16 April 2009 - Case #143
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. David Cohen, Herzliya Medical Center, Israel.
Case #143
Clinical history:
A 37 year old woman with no significant medical history was admitted for abdominal pain. Physical exam revealed a large mobile upper abdominal mass. Laboratory results as well as tumor markers were all within the normal range.
A laparotomy revealed a 20 x 15 cm, upper abdominal, highly vascularized and necrotic mass, that appeared to originate from the head of the pancreas. It was attached to the transverse mesocolon, stomach, portal vein and superior mesenteric vessels. An en block resection of the mass with the head of the pancreas, transverse colon and the mesentery was performed.
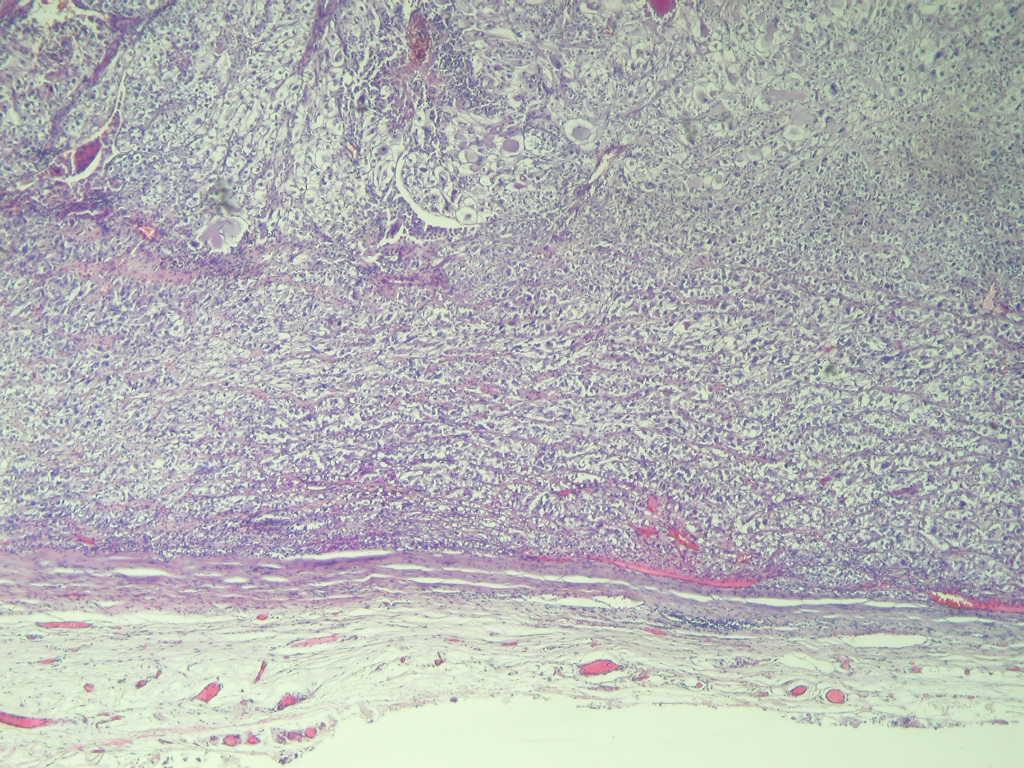
The mass was composed of gray-white solid tissue with large regions of yellow-gray necrosis. It was enclosed in a fibrous capsule with a peripheral rim of lymphoid tissue, suggesting the tumor had replaced a lymph node. The tumor had infiltrated the capsule and extended up to the excision margin.
