3 June 2009 - Case #148
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Moneil Patel, Chief Resident of Pathology, NYMC St. Vincent's Hospital, New York, New York (USA).

PathLab Coding Solutions SM is designed to assist in minimizing risks associated with over-coding and lack of documentation while maximizing reimbursement through proper coding practices.
Subscribers will be able to resolve simple to complex coding issues and remain up-to-date with changes in coding procedures by utilizing the Automated Coding Assistant, Resource Center and Coding Consultant Dashboard.
To learn more about PathLab Coding Solutions, visit www.PathLabCoding.com or contact Leigh Polk with PSA at 800-832-5270 ext 2941.
Advertisement
Case #148
Clinical history:
A 59 year old man presented with a left testicular mass which had been growing slowly for a year. He had a history of a left testicular hydrocelectomy in 2005. His serum AFP levels were normal and an orchiectomy was performed.
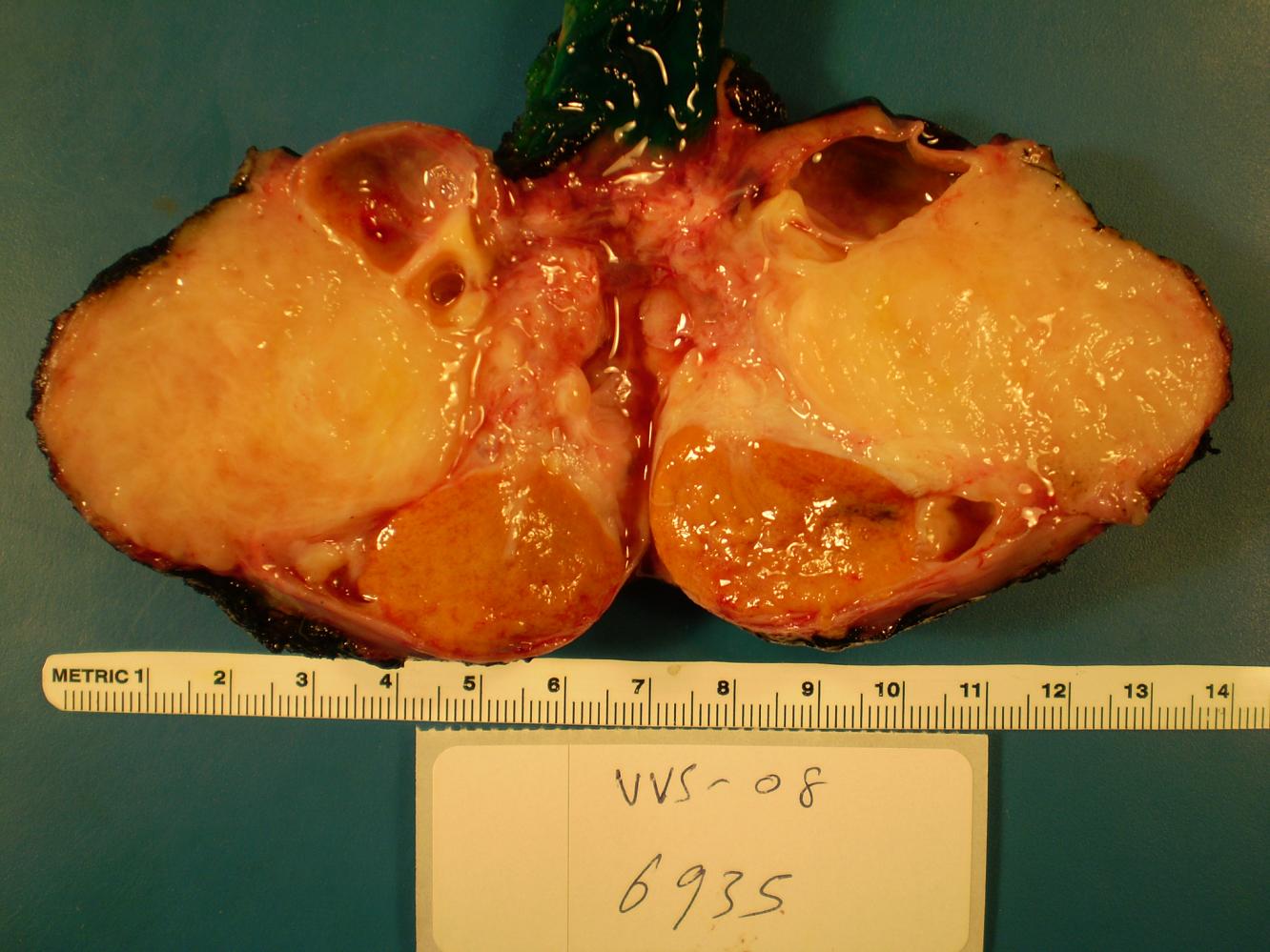
Sectioning revealed a 4.8 x 4.6 x 3.6 cm yellow, partially cystic firm mass pushing the testicular parenchyma to the edge. The mass was firmly attached to the tunica vaginalis.
