23 September 2008 - Case #130
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Drs. Mona Kandil, Moshera Abdel Wahed and Rehab Samaka, from Menofiya University, Egypt.

23rd Annual Park City Surgical Pathology Workshop
This 20-hour workshop is designed for the pathologist, clinician, and oncology specialist, focusing on surgical pathology, cytopathology, and hematopoietic pathology.
Short lectures and case-oriented discussions will include in-depth reviews of diagnostic anatomic pathology, insight into difficult differential diagnoses, use of immunohistochemistry and new technology to improve diagnosis.

Participants at the 23rd Annual Surgical Pathology Workshop will be asked to examine microscopic images and formulate a diagnosis and patient management strategy. The faculty pathologist will then discuss the diagnosis, differential diagnosis, patient management, and other pertinent features. Cases will be selected to represent common and/or difficult diagnostic problems. Held at The Canyons in Park City, Utah.
Advertisement
Case #130
Clinical history:
A 27 year old woman presented with painful swelling in the fibula. There was a history of an aneurysmal bone cell 5 years previously. Xrays showed a punched out, lytic, intramedullary lesion in the distal fibula. There was no sclerotic rim or periosteal reaction. A segment of fibula was excised.
Radiology images:
Gross image:
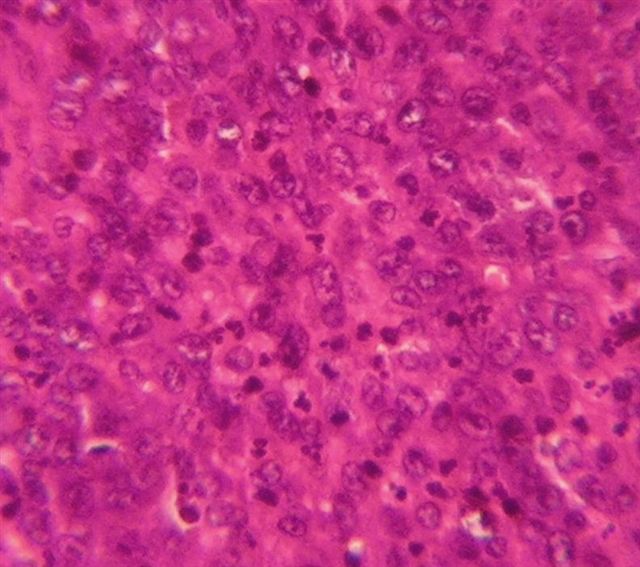
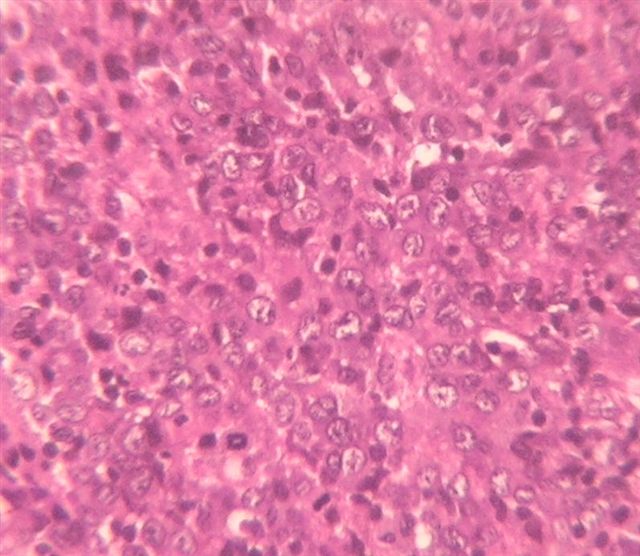
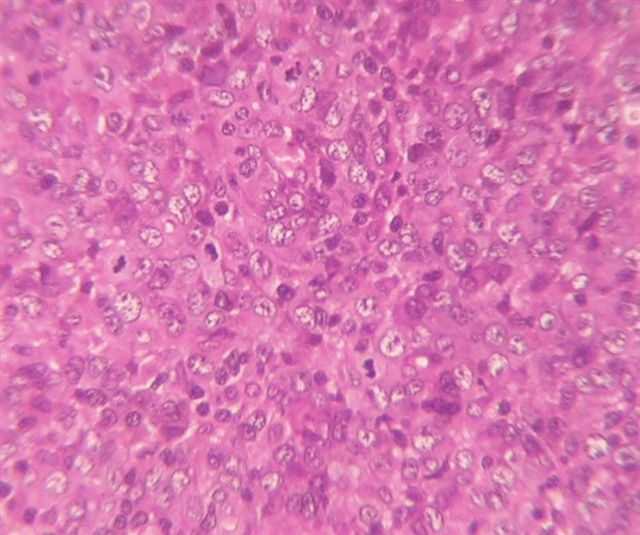
Microscopic images:
What is your diagnosis?
