14 August 2008 - Case #127
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Elaine Alt and Dr. Marise McNeeley, Quest Diagnostics, New Jersey (USA).
Case #127
Clinical history:
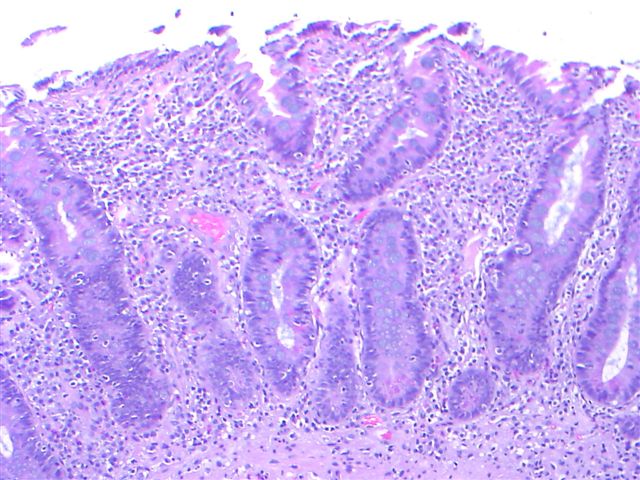
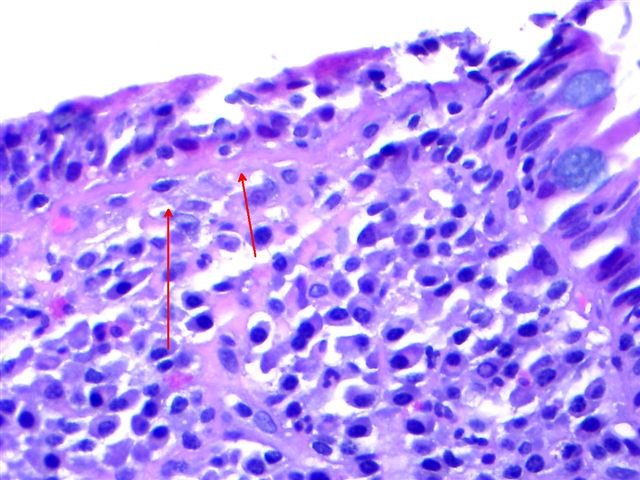
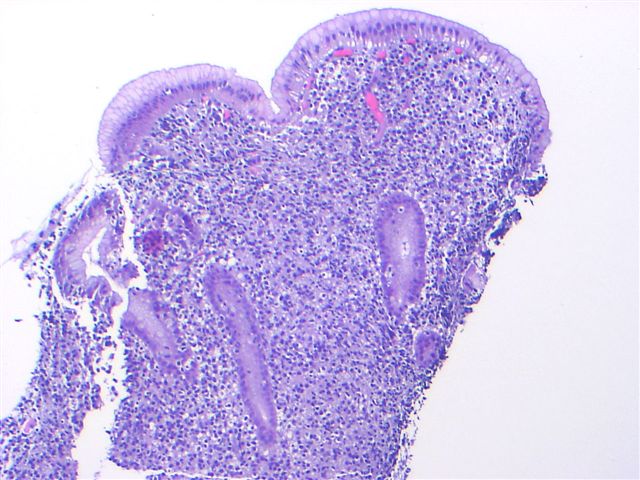
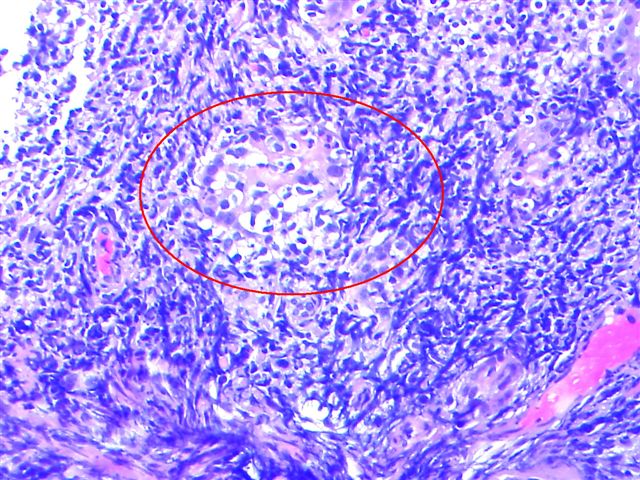
A 56 year old woman had a long history of untreated celiac sprue. An endoscopy showed nodular, ill defined areas in the antrum and gastritis. Small bowel and gastric biopsies were obtained.
