An upper GI endoscopy was followed by a gastric antral biopsy, which revealed a moderate acute and chronic inflammatory infiltrate in the lamina propria. There was no evidence of atrophic gastritis, intestinal metaplasia, dysplasia or malignancy.
Microscopic images:
What is your diagnosis?
Diagnosis: Gastric giardiasis
Discussion:
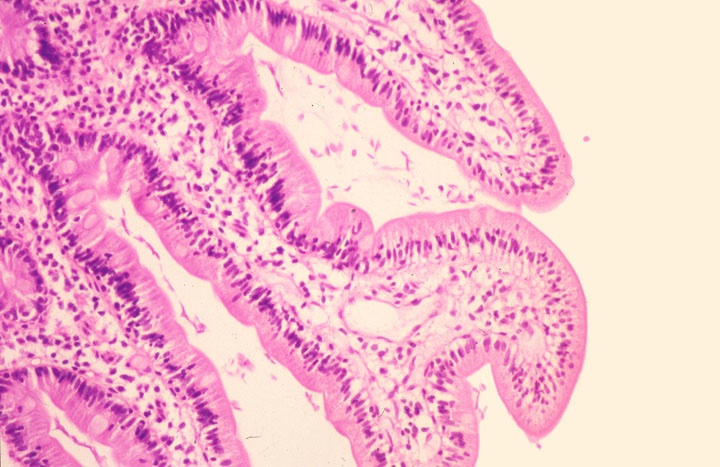
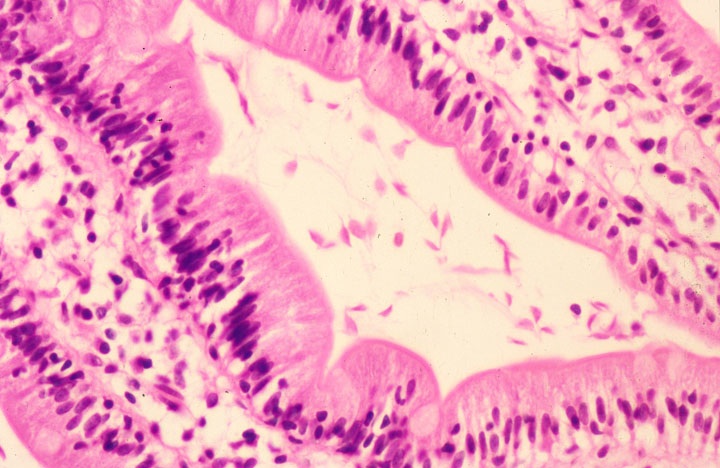
A large number of giardial trophozoites were identified along the surface of foveolar epithelial cells (figure 1). The trophozoites appeared as pear or sickle shaped, lying opposed to the gastric surface and foveolar epithelium (figure 2). No H. pylori organisms were identified.
Giardia lamblia is the most prevalent pathogenic intestinal protozoan and a major contributor to the burden of diarrheal disease worldwide. Giardia can be contracted from contaminated streams or pools, through food or by poor hygienic practices resulting in fecal-oral contact. The trophozoites colonize and reside in the lumen of the small intestine, causing severe diarrhea, vomiting, abdominal cramps and fever. These can lead to anorexia, malaise and fatigue.
In a cohort of 41 cases of gastric giardiasis, it was found that all patients showed moderate to severe chronic atrophic gastritis, with mild to severe activity associated with intestinal metaplasia. Though not seen in this case, concomitant H. pylori infection is common in patients with gastric giardiasis (J Clin Pathol 1992;45:964). In one study, H. pylori was found in 75% of patients with giardiasis (J Egypt Soc Parasitol 1996;26:481). Helicobacter produce urease, which breaks down urea to neutralize the acidic pH of the stomach. This produces a comparatively alkaline environment better suited for H. pylori survival. Thus, higher pH may induce a permissive local environment for Giardia and stimulate excystation and subsequent release and survival of trophozoites. Patients treated for ulcers who have recurring upper gastrointestinal tract symptoms should be examined for signs of Giardia (Indian J Pathol Med 2006;49:519).
Diagnosis can be made by simple examination of stool for ova and parasites, searching for teardrop or sickle shaped trophozoites. Treatment consists of a multiday course of antibiotics, such as metronidazole.
Based on the endoscopic findings, a differential diagnosis of H. pylori associated follicular gastritis and maltoma was given in this case. Histopathological examination was used to make the diagnosis.
References: eMedicine: Giardiasis [Accessed 29 April 2024], Koss: Diagnostic Cytology and Its Histopathologic Bases, 5th Edition, 2005
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Suhail Muzaffar and Dr. Bilal Karim Siddiqui, City Hospital, Sandwell & West Birmingham NHS Trust (United Kingdom).

We offer dermatopathology, head and neck and ophthalmic pathology consultations for pathology organizations worldwide. Visit our website or call (617) 549-1168 to find out how we can help your practice to establish, grow and promote your subspecialty outreach program and effectively compete with reference laboratories.
