9 September 2009 - Case #156
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Juan José Segura Fonseca, Laboratorio de Patología Diagnóstica, S.A., San José, Costa Rica.

We offer dermatopathology, head and neck and ophthalmic pathology consultations for pathology organizations worldwide. Visit our website or call (617) 549-1168 to find out how we can help your practice to establish, grow and promote your subspecialty outreach program and effectively compete with reference laboratories. Our services, supported by custom-designed digital pathology-ready workflow solution, range from second opinion consultations on difficult cases to providing daily subspecialty signout and short-term coverage. Find out how recognized experts in the field can support your practice at a fraction of the cost of hiring a full-time dermatopathologist.
Advertisement
Case #156
Clinical history:
A 50 year old man with a history of heavy cigar smoking presented with severe inflammation, marked hyperemia and swelling of the free and attached gingival in the maxillary and mandibular arches. Heavy plaque accumulation was present around the teeth, and the gingiva bled easily when touched. Small biopsies were taken.
Clinical images:
Microscopic images:
What is your diagnosis?
Diagnosis: Plasma cell gingivitis
Immunostains:
Discussion:
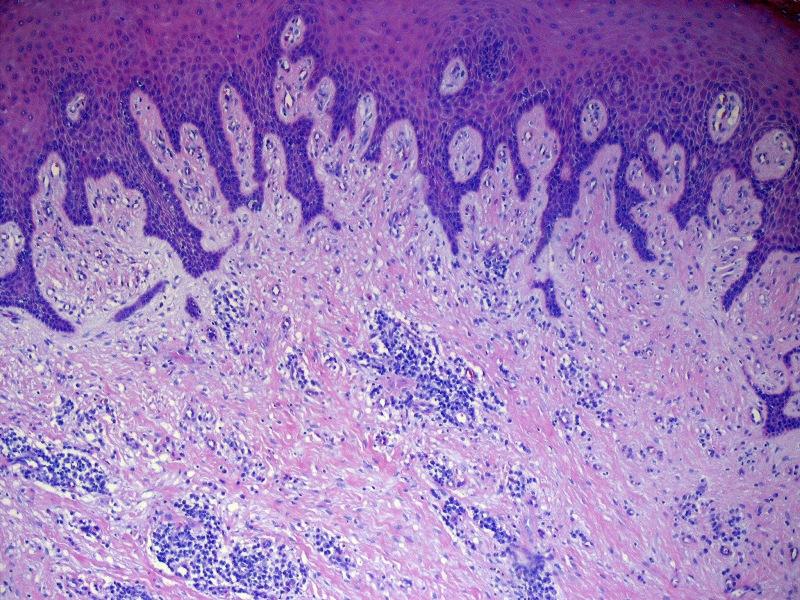
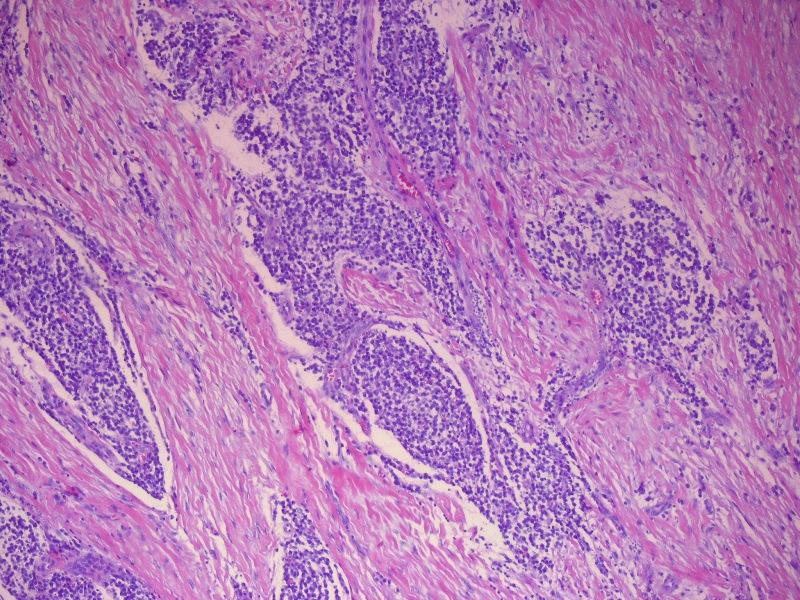
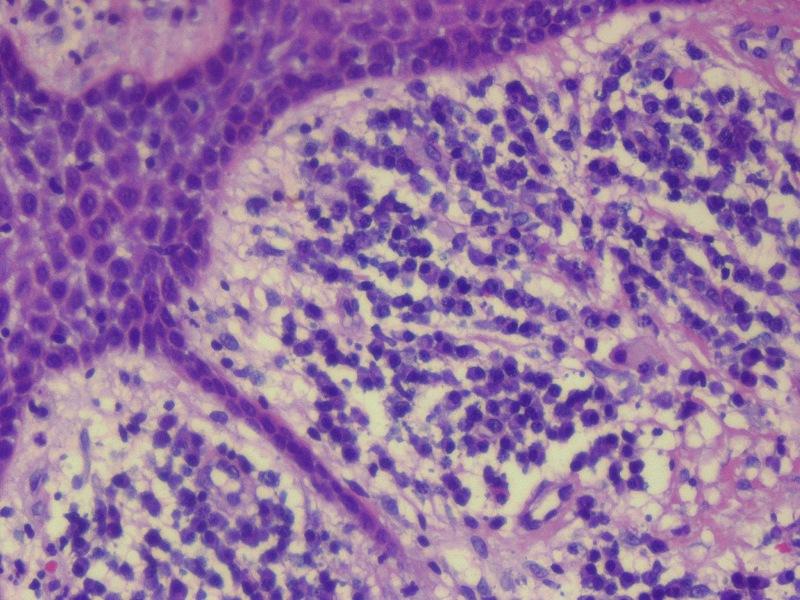
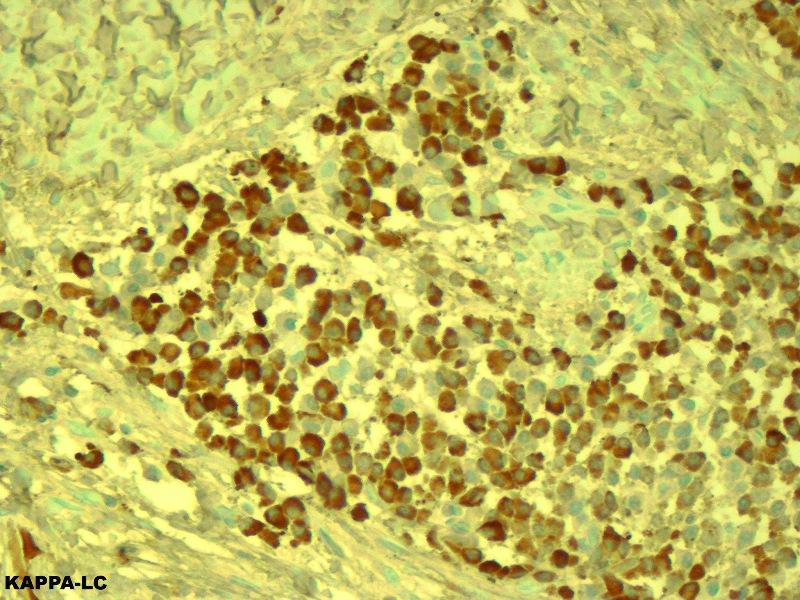
Microscopically, there was a dense infiltration of mature plasma cells beneath the squamous epithelium, separated by thick collagen bundles. A pronounced lichenoid reaction was seen in the overlying squamous epithelium. The plasma cells were polyclonal based on cytoplasmic staining for both kappa and lambda light chains.
