13 June 2008 - Case #122
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. R. F. Chinoy, Tata Memorial Hospital, Parel, Mumbai (India).

Attend the
Annual Summer Update in Clinical Immunology,
Microbiology and Infectious Diseases
July 14-18, 2008
Snow King Resort
Jackson, Wyoming (USA)
This 25.75-hour review and update in clinical immunology, microbiology and infectious diseases is intended to improve knowledge about the pathogenesis and clinical manifestations of infectious diseases, immunological mechanisms of disease and disease prevention, appropriate approaches to the diagnosis of infections and immunologic disorders, and utilization of the clinical microbiology and immunology laboratory, including selection and interpretation of results.
This course will provide a forum for the exchange of ideas dealing with microbial infections as well as immunity to infectious diseases and immunologic disorders.
Advertisement
Case #122
Clinical history:
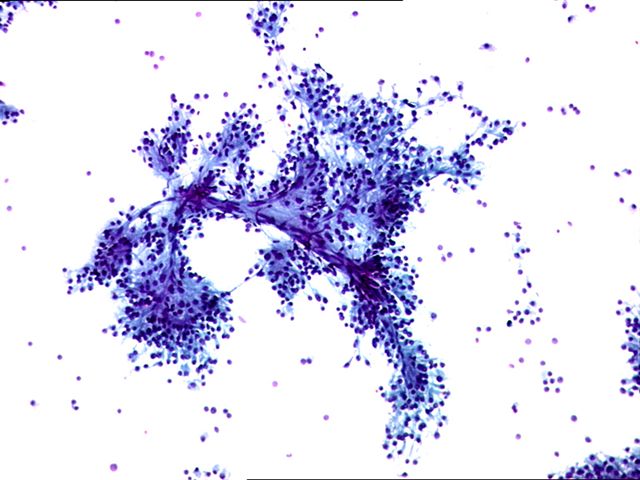
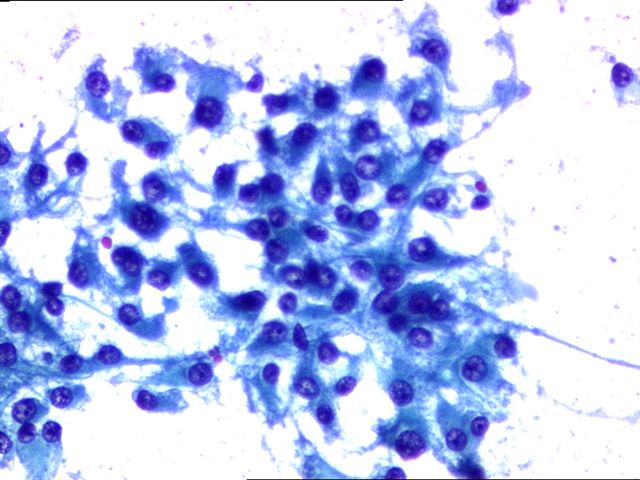
A 43 year old man presented with a painless testicular mass and normal serum AFP and beta-hCG. Fine needle aspiration cytology was followed by orchiectomy.
The tumor was 2.5 cm, tan brown and soft. The mass was within the testicular parenchyma.