Diagnosis: Myeloid (granulocytic) sarcoma
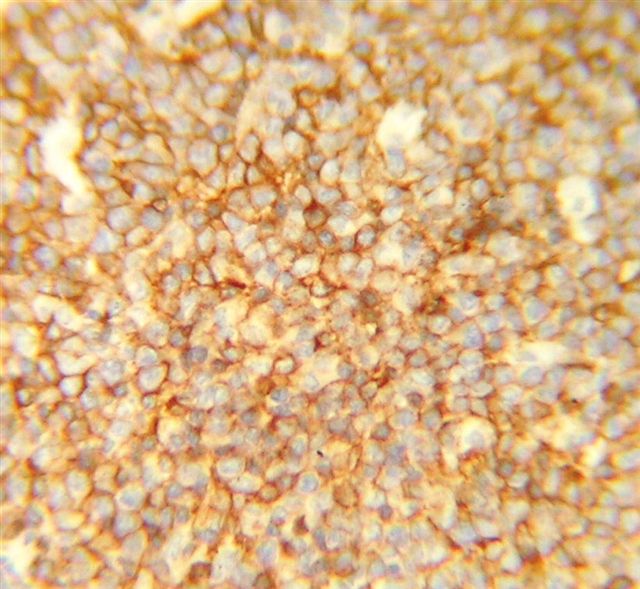
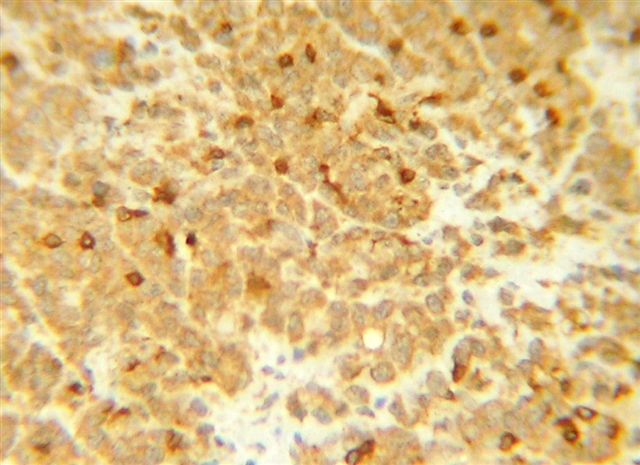
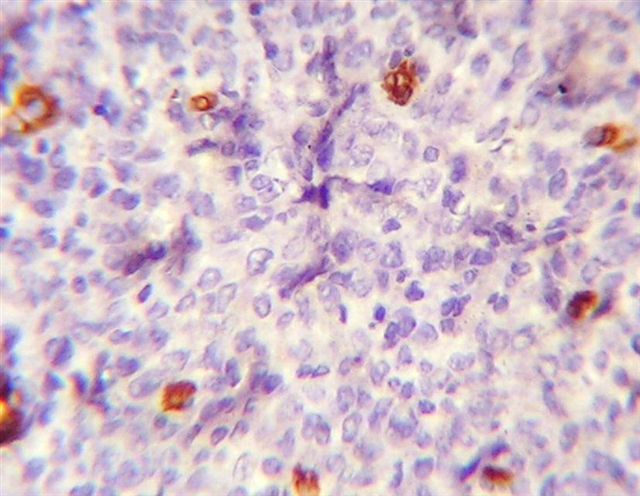
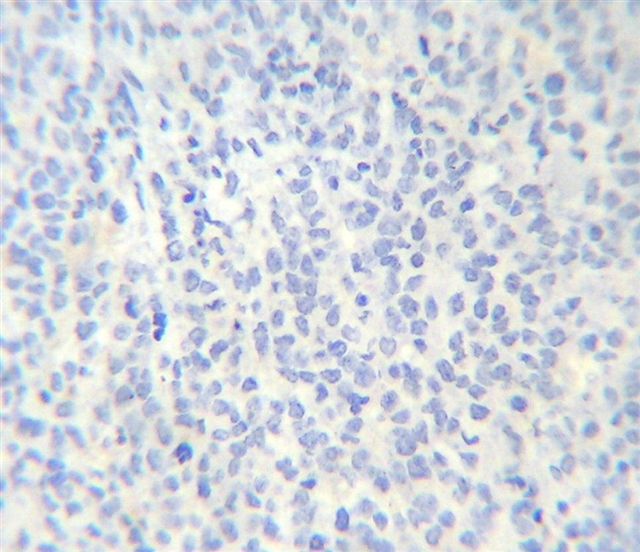
Immunostains:
Discussion:
Special stains showed diffuse immunoreactivity for CD45 / LCA and focal reactivity for CD45RO, CD3 and CD34. A CD20 stain was negative. A myeloperoxidase stain (not available) was also positive.