Gross images:
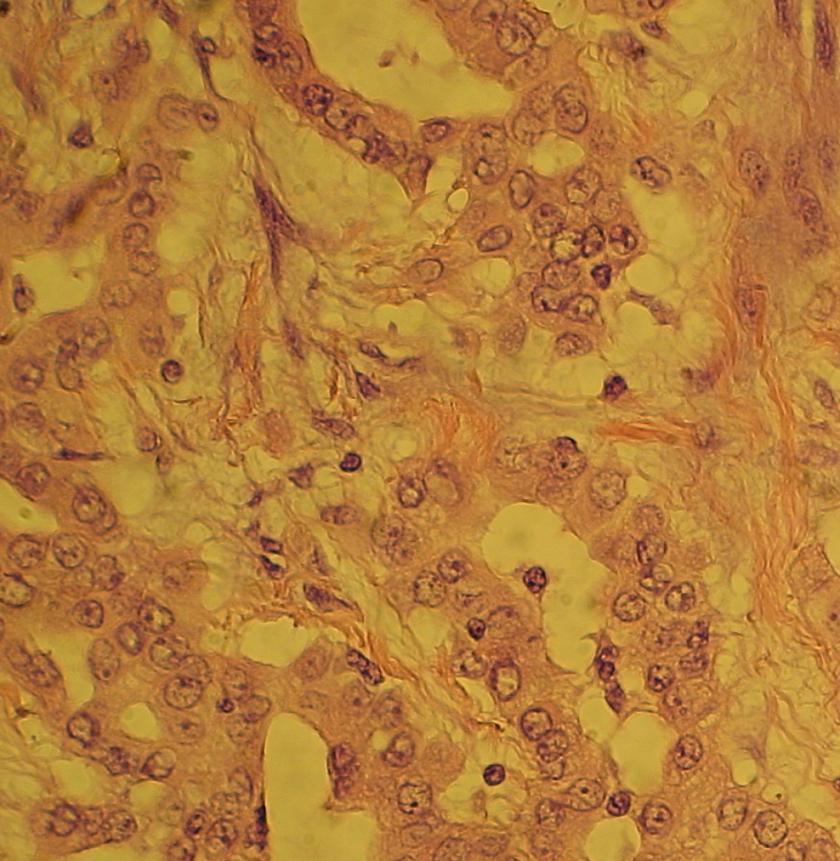
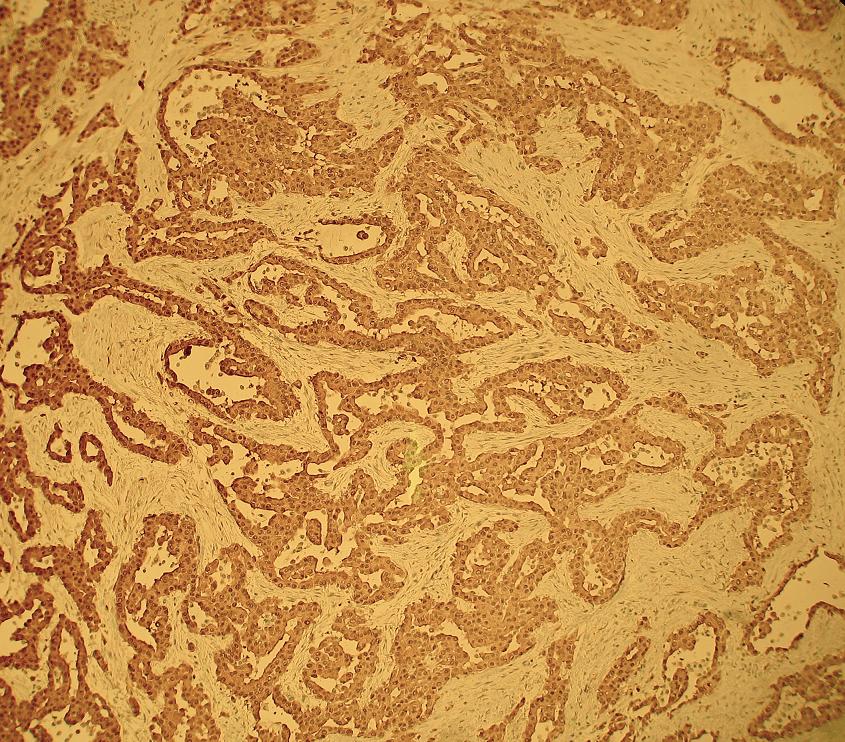
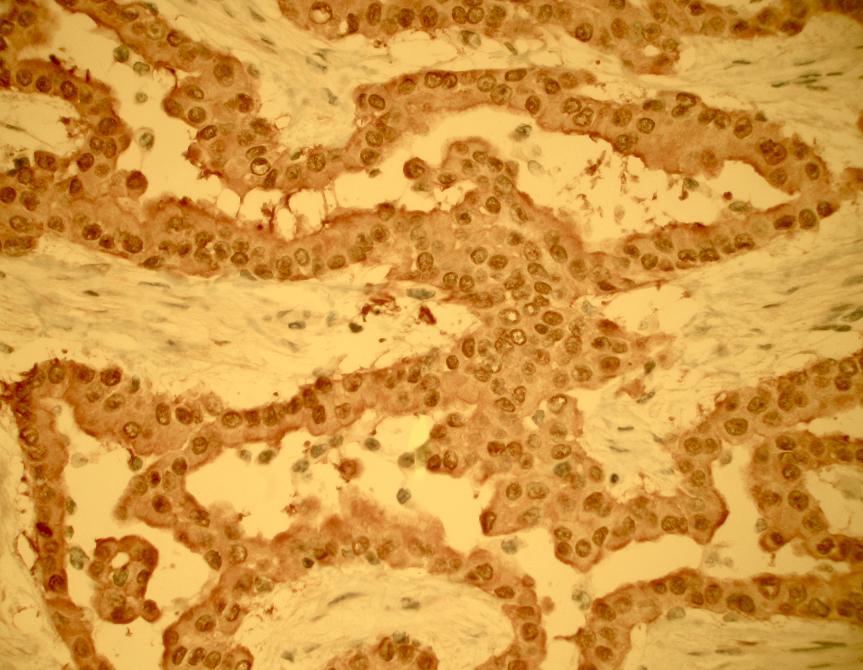
Microscopic images:
What is your diagnosis?
Diagnosis: Malignant mesothelioma of the tunica vaginalis
Discussion:
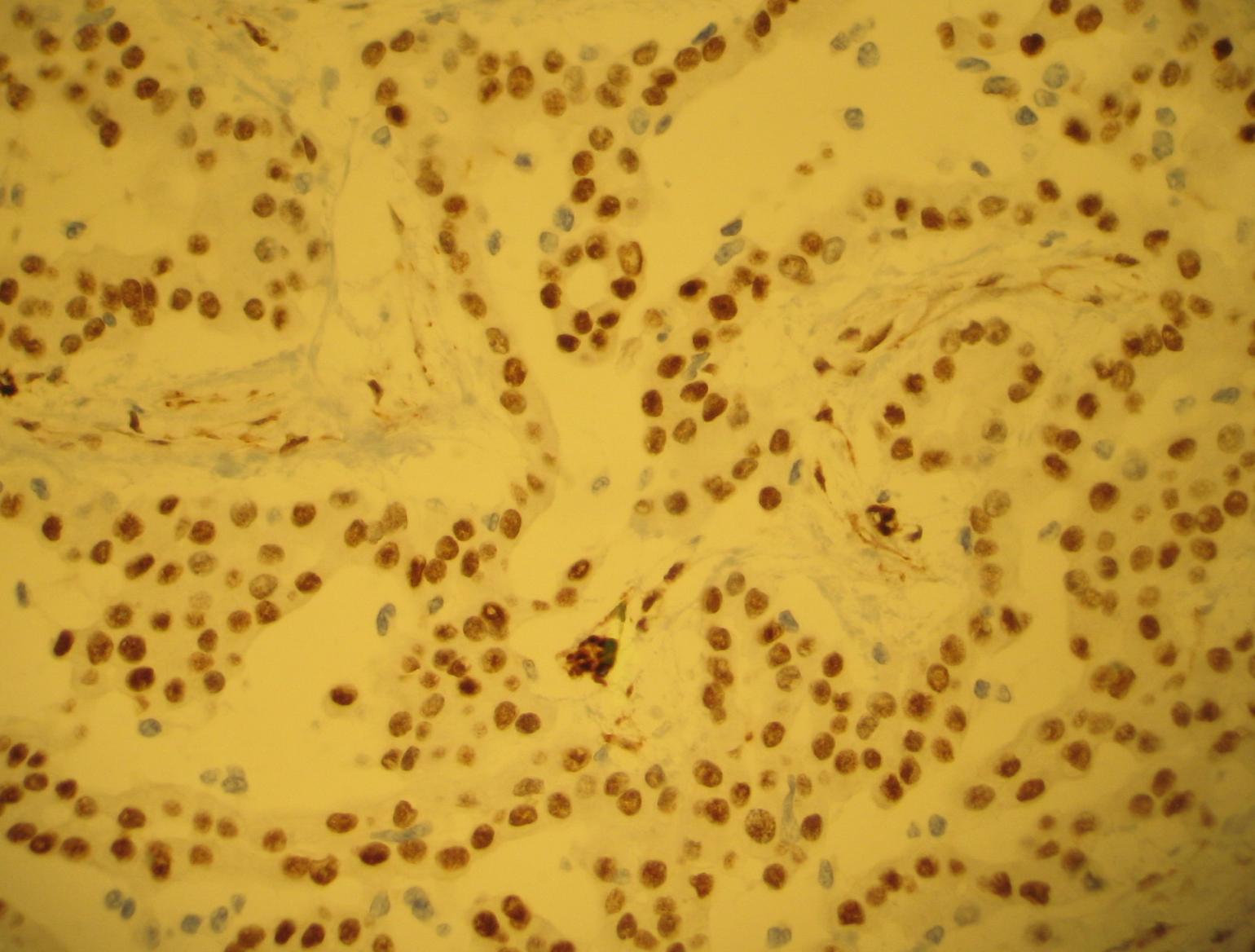
The tumor had an invasive, tubulopapillary pattern, with a single layer of atypical, epithelioid type mesothelium overlying a fibrovascular core. No sarcomatoid features were identified. Tumor cells were immunoreactive for calretinin and WT1 (nuclear staining) and negative for BerEP4, MOC31, CEA, desmin and AFP. This is consistent with the staining pattern for malignant mesotheliomas in the testis (calretinin+, EMA+, thrombomodulin+, CK7+, CK5/6 variable, CK20-, CEA-) (Am J Surg Pathol 2006;30:1).
