7 November 2008 - Case #134
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Angela Bohlke, Tulane University Hospital, New Orleans, Louisiana (USA).
Case #134
Clinical history:
A 10 year old girl presented with abdominal pain and anorexia. CT scan showed a 15 cm heterogeneous liver mass. Following rupture of the mass into the peritoneum, she was taken urgently to the operating room exploration and ultimately resection.
Gross image:
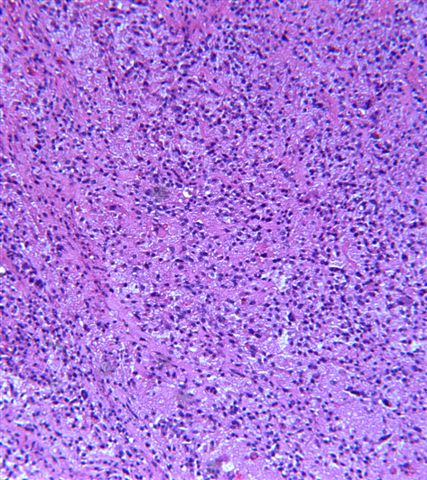
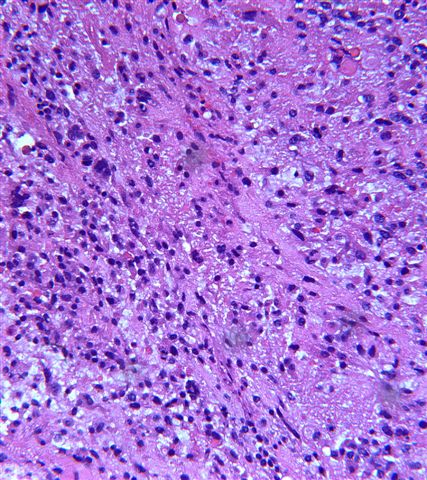
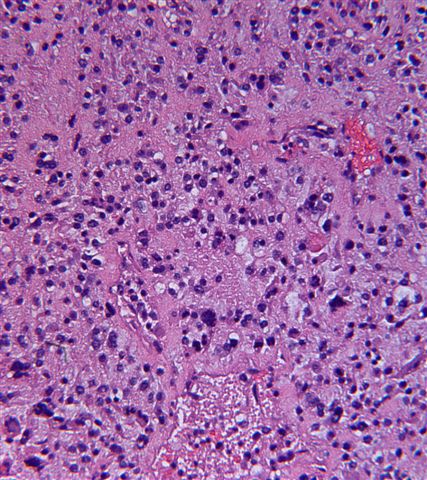
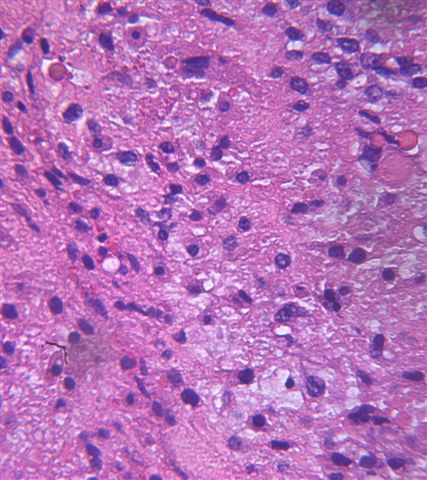
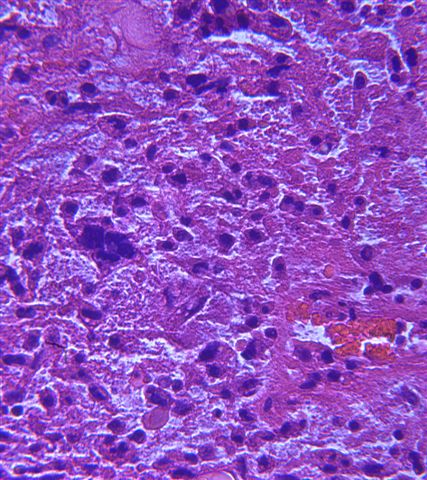
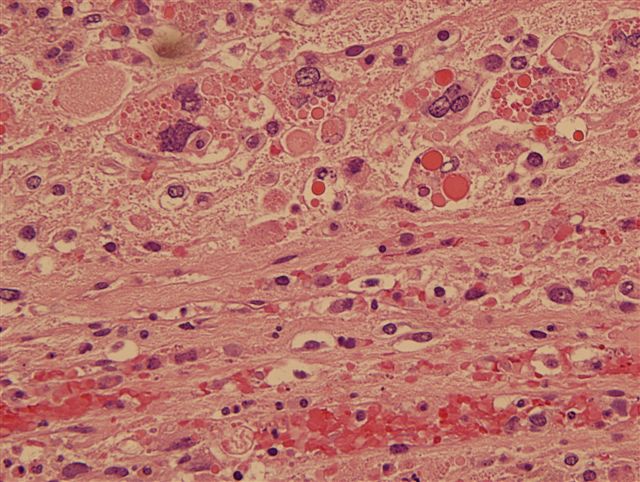
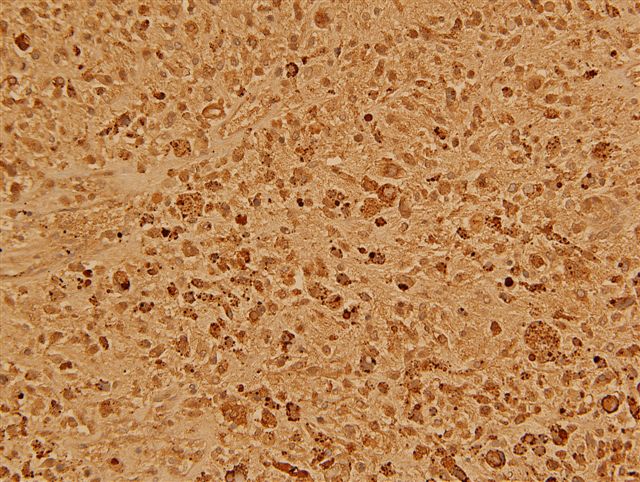
Microscopic images:
What is your diagnosis?
