6 August 2009 - Case #154
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Renuka Agrawal, Loma Linda University Medical Center, California (USA).
Case #154
Clinical history:
An 81 year old woman presented with epigastric pain caused by pancreatitis. CT scan showed a cystic papillary tumor in the head of the pancreas and a dilated pancreatic duct. The duodenum, pancreas and spleen were resected.
Gross image:
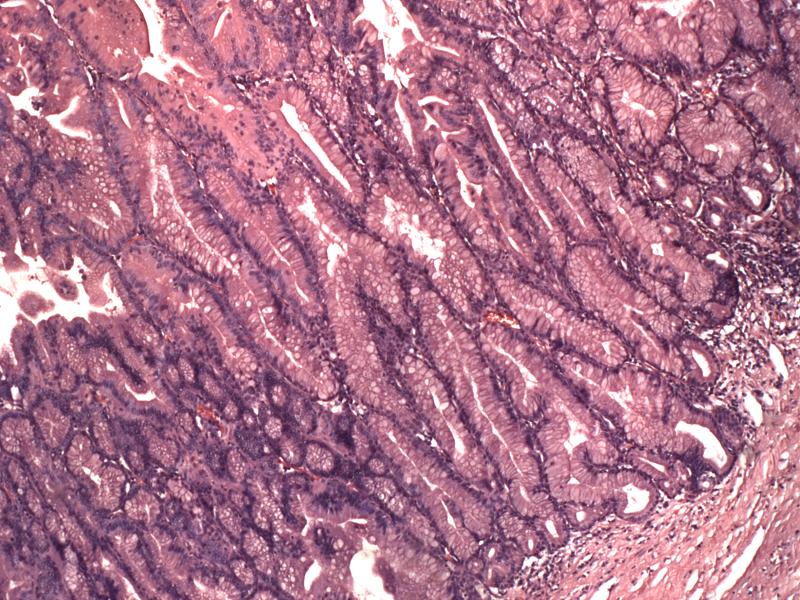
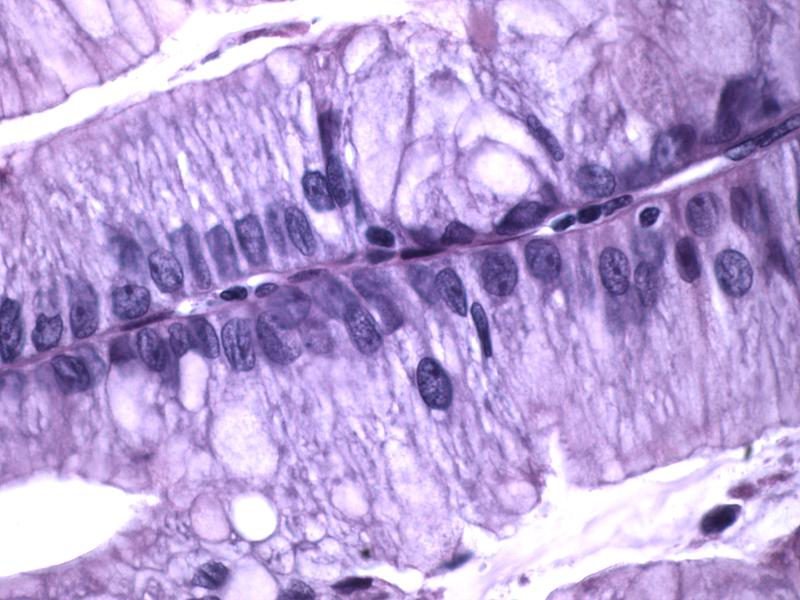
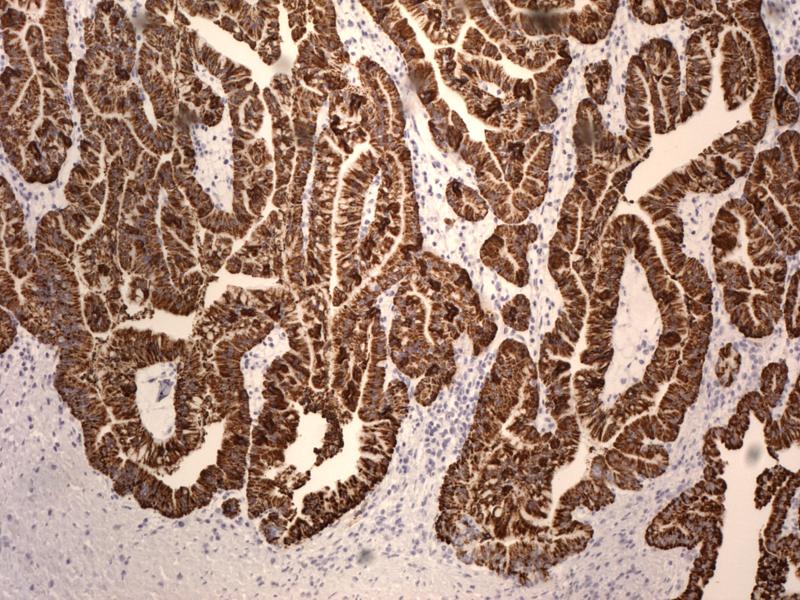
Microscopic images:
What is your diagnosis?