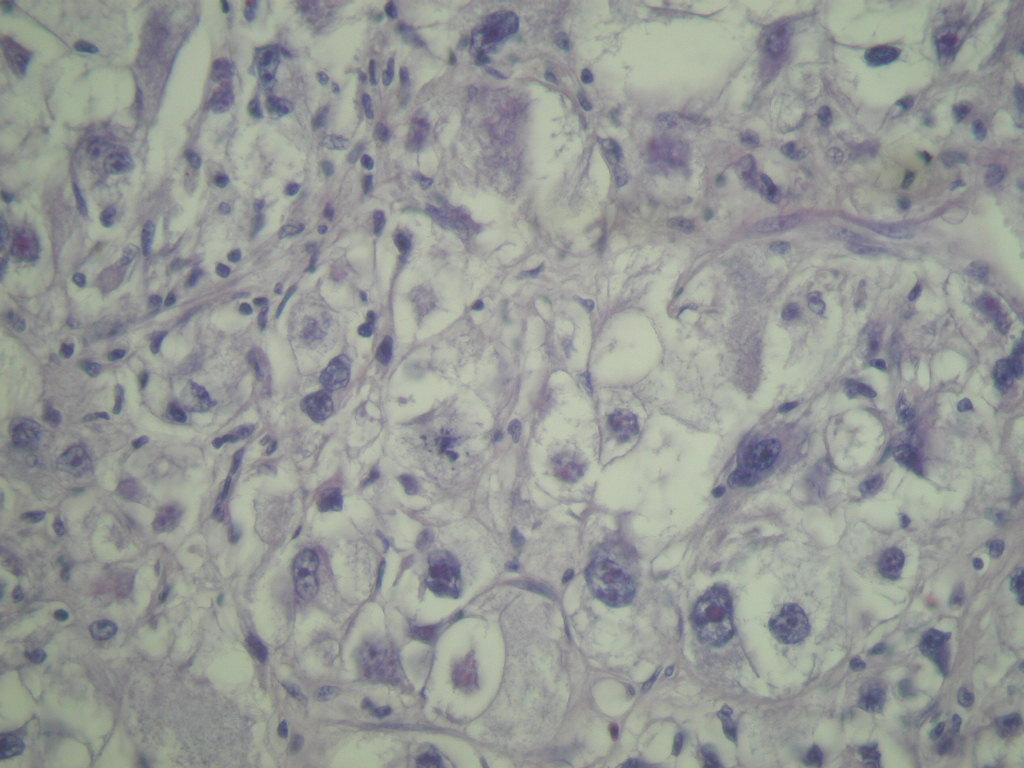
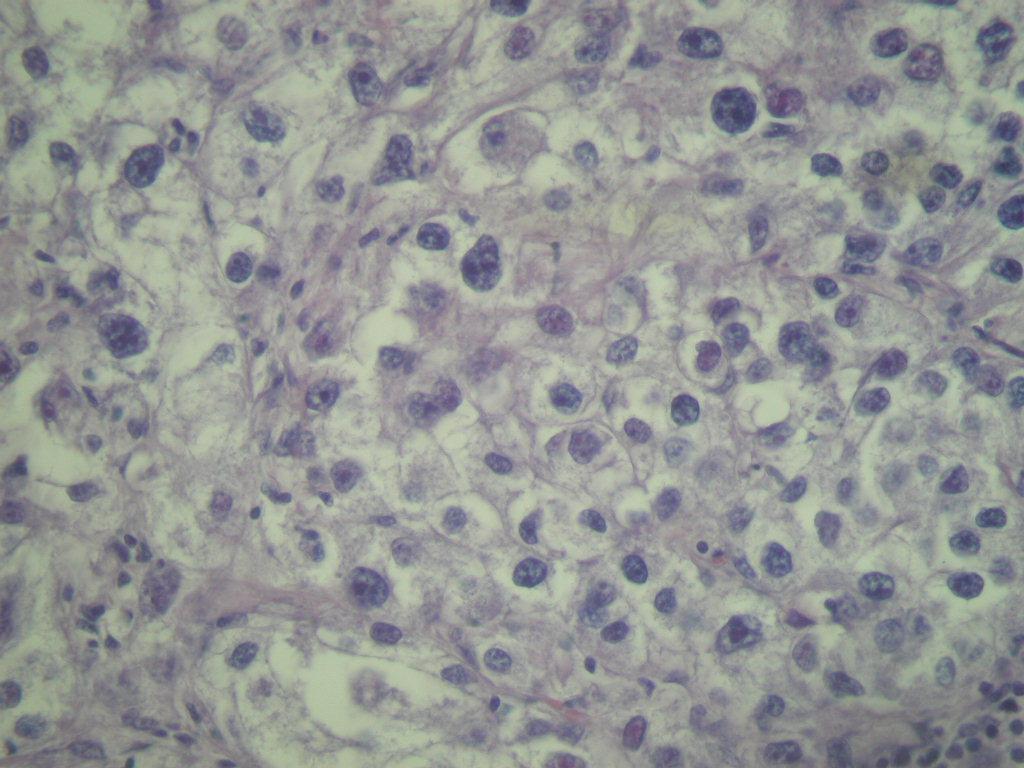
Microscopic images:
What is your diagnosis?