Plasma cell gingivitis, first reported in 1960 as plasmocytosis circumorificialis, is a rare inflammatory condition of uncertain etiology (Dtsh Zahnorzd 1960;15:601). It is characterized by a diffuse and intense infiltration of mature plasma cells in the subepithelial gingiva. Causes include an allergic reaction to chewing gum, mint, red chili, black pepper, cardamom, toothpaste (including herbal brands) and khat (Catha edulis, a plant that is chewed in Africa and the Arabian peninsula) (J Periodontol 1971;42:709, Oral Surg Oral Med Oral Pathol 1992;73:690, J Periodontol 1984;55:235, CDS Rev 1995;88:22, Br Dent J 1990;168:115, J Contempt Dent Pract 2007;8:60, Br Dent J 2002;192:311). Though plasma cell gingivitis seems to be a well established entity, its classification as a distinct condition has recently been questioned (SADJ 2008;63:394).
The clinical differential diagnosis includes more serious conditions that affect the gingiva, such as leukemic infiltrates, multiple myeloma, solitary plasmacytoma (forms a mass, clonal) and Waldenström macroglobulinemia. Chronic hyperplastic gingivitis usually has thick collagen fibers and granulation tissue and lacks an intense plasma cell infiltrate. Dermatologic diseases that involve the gingiva include discoid lupus erythematosus, lichen planus and pemphigus.
Treatment includes removal of the offending substance.
This case was also reviewed by an oral and maxillofacial pathologist, who noted that for his specialty (certified by the American Board of Oral and Maxillofacial Pathology), this case represents nonspecific gingival inflammatory hyperplasia, although the possibility that there could be a drug related component (phenytoin, Ca channel blocker, cyclosporin) would also be a consideration. Clinically, the gingival tissues would be much more erythematous in plasma cell gingivitis than in the present case, and the plasma cell infiltrate would be much more diffuse, essentially mimicking extramedullary plasmacytoma.
References: Cutis 2002;69:41
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Juan José Segura Fonseca, Laboratorio de Patología Diagnóstica, S.A., San José, Costa Rica.