Diagnosis: Intraductal papillary mucinous neoplasm (IPMN), intestinal type
Discussion:
Intraductal papillary mucinous neoplasms (IPMNs) are cystic, mucin producing neoplasms of the pancreas. They are grossly visible, papillary epithelial neoplasms which arise from the main pancreatic duct or branch ducts, with mucin extrusion from the ampulla and varying degrees of duct dilation. They display complex papillary fronds of mucin producing epithelial cells and are associated with chronic pancreatitis. There is no ovarian type stroma.
IPMNs are more common in men over age 60. They typically occur in the head of the pancreas.
4 histologic subtypes are recognized: gastric, intestinal, pancreaticobiliary and oncocytic. They also have a spectrum of atypia ranging from adenoma to invasive cancer (Virchows 2005;447:794). The biological behavior of invasive cancers arising from IPMNs is better than that of de novo pancreatic adenocarcinoma. The surgical pathology report on IPMNs should indicate whether the main or branch ducts are involved, the presence and extent of invasion and margin status.
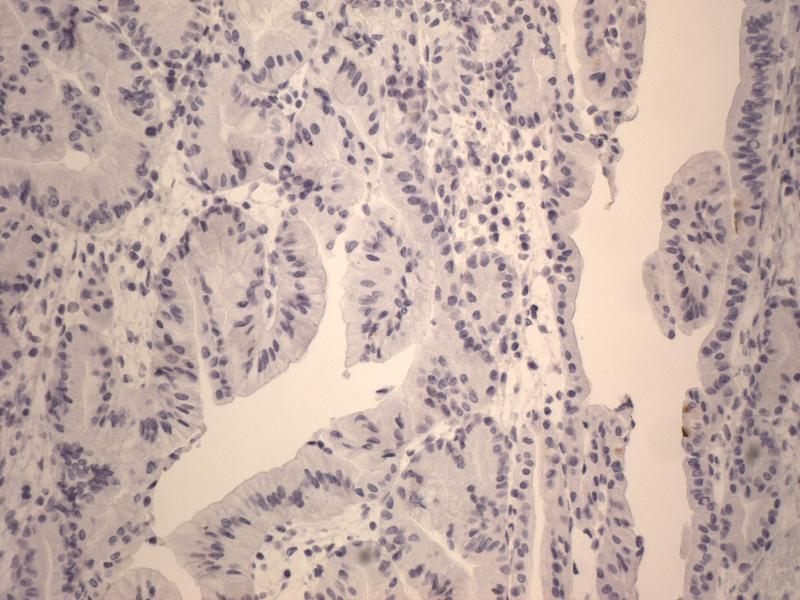
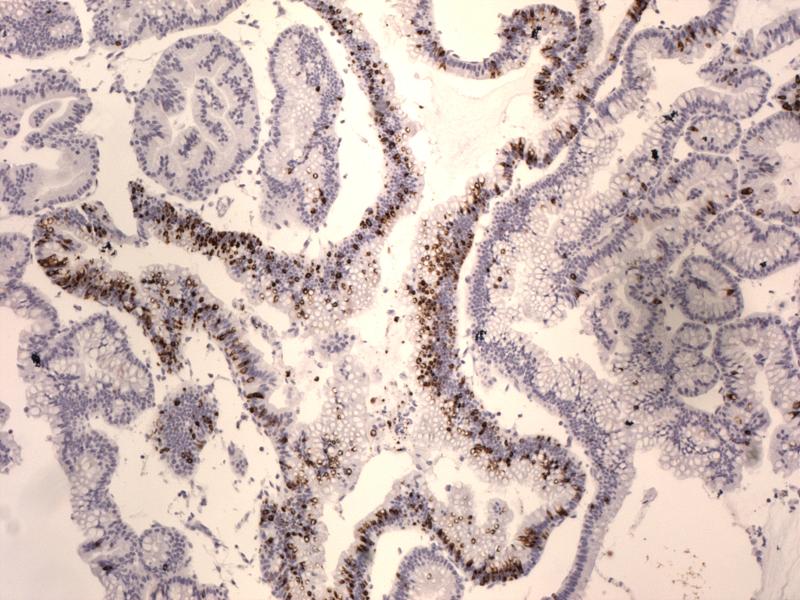
A MUC1 / MUC2 expression profile may be helpful (Mod Pathol 2002;15:1087). MUC1 is an indicator of aggressive pancreatic neoplasms, while MUC2 is a marker of indolent phenotypes (J Clin Pathol 2004;57:456). In intestinal IPMN, MUC2 and MUC5AC are positive and MUC1 is negative. This subtype usually involves the main pancreatic duct, has a more favorable prognosis, and is not associated with ductal carcinoma (Am J Surg Pathol 2006;30:1561, Am J Surg Pathol 2001;25:942). However, intestinal type IPMN can be invasive and at these times, is associated with colloid carcinoma (Am J Surg Pathol 2004;28:839). Prognosis can be unpredictable and depends on the severity of invasion.