Diagnosis: Undifferentiated embryonal sarcoma
Discussion:
Undifferentiated embryonal sarcoma comprises 10% of pediatric tumors and is the third most common pediatric hepatic tumor after hepatoblastoma and hepatocellular carcinoma. It commonly occurs at ages 6 to 10 years and only rarely occurs in adults (Cancer 2008;112:2274). It typically presents with pain, fever, an abdominal mass and a normal serum AFP (J Pediatr Surg 2008;43:1912).
Grossly, the tumor is up to 30 cm, well demarcated and soft, with cystic, gelatinous, hemorrhagic or necrotic foci. Histologically, it has variable cellularity, and is composed of anaplastic and spindle cells with ill defined borders and prominent PAS+ diastase resistant hyaline globules. The nuclei have stippled chromatin and indistinct nucleoli. The stroma has numerous thin walled vessels and may be myxoid. There is frequent mitotic activity. The tumor periphery may demonstrate trapped hepatocytes or bile duct structures. Tumor cells are immunoreactive for vimentin with a high Ki67 index and negative for myogenin and keratin (Appl Immunohistochem Mol Morphol 2006;14:193). The hyaline globules are negative for alpha fetoprotein.
The differential diagnosis includes mesenchymal hamartoma (usually < 1 year old, cystic tumor with bland tumor cells and no giant cells), embryonal rhabdomyosarcoma (usually 2 - 6 years old, myxoid mass extending into bile duct, rhabdomyoblastic differentiation with cytoplasmic cross striations, cambium layer present but no diffuse anaplasia or hyaline globules, myogenin+, MyoD1+), sarcomatoid hepatocellular carcinoma and a mixed form of hepatoblastoma (Pediatr Dev Pathol 2007;10:89). Hydatid cyst is also a consideration in endemic areas (J Pediatr Surg 2008;43:E1).
Treatment is complete resection and chemotherapy and the prognosis is now considered good (J Gastrointest Surg 2007;11:73, Cancer 2002;94:252). Large tumors may rupture and cause death (J Pediatr Hematol Oncol 2007;29:63).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Angela Bohlke, Tulane University Hospital, New Orleans, Louisiana (USA).
Website news:
(1) How can you learn about new fellowship openings? We have a new email list sent out every two weeks, listing the new fellowships posted at our website. To subscribe, click here.
(2) Please visit our Management Page, to read the new article, The Tangled Web of Claim Payments - How Managed Care Contracts Kill Your Revenue. The informative articles on the Management Page are written exclusive for our website.
Visit and follow our Blog to see recent updates to the website.
(1) How can you learn about new fellowship openings? We have a new email list sent out every two weeks, listing the new fellowships posted at our website. To subscribe, click here.
(2) Please visit our Management Page, to read the new article, The Tangled Web of Claim Payments - How Managed Care Contracts Kill Your Revenue. The informative articles on the Management Page are written exclusive for our website.
Visit and follow our Blog to see recent updates to the website.
Case #134
Clinical history:
A 10 year old girl presented with abdominal pain and anorexia. CT scan showed a 15 cm heterogeneous liver mass. Following rupture of the mass into the peritoneum, she was taken urgently to the operating room exploration and ultimately resection.
Gross image:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Undifferentiated embryonal sarcoma
Discussion:
Undifferentiated embryonal sarcoma comprises 10% of pediatric tumors and is the third most common pediatric hepatic tumor after hepatoblastoma and hepatocellular carcinoma. It commonly occurs at ages 6 to 10 years and only rarely occurs in adults (Cancer 2008;112:2274). It typically presents with pain, fever, an abdominal mass and a normal serum AFP (J Pediatr Surg 2008;43:1912).
Grossly, the tumor is up to 30 cm, well demarcated and soft, with cystic, gelatinous, hemorrhagic or necrotic foci. Histologically, it has variable cellularity, and is composed of anaplastic and spindle cells with ill defined borders and prominent PAS+ diastase resistant hyaline globules. The nuclei have stippled chromatin and indistinct nucleoli. The stroma has numerous thin walled vessels and may be myxoid. There is frequent mitotic activity. The tumor periphery may demonstrate trapped hepatocytes or bile duct structures. Tumor cells are immunoreactive for vimentin with a high Ki67 index and negative for myogenin and keratin (Appl Immunohistochem Mol Morphol 2006;14:193). The hyaline globules are negative for alpha fetoprotein.
The differential diagnosis includes mesenchymal hamartoma (usually < 1 year old, cystic tumor with bland tumor cells and no giant cells), embryonal rhabdomyosarcoma (usually 2 - 6 years old, myxoid mass extending into bile duct, rhabdomyoblastic differentiation with cytoplasmic cross striations, cambium layer present but no diffuse anaplasia or hyaline globules, myogenin+, MyoD1+), sarcomatoid hepatocellular carcinoma and a mixed form of hepatoblastoma (Pediatr Dev Pathol 2007;10:89). Hydatid cyst is also a consideration in endemic areas (J Pediatr Surg 2008;43:E1).
Treatment is complete resection and chemotherapy and the prognosis is now considered good (J Gastrointest Surg 2007;11:73, Cancer 2002;94:252). Large tumors may rupture and cause death (J Pediatr Hematol Oncol 2007;29:63).