Mesotheliomas are neoplasms of the lining of the body's serous cavities, usually involving the pleura, but occasionally the peritoneum or pericardium (eMedicine: Mesothelioma [Accessed 30 April 2024]). In the testis, the tunica vaginalis derives from evagination of peritoneum into the scrotum. Mesotheliomas at this site are rare, with a wide age range (Am J Surg Pathol 1995;19:815). Most cases are associated with asbestos exposure, although some cases, including the present one, have no history of asbestos exposure (Orphanet J Rare Dis 2008 Dec 19;3:34, Cases J 2008 Nov 14;1:310). Of note, mesotheliomas often present with a hydrocele, as in this case.
The differential diagnosis includes:
Malignant mesothelioma of the tunica vaginalis is often fatal. Treatment includes radical orchiectomy and possibly retroperitoneal lymph node dissection. Even patients with negative resection margins frequently die of disease. In a recent study of 5 patients, mean disease specific survival was only 29 months and 3 patients developed inguinal nodal metastases (Urology 2005;66:397).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Moneil Patel, Chief Resident of Pathology, NYMC St. Vincent's Hospital, New York, New York (USA).

PathLab Coding Solutions SM is designed to assist in minimizing risks associated with over-coding and lack of documentation while maximizing reimbursement through proper coding practices.
Subscribers will be able to resolve simple to complex coding issues and remain up-to-date with changes in coding procedures by utilizing the Automated Coding Assistant, Resource Center and Coding Consultant Dashboard.
To learn more about PathLab Coding Solutions, visit www.PathLabCoding.com or contact Leigh Polk with PSA at 800-832-5270 ext 2941.