Resection is adequate treatment for adenomas, which do not recur (Ann Surg Oncol 2006;13:582). Invasive tumors may be lethal and require chemotherapy or radiation (Int J Radiat Oncol Biol Phys 2010;76:839, Ann Surg Oncol 2007;14:3174). Minimally invasive tumors have similar survival rates as noninvasive tumors (Am J Surg Pathol 2008;32:243).
The differential diagnosis includes:
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Renuka Agrawal, Loma Linda University Medical Center, California (USA).
Website news:
(1) We now have a PathologyOutlines group on Flickr. If you have a Flickr account, you can upload directly to our Flickr group at http://www.flickr.com/groups/pathologyoutlines/. We will post your name as the contributor (unless you want to be anonymous) and a link to the pictures in the appropriate chapter of our online textbook, so pathologists and related personnel around the world can benefit from them.
(2) We have updated the Skeletal Muscle section of our Soft Tissue Tumors - Part 3 chapter.
Visit and follow our Blog to see recent updates to the website.
(1) We now have a PathologyOutlines group on Flickr. If you have a Flickr account, you can upload directly to our Flickr group at http://www.flickr.com/groups/pathologyoutlines/. We will post your name as the contributor (unless you want to be anonymous) and a link to the pictures in the appropriate chapter of our online textbook, so pathologists and related personnel around the world can benefit from them.
(2) We have updated the Skeletal Muscle section of our Soft Tissue Tumors - Part 3 chapter.
Visit and follow our Blog to see recent updates to the website.
Case #154
Clinical history:
An 81 year old woman presented with epigastric pain caused by pancreatitis. CT scan showed a cystic papillary tumor in the head of the pancreas and a dilated pancreatic duct. The duodenum, pancreas and spleen were resected.
Gross image:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Intraductal papillary mucinous neoplasm (IPMN), intestinal type
Discussion:
Intraductal papillary mucinous neoplasms (IPMNs) are cystic, mucin producing neoplasms of the pancreas. They are grossly visible, papillary epithelial neoplasms which arise from the main pancreatic duct or branch ducts, with mucin extrusion from the ampulla and varying degrees of duct dilation. They display complex papillary fronds of mucin producing epithelial cells and are associated with chronic pancreatitis. There is no ovarian type stroma.
IPMNs are more common in men over age 60. They typically occur in the head of the pancreas.
4 histologic subtypes are recognized: gastric, intestinal, pancreaticobiliary and oncocytic. They also have a spectrum of atypia ranging from adenoma to invasive cancer (Virchows 2005;447:794). The biological behavior of invasive cancers arising from IPMNs is better than that of de novo pancreatic adenocarcinoma. The surgical pathology report on IPMNs should indicate whether the main or branch ducts are involved, the presence and extent of invasion and margin status.
A MUC1 / MUC2 expression profile may be helpful (Mod Pathol 2002;15:1087). MUC1 is an indicator of aggressive pancreatic neoplasms, while MUC2 is a marker of indolent phenotypes (J Clin Pathol 2004;57:456). In intestinal IPMN, MUC2 and MUC5AC are positive and MUC1 is negative. This subtype usually involves the main pancreatic duct, has a more favorable prognosis, and is not associated with ductal carcinoma (Am J Surg Pathol 2006;30:1561, Am J Surg Pathol 2001;25:942). However, intestinal type IPMN can be invasive and at these times, is associated with colloid carcinoma (Am J Surg Pathol 2004;28:839). Prognosis can be unpredictable and depends on the severity of invasion.
Resection is adequate treatment for adenomas, which do not recur (Ann Surg Oncol 2006;13:582). Invasive tumors may be lethal and require chemotherapy or radiation (Int J Radiat Oncol Biol Phys 2010;76:839, Ann Surg Oncol 2007;14:3174). Minimally invasive tumors have similar survival rates as noninvasive tumors (Am J Surg Pathol 2008;32:243).
The differential diagnosis includes:
- Pancreatic intra-epithelial neoplasms (PanIN): a microscopic rather than a gross lesion
- Mucinous cystic neoplasms (MCN): more prevalent among women, not in ducts, have ovarian type stroma (Pancreatology 2006;6:17)
- Intraductal tubulopapillary neoplasm: newly described, no / minimal visible or microscopic mucin (Am J Surg Pathol 2009;33:1164)