Myeloid sarcoma is also called granulocytic sarcoma, extramedullary myeloid tumor or chloroma. It presents as a mass lesion, usually associated with AML M4 or M5 or a chromic myeloproliferative syndrome, although rarely no leukemia or myelodysplasia is identified in blood or bone marrow (J Neurosurg 2006;105:916). At all sites combined, it is found in 2 - 8% of AML patients.
The morphology of the leukemic infiltrates resembles the underlying disease. Myeloid tumors may be (a) blastic, with myeloblasts containing a mild / moderate rim of basophilic cytoplasm, fine nuclear chromatin and 2 - 4 nucleoli; (b) immature with myeloblasts, promyelocytes and eosinophilic myelocytes; or (c) differentiated with promyelocytes, eosinophilic myelocytes and more mature forms.
Myeloid sarcoma is often misdiagnosed. Immunostains are necessary to differentiate these tumors from lymphoma. All tumors are typically immunoreactive for lysozyme and CD43. Myeloid tumors are commonly immunoreactive for myeloperoxidase and CD117 (Archives 2001;125:1448). Monocytic tumors are typically immunoreactive for CD68 and CD163 (Diagn Pathol 2007;2:42). Tumor cells may express CD45 / LCA but are typically negative for CD3, CD20 and CD79a.
Aggressive treatment, including bone marrow transplantation, is recommended (Leukemia 2007;21:340, Cancer 2002;94:1739).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Drs. Mona Kandil, Moshera Abdel Wahed and Rehab Samaka, from Menofiya University, Egypt.

This 20-hour workshop is designed for the pathologist, clinician, and oncology specialist, focusing on surgical pathology, cytopathology, and hematopoietic pathology.
Short lectures and case-oriented discussions will include in-depth reviews of diagnostic anatomic pathology, insight into difficult differential diagnoses, use of immunohistochemistry and new technology to improve diagnosis.

Participants at the 23rd Annual Surgical Pathology Workshop will be asked to examine microscopic images and formulate a diagnosis and patient management strategy. The faculty pathologist will then discuss the diagnosis, differential diagnosis, patient management, and other pertinent features. Cases will be selected to represent common and/or difficult diagnostic problems. Held at The Canyons in Park City, Utah.
Website news:
(1) We have split the chapter on Skin tumors into separate chapters for Melanocytic and Non-melanocytic tumors, and are currently updating the Melanocytic tumors chapter.
Visit and follow our Blog to see recent updates to the website.
(1) We have split the chapter on Skin tumors into separate chapters for Melanocytic and Non-melanocytic tumors, and are currently updating the Melanocytic tumors chapter.
Visit and follow our Blog to see recent updates to the website.
Case #130
Clinical history:
A 27 year old woman presented with painful swelling in the fibula. There was a history of an aneurysmal bone cell 5 years previously. Xrays showed a punched out, lytic, intramedullary lesion in the distal fibula. There was no sclerotic rim or periosteal reaction. A segment of fibula was excised.
Radiology images:
Gross image:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Myeloid (granulocytic) sarcoma
Immunostains:
Discussion:
Special stains showed diffuse immunoreactivity for CD45 / LCA and focal reactivity for CD45RO, CD3 and CD34. A CD20 stain was negative. A myeloperoxidase stain (not available) was also positive.
Myeloid sarcoma is also called granulocytic sarcoma, extramedullary myeloid tumor or chloroma. It presents as a mass lesion, usually associated with AML M4 or M5 or a chromic myeloproliferative syndrome, although rarely no leukemia or myelodysplasia is identified in blood or bone marrow (J Neurosurg 2006;105:916). At all sites combined, it is found in 2 - 8% of AML patients.
The morphology of the leukemic infiltrates resembles the underlying disease. Myeloid tumors may be (a) blastic, with myeloblasts containing a mild / moderate rim of basophilic cytoplasm, fine nuclear chromatin and 2 - 4 nucleoli; (b) immature with myeloblasts, promyelocytes and eosinophilic myelocytes; or (c) differentiated with promyelocytes, eosinophilic myelocytes and more mature forms.
Myeloid sarcoma is often misdiagnosed. Immunostains are necessary to differentiate these tumors from lymphoma. All tumors are typically immunoreactive for lysozyme and CD43. Myeloid tumors are commonly immunoreactive for myeloperoxidase and CD117 (Archives 2001;125:1448). Monocytic tumors are typically immunoreactive for CD68 and CD163 (Diagn Pathol 2007;2:42). Tumor cells may express CD45 / LCA but are typically negative for CD3, CD20 and CD79a.
Aggressive treatment, including bone marrow transplantation, is recommended (Leukemia 2007;21:340, Cancer 2002;94:1739).