Our services, supported by custom-designed digital pathology-ready workflow solution, range from second opinion consultations on difficult cases to providing daily subspecialty signout and short-term coverage.
Find out how recognized experts in the field can support your practice at a fraction of the cost of hiring a full-time dermatopathologist.
Website news:
(1) We have updated the in situ carcinoma section of the Breast-Malignant chapter, which is now in our new format with thumbnails of most images.
(2) Thanks to the following contributors of images:
(3) Have you visited Detroits new Riverwalk? If you live in the Detroit, Michigan area, sign up for the 5K Run / Walk for the charity we sponsor, The Detroit College Promise. The event is fun for all, even if you are not a runner. It is scheduled for Saturday, October 10, 2009 at 9:00 am, with registration at 8:00 am. You'll have a great time visiting Detroit's new Riverwalk and meeting other people interested in the outdoors and supporting college education.
(4) Be sure to check the special sections on our Jobs page, under Miscellaneous, for Locum Tenens / Part-time jobs, PhD positions, Seeking a Residency or Residency Positions available, Job Advice and an article on Transitioning.
Visit and follow our Blog to see recent updates to the website.
(1) We have updated the in situ carcinoma section of the Breast-Malignant chapter, which is now in our new format with thumbnails of most images.
(2) Thanks to the following contributors of images:
- Dr. Asmaa Gaber Abdou, Menoufiya University, Egypt - Uterus chapter: Dysfunctional Uterine Bleeding
- John Irlam, D.O., University of Toledo Medical Center (Ohio) - Skin-Nonmelanocytic tumors chapter: Cylindroma, Trichilemmoma, Sebaceous Hyperplasia, Eccrine Poroma and Sebaceous Carcinoma; and Skin-Melanocytic tumors chapter: Blue Nevus.
- Ed Uthman, MD., Texas, Cervix chapter - Squamous Cell Carcinoma, Lymphomas: B cell chapter - Burkitts Lymphoma, Oral Cavity chapter - Infectious Mononucleosis and Placenta chapter - Incomplete / Partial Hydatiform mole
(3) Have you visited Detroits new Riverwalk? If you live in the Detroit, Michigan area, sign up for the 5K Run / Walk for the charity we sponsor, The Detroit College Promise. The event is fun for all, even if you are not a runner. It is scheduled for Saturday, October 10, 2009 at 9:00 am, with registration at 8:00 am. You'll have a great time visiting Detroit's new Riverwalk and meeting other people interested in the outdoors and supporting college education.
(4) Be sure to check the special sections on our Jobs page, under Miscellaneous, for Locum Tenens / Part-time jobs, PhD positions, Seeking a Residency or Residency Positions available, Job Advice and an article on Transitioning.
Visit and follow our Blog to see recent updates to the website.
Case #157
Clinical history:
A 20 year old Asian woman presented with dyspepsia. An upper GI endoscopy was followed by a gastric antral biopsy, which revealed a moderate acute and chronic inflammatory infiltrate in the lamina propria. There was no evidence of atrophic gastritis, intestinal metaplasia, dysplasia or malignancy.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Gastric giardiasis
Discussion:
A large number of giardial trophozoites were identified along the surface of foveolar epithelial cells (figure 1). The trophozoites appeared as pear or sickle shaped, lying opposed to the gastric surface and foveolar epithelium (figure 2). No H. pylori organisms were identified.
Giardia lamblia is the most prevalent pathogenic intestinal protozoan and a major contributor to the burden of diarrheal disease worldwide. Giardia can be contracted from contaminated streams or pools, through food or by poor hygienic practices resulting in fecal-oral contact. The trophozoites colonize and reside in the lumen of the small intestine, causing severe diarrhea, vomiting, abdominal cramps and fever. These can lead to anorexia, malaise and fatigue.
In a cohort of 41 cases of gastric giardiasis, it was found that all patients showed moderate to severe chronic atrophic gastritis, with mild to severe activity associated with intestinal metaplasia. Though not seen in this case, concomitant H. pylori infection is common in patients with gastric giardiasis (J Clin Pathol 1992;45:964). In one study, H. pylori was found in 75% of patients with giardiasis (J Egypt Soc Parasitol 1996;26:481). Helicobacter produce urease, which breaks down urea to neutralize the acidic pH of the stomach. This produces a comparatively alkaline environment better suited for H. pylori survival. Thus, higher pH may induce a permissive local environment for Giardia and stimulate excystation and subsequent release and survival of trophozoites. Patients treated for ulcers who have recurring upper gastrointestinal tract symptoms should be examined for signs of Giardia (Indian J Pathol Med 2006;49:519).
Diagnosis can be made by simple examination of stool for ova and parasites, searching for teardrop or sickle shaped trophozoites. Treatment consists of a multiday course of antibiotics, such as metronidazole.
Based on the endoscopic findings, a differential diagnosis of H. pylori associated follicular gastritis and maltoma was given in this case. Histopathological examination was used to make the diagnosis.
References: eMedicine: Giardiasis [Accessed 29 April 2024], Koss: Diagnostic Cytology and Its Histopathologic Bases, 5th Edition, 2005