7 May 2009 - Case #145
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Debra L. Zynger, MD and Jeffrey A. McDavit, MD, University of Pittsburgh Medical Center, Pittsburgh, PA (USA).
Case #145
Clinical history:
A 15 year old boy presented with a paratesticular mass.
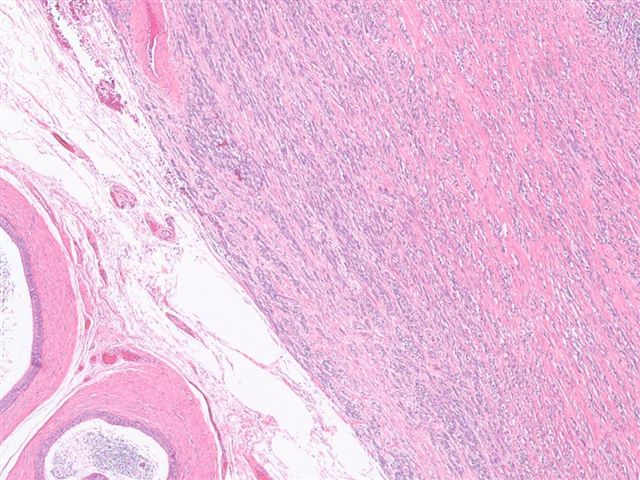
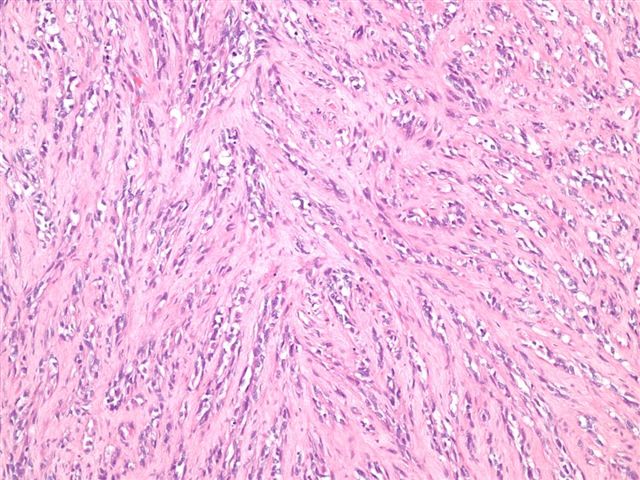
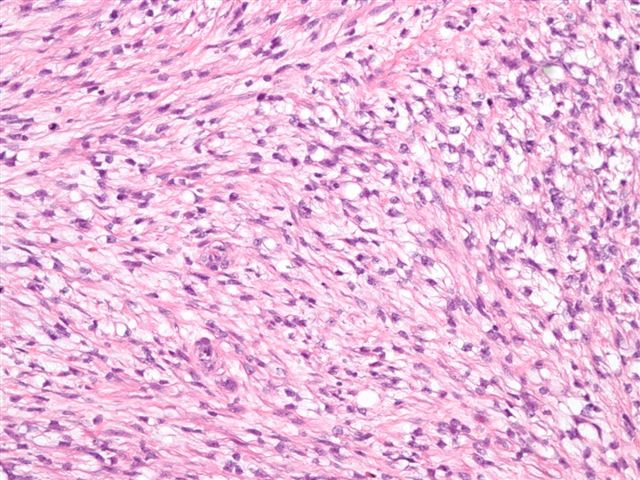
Microscopic images:
What is your diagnosis?