Diagnosis: Intra-abdominal PEComa
Discussion:
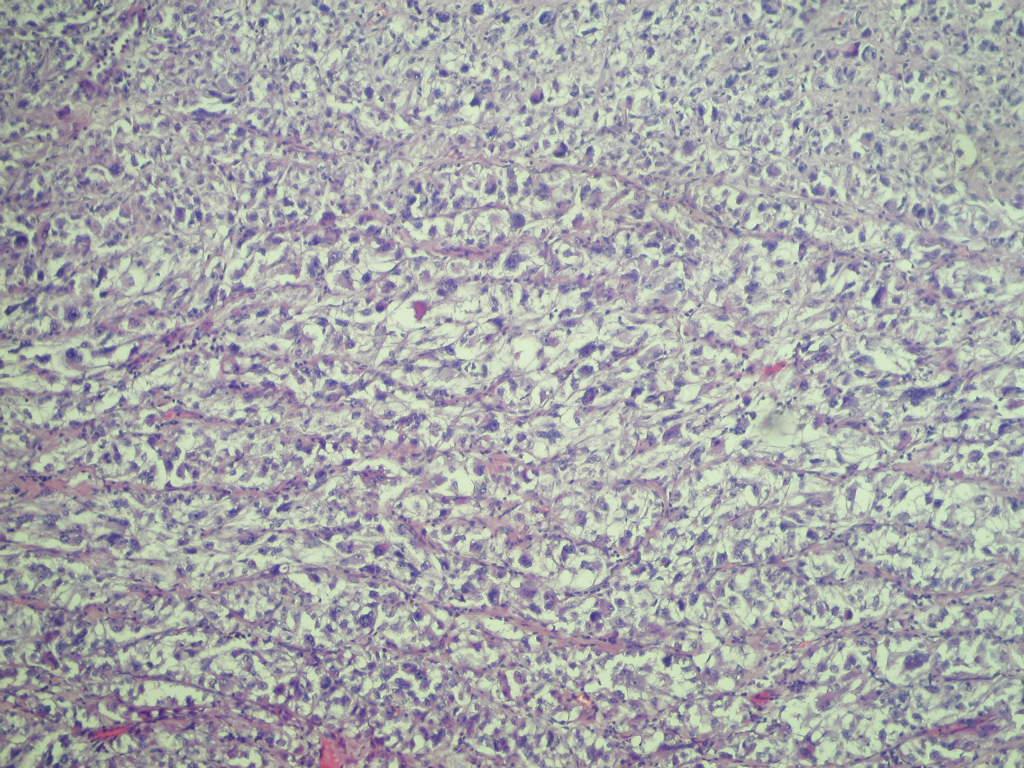
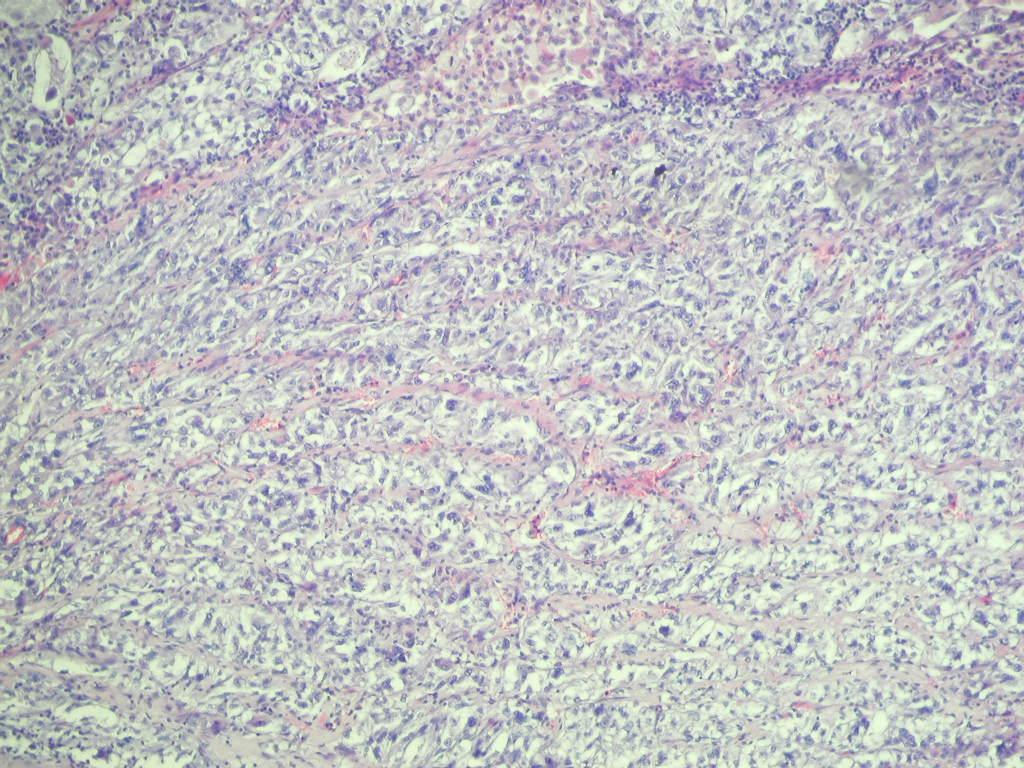
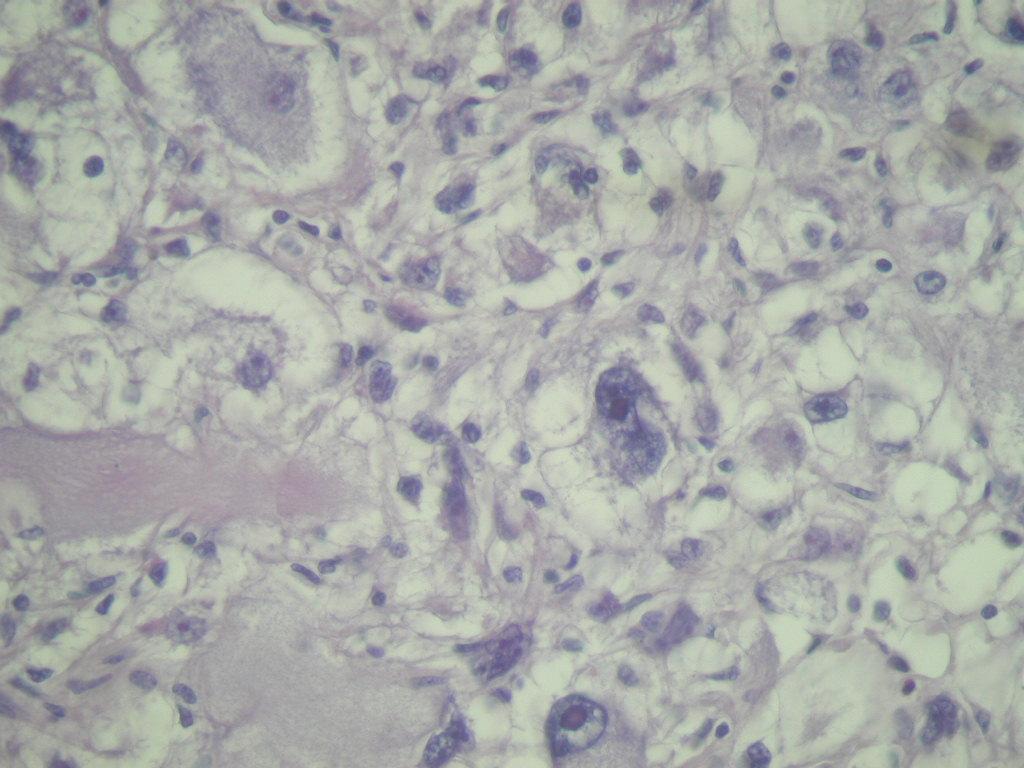
The tumor showed large zones of necrosis, with interspersed nests of malignant cells, which showed marked cellular pleomorphism and mitotic activity. The cells had clear to eosinophilic cytoplasm, with large vesicular nuclei and prominent eosinophilic nucleoli. Focally, there were areas showing a brown dusty pigment suggestive of melanin. There was no glandular growth or sarcomatous features.
The tumor cells were strongly immunoreactive for MelanA and HMB45, weakly positive for EMA and had focal weak positivity for S100. Tumor cells were negative for CD68, pan-keratin, LCA, CD117 and inhibin. There was no clinical history of a prior melanoma or other tumor. These findings are consistent with a perivascular epithelioid cell tumor (PEComa), originating from the transverse mesocolon and infiltrating lymphatic structures and its capsule. The diagnosis was confirmed by Dr. Christopher Fletcher (Harvard Medical School).
The concept of a perivascular epithelioid cell tumor was first proposed by Bonetti in 1992 (Am J Surg Pathol 1992;16:307). This tumor family includes angiomyolipoma (renal and extrarenal), clear cell sugar tumor (lung and extrapulmonary), lymphangioleiomyomatosis and related tumors of the falciform ligament / ligamentum teres, skin, uterus and other viscera and soft tissue (Histopathology 2005;46:498, Mod Pathol 2005;18:1336). There is no known normal counterpart to the perivascular epithelioid cell.