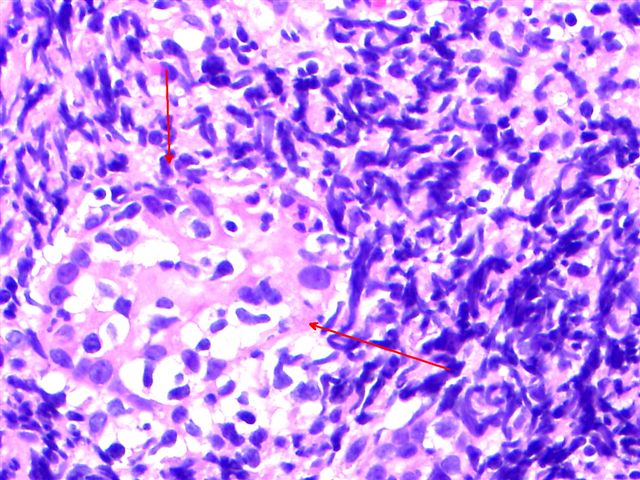
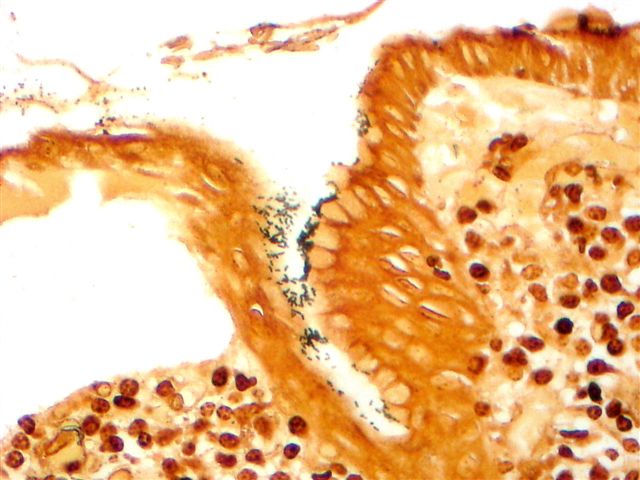
Microscopic images:
What is your diagnosis?
Diagnosis: Stomach biopsies - MALT lymphoma, H. pylori gastritis; small bowel biopsy (changes consistent with celiac disease)
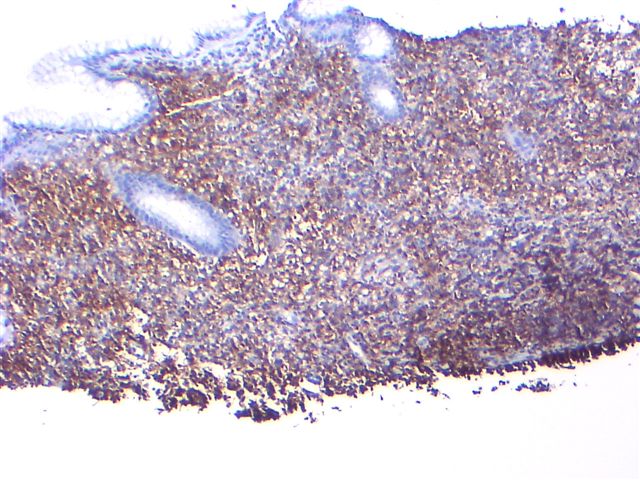
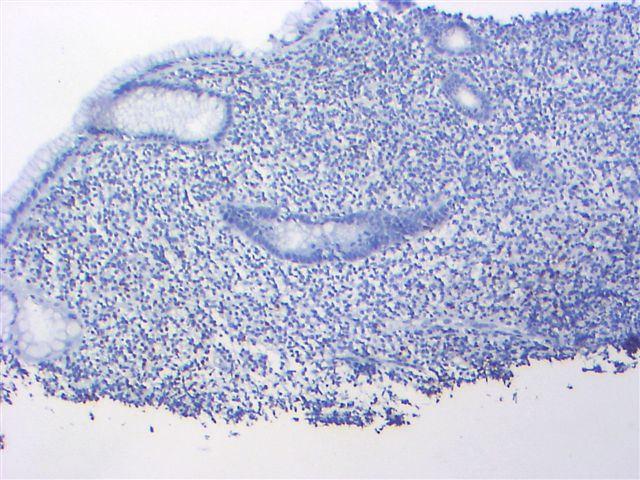
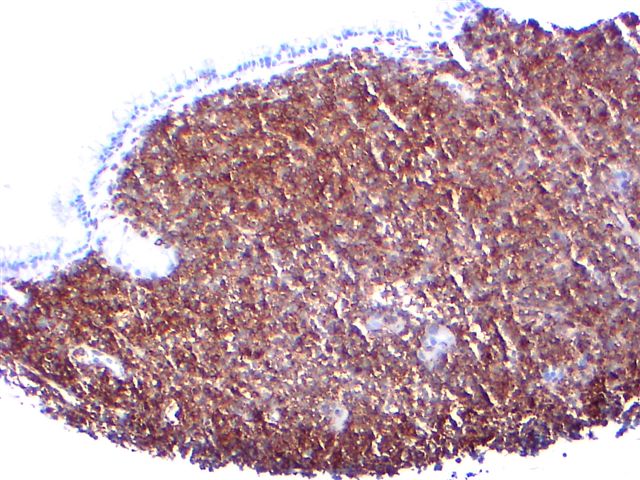
Immunostains:
Discussion:
MALT lymphoma is characterized by a dense, monotonous population of centrocyte-like cells, lymphoepithelial lesions (infiltration of glandular epithelium by lymphocytes) and frequent follicular colonization. The tumor cells may also have plasmacytoid differentiation. Tumor cells are immunoreactive for B cell markers, including CD19, CD20 and CD79a, as well as BCL10, with variable CD43 staining. They exhibit monoclonal light chain staining. This case demonstrated monoclonal heavy chain rearrangement by molecular studies.