Diagnosis: Spindle cell embryonal rhabdomyosarcoma
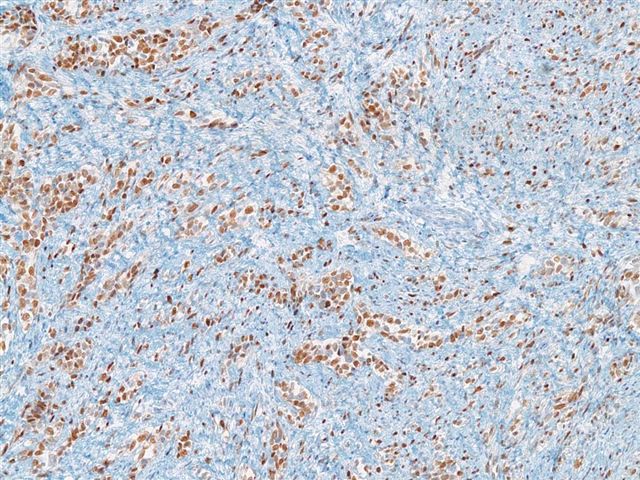
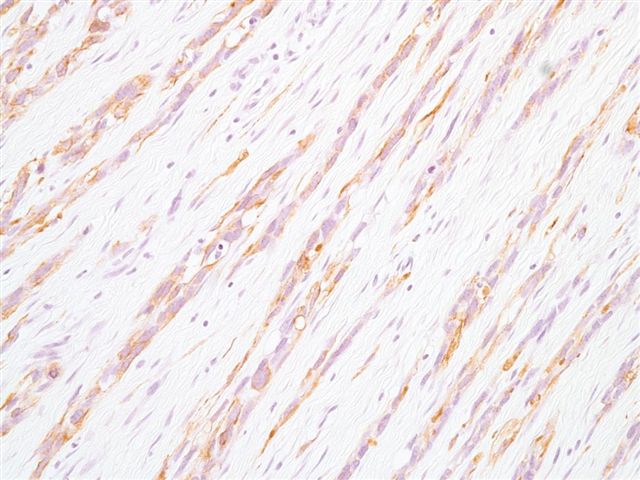
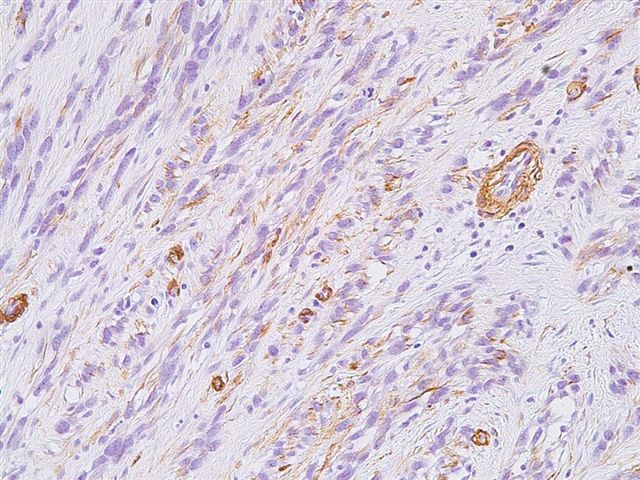
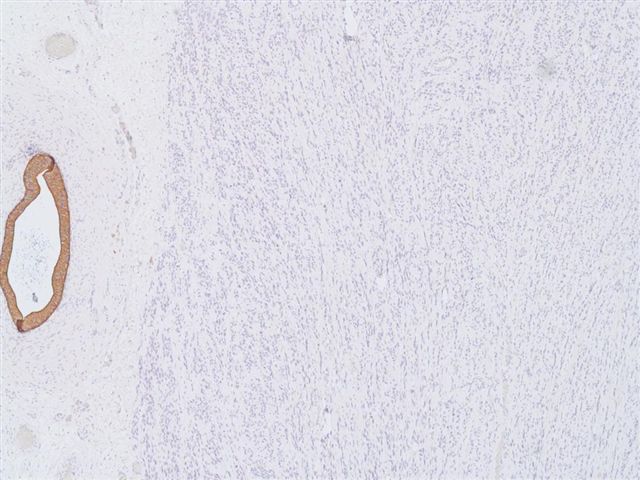
Immunostains:
Discussion:
Rhabdomyosarcomas are classified into embryonal, alveolar and pleomorphic types. Embryonal rhabdomyosarcoma can be further classified as spindle cell or botryoid subtypes.
Spindle cell rhabdomyosarcoma, first described in 1992, is most commonly found in the paratesticular region of young boys, although cases have also been described in adults (Am J Surg Pathol 1992;16:229, Am J Surg Pathol 2005:29:1106, Virchows Arch 2006;449:554). Grossly, the tumors are firm and fibrous, with a whorled cut surface resembling leiomyoma. Fine needle aspiration reveals numerous spindle cells and large fragments of cytoplasmic processes with cross striations (Acta Cytol 2005;49:331). At excision, they are composed of a uniform proliferation of relatively bland, elongated spindle cells (at least 50% of tumor cells) with eosinophilic and fibrillar cytoplasm mimicking smooth muscle fibers. Nuclei are often elongated and vesicular. Scattered spindled or polygonal rhabdomyoblasts with brightly eosinophilic cytoplasm and pleomorphic nuclei are also present.