Histologically, these tumors are composed of epithelioid and spindle cells with immunoreactivity for melanocytic markers such as HMB45 and MelanA and myogenic markers such as actin (Int J Surg Pathol 2010;18:243). They are usually positive for CD1a (Pathol Int 2008;58:169).
The differential diagnosis is broad and includes melanoma, GIST tumors, clear cell sarcoma of soft parts, alveolar soft part sarcoma, leiomyosarcoma and even paraganglioma (Am J Surg Pathol 2009;33:475). In general, thorough sampling of the tumor, use of melanocytic markers and other immunostains and possibly molecular markers for characteristic cytogenetics will differentiate these disorders.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. David Cohen, Herzliya Medical Center, Israel.
Website news:
(1) We have extensively updated Kidney tumors, and split the topic into two smaller chapters, which will now be updated annually: Kidney tumor, Kidney nontumor
(2) We have added a new Management Page article, CMS Continues to Tinker with Anti-Markup Rule, POD Labs and In-Office Histology Labs in the Cross-Hairs, by John Outlaw, PSA, LLC.
Visit and follow our Blog to see recent updates to the website.
(1) We have extensively updated Kidney tumors, and split the topic into two smaller chapters, which will now be updated annually: Kidney tumor, Kidney nontumor
(2) We have added a new Management Page article, CMS Continues to Tinker with Anti-Markup Rule, POD Labs and In-Office Histology Labs in the Cross-Hairs, by John Outlaw, PSA, LLC.
Visit and follow our Blog to see recent updates to the website.
Case #143
Clinical history:
A 37 year old woman with no significant medical history was admitted for abdominal pain. Physical exam revealed a large mobile upper abdominal mass. Laboratory results as well as tumor markers were all within the normal range.
A laparotomy revealed a 20 x 15 cm, upper abdominal, highly vascularized and necrotic mass, that appeared to originate from the head of the pancreas. It was attached to the transverse mesocolon, stomach, portal vein and superior mesenteric vessels. An en block resection of the mass with the head of the pancreas, transverse colon and the mesentery was performed.
The mass was composed of gray-white solid tissue with large regions of yellow-gray necrosis. It was enclosed in a fibrous capsule with a peripheral rim of lymphoid tissue, suggesting the tumor had replaced a lymph node. The tumor had infiltrated the capsule and extended up to the excision margin.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Intra-abdominal PEComa
Discussion:
The tumor showed large zones of necrosis, with interspersed nests of malignant cells, which showed marked cellular pleomorphism and mitotic activity. The cells had clear to eosinophilic cytoplasm, with large vesicular nuclei and prominent eosinophilic nucleoli. Focally, there were areas showing a brown dusty pigment suggestive of melanin. There was no glandular growth or sarcomatous features.
The tumor cells were strongly immunoreactive for MelanA and HMB45, weakly positive for EMA and had focal weak positivity for S100. Tumor cells were negative for CD68, pan-keratin, LCA, CD117 and inhibin. There was no clinical history of a prior melanoma or other tumor. These findings are consistent with a perivascular epithelioid cell tumor (PEComa), originating from the transverse mesocolon and infiltrating lymphatic structures and its capsule. The diagnosis was confirmed by Dr. Christopher Fletcher (Harvard Medical School).
The concept of a perivascular epithelioid cell tumor was first proposed by Bonetti in 1992 (Am J Surg Pathol 1992;16:307). This tumor family includes angiomyolipoma (renal and extrarenal), clear cell sugar tumor (lung and extrapulmonary), lymphangioleiomyomatosis and related tumors of the falciform ligament / ligamentum teres, skin, uterus and other viscera and soft tissue (Histopathology 2005;46:498, Mod Pathol 2005;18:1336). There is no known normal counterpart to the perivascular epithelioid cell.
Histologically, these tumors are composed of epithelioid and spindle cells with immunoreactivity for melanocytic markers such as HMB45 and MelanA and myogenic markers such as actin (Int J Surg Pathol 2010;18:243). They are usually positive for CD1a (Pathol Int 2008;58:169).
The differential diagnosis is broad and includes melanoma, GIST tumors, clear cell sarcoma of soft parts, alveolar soft part sarcoma, leiomyosarcoma and even paraganglioma (Am J Surg Pathol 2009;33:475). In general, thorough sampling of the tumor, use of melanocytic markers and other immunostains and possibly molecular markers for characteristic cytogenetics will differentiate these disorders.