Website news:
(1) We have reformatted the Home Page to reduce the amount of scrolling necessary. We have also changed the Jobs and Conferences pages so that they load faster. Let us know if you have other suggestions to make our website easier to use.
(2) We have split the Soft Tissue chapter into three chapters, and updated Part 1, which discusses Introduction, Infections & Fibroblastic / myofibroblastic tumors (click here). New features to be incorporated into all updated chapters include an additional table of contents sorted alphabetically, new formatting and more discussion of differential diagnoses.
(3) Thanks to Angel Fernandez-Flores, MD, PhD, Hospital El Bierzo and Clinica Ponferrada, Spain, for contributing images of botryomycosis to the Skin-nontumor chapter and acquired digital fibrokeratoma to the Skin-nonmelanocytic tumor chapter.
Visit and follow our Blog to see recent updates to the website.
(1) We have reformatted the Home Page to reduce the amount of scrolling necessary. We have also changed the Jobs and Conferences pages so that they load faster. Let us know if you have other suggestions to make our website easier to use.
(2) We have split the Soft Tissue chapter into three chapters, and updated Part 1, which discusses Introduction, Infections & Fibroblastic / myofibroblastic tumors (click here). New features to be incorporated into all updated chapters include an additional table of contents sorted alphabetically, new formatting and more discussion of differential diagnoses.
(3) Thanks to Angel Fernandez-Flores, MD, PhD, Hospital El Bierzo and Clinica Ponferrada, Spain, for contributing images of botryomycosis to the Skin-nontumor chapter and acquired digital fibrokeratoma to the Skin-nonmelanocytic tumor chapter.
Visit and follow our Blog to see recent updates to the website.
Case #148
Clinical history:
A 59 year old man presented with a left testicular mass which had been growing slowly for a year. He had a history of a left testicular hydrocelectomy in 2005. His serum AFP levels were normal and an orchiectomy was performed.
Sectioning revealed a 4.8 x 4.6 x 3.6 cm yellow, partially cystic firm mass pushing the testicular parenchyma to the edge. The mass was firmly attached to the tunica vaginalis.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Malignant mesothelioma of the tunica vaginalis
Discussion:
The tumor had an invasive, tubulopapillary pattern, with a single layer of atypical, epithelioid type mesothelium overlying a fibrovascular core. No sarcomatoid features were identified. Tumor cells were immunoreactive for calretinin and WT1 (nuclear staining) and negative for BerEP4, MOC31, CEA, desmin and AFP. This is consistent with the staining pattern for malignant mesotheliomas in the testis (calretinin+, EMA+, thrombomodulin+, CK7+, CK5/6 variable, CK20-, CEA-) (Am J Surg Pathol 2006;30:1).
Mesotheliomas are neoplasms of the lining of the body's serous cavities, usually involving the pleura, but occasionally the peritoneum or pericardium (eMedicine: Mesothelioma [Accessed 30 April 2024]). In the testis, the tunica vaginalis derives from evagination of peritoneum into the scrotum. Mesotheliomas at this site are rare, with a wide age range (Am J Surg Pathol 1995;19:815). Most cases are associated with asbestos exposure, although some cases, including the present one, have no history of asbestos exposure (Orphanet J Rare Dis 2008 Dec 19;3:34, Cases J 2008 Nov 14;1:310). Of note, mesotheliomas often present with a hydrocele, as in this case.
The differential diagnosis includes:
- Adenocarcinoma: more common in the epididymis than the tunica vaginalis, has back to back glands or a poorly differentiated pattern, often necrosis and mitotic figures, CK20+, BerEP4+, CEA+, calretinin-, thrombomodulin-, no long thin microvilli on EM
- Well differentiated papillary mesothelioma: very rare, papillary but not tubular, papillae are lined by cuboidal cells with a complex branching pattern but no atypia and no invasion; stroma has lymphoplasmacytic infiltrate
- Mesothelial hyperplasia: no mass, no complex arborizing papillae, not invasive
Malignant mesothelioma of the tunica vaginalis is often fatal. Treatment includes radical orchiectomy and possibly retroperitoneal lymph node dissection. Even patients with negative resection margins frequently die of disease. In a recent study of 5 patients, mean disease specific survival was only 29 months and 3 patients developed inguinal nodal metastases (Urology 2005;66:397).