Stains for desmin, myogenin, vimentin, myoD1 and smooth muscle actin are positive (Arch Pathol Lab Med 2006;130:1454). The tumor cells are negative for S100, keratin and caldesmon.
The differential diagnosis includes:
Excision typically results in a good prognosis in children but tumors in adults have a more aggressive course.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Debra L. Zynger, MD and Jeffrey A. McDavit, MD, University of Pittsburgh Medical Center, Pittsburgh, PA (USA).
Website news:
(1) We added a new article to our Management Page - Coding Prostate Saturation Biopsies, by Laura Edgeworth, PSA, LLC.
(2) We added a new article to our Management Page - Billing Contracts verses Managed Care Contracts, by Mick Raich, Vachette Pathology.
(3) Do you have good examples of Ovarian-nontumor pathology? Help your fellow pathologists worldwide by contributing these images to PathologyOutlines.com, where they will be viewed on a regular basis.
Visit and follow our Blog to see recent updates to the website.
(1) We added a new article to our Management Page - Coding Prostate Saturation Biopsies, by Laura Edgeworth, PSA, LLC.
(2) We added a new article to our Management Page - Billing Contracts verses Managed Care Contracts, by Mick Raich, Vachette Pathology.
(3) Do you have good examples of Ovarian-nontumor pathology? Help your fellow pathologists worldwide by contributing these images to PathologyOutlines.com, where they will be viewed on a regular basis.
Visit and follow our Blog to see recent updates to the website.
Case #145
Clinical history:
A 15 year old boy presented with a paratesticular mass.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Spindle cell embryonal rhabdomyosarcoma
Immunostains:
Discussion:
Rhabdomyosarcomas are classified into embryonal, alveolar and pleomorphic types. Embryonal rhabdomyosarcoma can be further classified as spindle cell or botryoid subtypes.
Spindle cell rhabdomyosarcoma, first described in 1992, is most commonly found in the paratesticular region of young boys, although cases have also been described in adults (Am J Surg Pathol 1992;16:229, Am J Surg Pathol 2005:29:1106, Virchows Arch 2006;449:554). Grossly, the tumors are firm and fibrous, with a whorled cut surface resembling leiomyoma. Fine needle aspiration reveals numerous spindle cells and large fragments of cytoplasmic processes with cross striations (Acta Cytol 2005;49:331). At excision, they are composed of a uniform proliferation of relatively bland, elongated spindle cells (at least 50% of tumor cells) with eosinophilic and fibrillar cytoplasm mimicking smooth muscle fibers. Nuclei are often elongated and vesicular. Scattered spindled or polygonal rhabdomyoblasts with brightly eosinophilic cytoplasm and pleomorphic nuclei are also present.
Stains for desmin, myogenin, vimentin, myoD1 and smooth muscle actin are positive (Arch Pathol Lab Med 2006;130:1454). The tumor cells are negative for S100, keratin and caldesmon.
The differential diagnosis includes:
- Fibrosarcoma: herringbone pattern, may have similar morphology but no rhabdomyoblasts, negative for skeletal muscle markers
- Infantile fibromatosis: deep location, fascicles of spindle cells, no cross striations, no undifferentiated cells
- Leiomyosarcoma: usually high grade, cigar shaped nuclei, no rhabdomyoblasts, often positive for caldesmon, negative for myoglobin
- Neuromuscular hamartoma of soft tissue: usually age < 2 years, affects brachial plexus or sciatic nerve, multinodular growth with connective tissue separating nodules, no rhabdomyoblasts, muscular component is positive for desmin and muscle specific actin, neural component is positive for S100
- Rhabdomyoma: benign tumor of skeletal muscle differentiation, no rhabdomyoblasts, no pleomorphism, no necrosis
Excision typically results in a good prognosis in children but tumors in adults have a more aggressive course.