We offer dermatopathology, head and neck and ophthalmic pathology consultations for pathology organizations worldwide. Visit our website or call (617) 549-1168 to find out how we can help your practice to establish, grow and promote your subspecialty outreach program and effectively compete with reference laboratories. Our services, supported by custom-designed digital pathology-ready workflow solution, range from second opinion consultations on difficult cases to providing daily subspecialty signout and short-term coverage. Find out how recognized experts in the field can support your practice at a fraction of the cost of hiring a full-time dermatopathologist.
Website news:
(1) We have updated the in situ carcinoma section of the Breast-Malignant chapter, which is now in our new format with thumbnails of most images.
(2) Thanks to the following contributors of images:
(3) If you live in the Detroit, Michigan area, sign up for the first annual 5K Run / Walk for our charity, The Detroit College Promise. The run is scheduled for Saturday, October 10, 2009 at 9:00 am, with registration at 8:00 am. You'll have a great time visiting Detroit's new Riverwalk and meeting other people interested in running, education and supporting the city.
Visit and follow our Blog to see recent updates to the website.
(1) We have updated the in situ carcinoma section of the Breast-Malignant chapter, which is now in our new format with thumbnails of most images.
(2) Thanks to the following contributors of images:
- Dr. Asmaa Gaber Abdou, Menoufiya University, Egypt - Uterus chapter: Dysfunctional Uterine Bleeding
- John Irlam, D.O., University of Toledo Medical Center (Ohio) - Skin-Nonmelanocytic tumors chapter: Cylindroma, Trichilemmoma, Sebaceous Hyperplasia, Eccrine Poroma and Sebaceous Carcinoma; and Skin-Melanocytic tumors chapter: Blue Nevus.
- Ed Uthman, MD., Texas, Cervix chapter - Squamous Cell Carcinoma, Lymphomas: B cell chapter - Burkitt Lymphoma, Oral Cavity chapter - Infectious Mononucleosis and Placenta chapter - Incomplete / Partial Hydatiform mole
(3) If you live in the Detroit, Michigan area, sign up for the first annual 5K Run / Walk for our charity, The Detroit College Promise. The run is scheduled for Saturday, October 10, 2009 at 9:00 am, with registration at 8:00 am. You'll have a great time visiting Detroit's new Riverwalk and meeting other people interested in running, education and supporting the city.
Visit and follow our Blog to see recent updates to the website.
Case #156
Clinical history:
A 50 year old man with a history of heavy cigar smoking presented with severe inflammation, marked hyperemia and swelling of the free and attached gingival in the maxillary and mandibular arches. Heavy plaque accumulation was present around the teeth, and the gingiva bled easily when touched. Small biopsies were taken.
Clinical images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Plasma cell gingivitis
Immunostains:
Discussion:
Microscopically, there was a dense infiltration of mature plasma cells beneath the squamous epithelium, separated by thick collagen bundles. A pronounced lichenoid reaction was seen in the overlying squamous epithelium. The plasma cells were polyclonal based on cytoplasmic staining for both kappa and lambda light chains.
Plasma cell gingivitis, first reported in 1960 as plasmocytosis circumorificialis, is a rare inflammatory condition of uncertain etiology (Dtsh Zahnorzd 1960;15:601). It is characterized by a diffuse and intense infiltration of mature plasma cells in the subepithelial gingiva. Causes include an allergic reaction to chewing gum, mint, red chili, black pepper, cardamom, toothpaste (including herbal brands) and khat (Catha edulis, a plant that is chewed in Africa and the Arabian peninsula) (J Periodontol 1971;42:709, Oral Surg Oral Med Oral Pathol 1992;73:690, J Periodontol 1984;55:235, CDS Rev 1995;88:22, Br Dent J 1990;168:115, J Contempt Dent Pract 2007;8:60, Br Dent J 2002;192:311). Though plasma cell gingivitis seems to be a well established entity, its classification as a distinct condition has recently been questioned (SADJ 2008;63:394).
The clinical differential diagnosis includes more serious conditions that affect the gingiva, such as leukemic infiltrates, multiple myeloma, solitary plasmacytoma (forms a mass, clonal) and Waldenström macroglobulinemia. Chronic hyperplastic gingivitis usually has thick collagen fibers and granulation tissue and lacks an intense plasma cell infiltrate. Dermatologic diseases that involve the gingiva include discoid lupus erythematosus, lichen planus and pemphigus.
Treatment includes removal of the offending substance.
This case was also reviewed by an oral and maxillofacial pathologist, who noted that for his specialty (certified by the American Board of Oral and Maxillofacial Pathology), this case represents nonspecific gingival inflammatory hyperplasia, although the possibility that there could be a drug related component (phenytoin, Ca channel blocker, cyclosporin) would also be a consideration. Clinically, the gingival tissues would be much more erythematous in plasma cell gingivitis than in the present case, and the plasma cell infiltrate would be much more diffuse, essentially mimicking extramedullary plasmacytoma.
References: Cutis 2002;69:41