Gastric MALT lymphomas are closely linked to Helicobacter pylori infection and H. pylori eradication therapy produces a long term favorable outcome (Tohoku J Exp Med 2008;214:79).
Celiac disease or gluten sensitive enteropathy, is a T cell mediated disease of genetically susceptible individuals, induced by ingesting proteins in wheat (gliadins), barley (hordeins) or rye (secalinin). Symptoms include episodic diarrhea, abdominal pain and distention and weight loss, with clinical and microscopic improvement after dietary withdrawal (Clin Med Res 2004;2:71). Microscopic changes include an increase in intraepithelial lymphocytes of 40+ lymphocytes/100 surface or upper crypt enterocytes, or early clustering of 12+ lymphocytes at the tip of villi and extending evenly down the sides of the villus (Mod Path 2003;16:342). There is also diffuse enteritis with marked atrophy or total loss of villi and elongated crypts. Definitive diagnosis requires these histologic findings plus positive serology and favorable clinical and serologic responses after dietary change. The differential diagnosis includes duodenal intraepithelial lymphocytosis with normal villous architecture, associated with H. pylori infection, but without any other features of celiac disease (Mod Path 2005;18:1134).
In this case, the presence of celiac sprue appears to be incidental. Celiac sprue is associated with an increased risk of malignant intestinal disease but this is usually T cell intestinal lymphoma of the small bowel, not MALT lymphoma of the stomach. Celiac sprue does not appear to be associated with H. pylori gastritis (Am J Gastroenterol 2006;101:1880).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Elaine Alt and Dr. Marise McNeeley, Quest Diagnostics, New Jersey (USA).
Website news:
(1) Please tell any new staff, residents or fellows about PathologyOutlines.com, and about our mailing lists. We want to make our website more useful to you. Tell us how we can make it better by email (Comments@pathologyoutlines.com) or by stopping by our booths at the upcoming AAPA, CAP or ASCP meetings.
Visit and follow our Blog to see recent updates to the website.
(1) Please tell any new staff, residents or fellows about PathologyOutlines.com, and about our mailing lists. We want to make our website more useful to you. Tell us how we can make it better by email (Comments@pathologyoutlines.com) or by stopping by our booths at the upcoming AAPA, CAP or ASCP meetings.
Visit and follow our Blog to see recent updates to the website.
Case #127
Clinical history:
A 56 year old woman had a long history of untreated celiac sprue. An endoscopy showed nodular, ill defined areas in the antrum and gastritis. Small bowel and gastric biopsies were obtained.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Stomach biopsies - MALT lymphoma, H. pylori gastritis; small bowel biopsy (changes consistent with celiac disease)
Immunostains:
Discussion:
MALT lymphoma is characterized by a dense, monotonous population of centrocyte-like cells, lymphoepithelial lesions (infiltration of glandular epithelium by lymphocytes) and frequent follicular colonization. The tumor cells may also have plasmacytoid differentiation. Tumor cells are immunoreactive for B cell markers, including CD19, CD20 and CD79a, as well as BCL10, with variable CD43 staining. They exhibit monoclonal light chain staining. This case demonstrated monoclonal heavy chain rearrangement by molecular studies.
Gastric MALT lymphomas are closely linked to Helicobacter pylori infection and H. pylori eradication therapy produces a long term favorable outcome (Tohoku J Exp Med 2008;214:79).
Celiac disease or gluten sensitive enteropathy, is a T cell mediated disease of genetically susceptible individuals, induced by ingesting proteins in wheat (gliadins), barley (hordeins) or rye (secalinin). Symptoms include episodic diarrhea, abdominal pain and distention and weight loss, with clinical and microscopic improvement after dietary withdrawal (Clin Med Res 2004;2:71). Microscopic changes include an increase in intraepithelial lymphocytes of 40+ lymphocytes/100 surface or upper crypt enterocytes, or early clustering of 12+ lymphocytes at the tip of villi and extending evenly down the sides of the villus (Mod Path 2003;16:342). There is also diffuse enteritis with marked atrophy or total loss of villi and elongated crypts. Definitive diagnosis requires these histologic findings plus positive serology and favorable clinical and serologic responses after dietary change. The differential diagnosis includes duodenal intraepithelial lymphocytosis with normal villous architecture, associated with H. pylori infection, but without any other features of celiac disease (Mod Path 2005;18:1134).
In this case, the presence of celiac sprue appears to be incidental. Celiac sprue is associated with an increased risk of malignant intestinal disease but this is usually T cell intestinal lymphoma of the small bowel, not MALT lymphoma of the stomach. Celiac sprue does not appear to be associated with H. pylori gastritis (Am J Gastroenterol 2006;101:1880).