Cytology images:
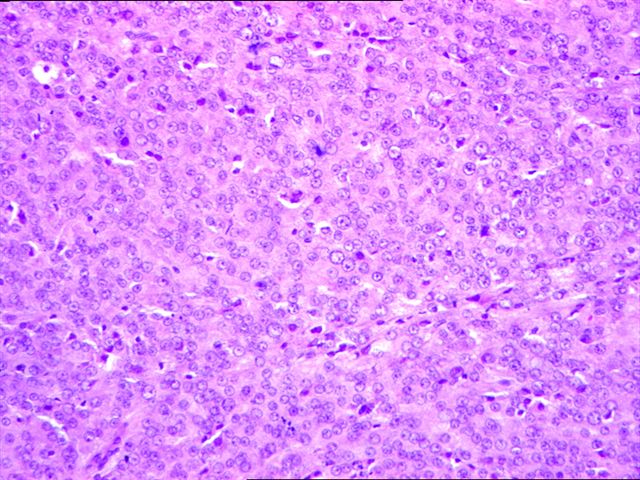
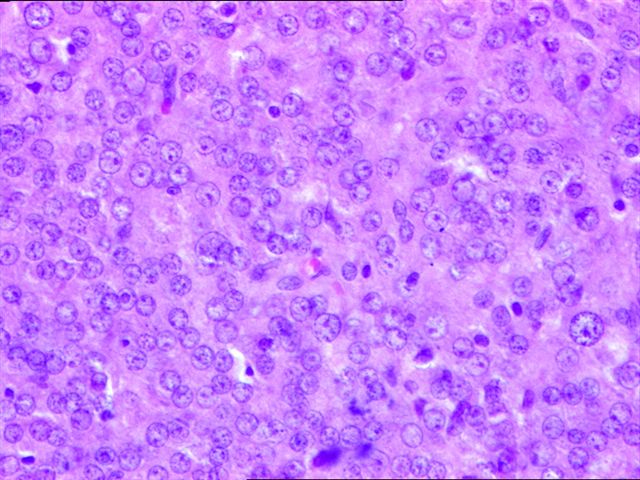
Microscopic images:
What is your diagnosis?
Diagnosis: Leydig cell tumor of the testes
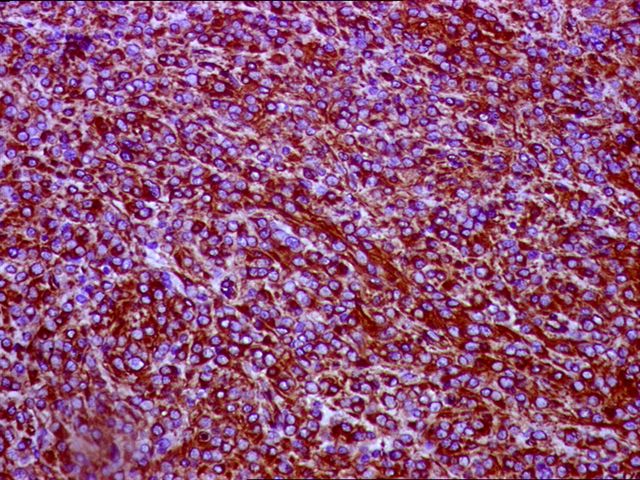
Immunostains:
Discussion:
An inhibin stain was diffusely and strongly positive.
Leydig cell tumors comprise 1 - 3% of testicular tumors. Although they arise at any age, most patients are 20 - 60 years old. They often secrete androgens, estrogens or corticosteriods and patients may present with gynecomastia or other feminizing symptoms or with precocious puberty without spermatocytic maturation (Hum Path 1977;8:621).
Grossly, the tumor is usually a solid, well circumscribed nodule 5 cm or less, with a distinct golden-brown homogenous cut surface. Up to 10% have extratesticular extension. Microscopically, there are sheets, nests, ribbons or cords of large, round or polygonal cells with defined cell borders, eosinophilic cytoplasm and round central nuclei. The cytoplasm may contain vacuoles, lipofuscin or Reinke crystals (35%). The tumor cells may display endocrine atypia. Occasionally, cells may have adipose differentiation, which should not be confused with extratesticular extension (Am J Surg Pathol 2002;26:1424). There is no / rare mitotic activity.
Positive immunostains include inhibin, MelanA and keratin, as well as vimentin and steroid hormones. Tumor cells are negative for S100.
The differential diagnosis includes nodular Leydig cell hyperplasia (associated with cryptorchidism, usually 1 cm or less, multifocal, does not destroy surrounding tubules), large cell calcifying Sertoli cell tumor (usually multifocal, often bilateral, more stroma, calcifications, intratubular growth, no Reinkes crystals, slightly different immunostaining pattern) and testicular tumors of adrenogenital syndrome (bilateral, multifocal, clinical symptoms, laboratory findings, shrink after corticosteroid therapy) (Pathol Int 2005;55:366).
Orchiectomy is usually curative for benign tumors, although testis sparing surgery has also been advocated for young men (Int J Clin Pract 2003;57:912). In adults, 10% of tumors have malignant behavior, with metastases to lymph nodes, lung and liver. These tumors are usually > 5 cm with necrosis, vascular invasion, nuclear atypia, numerous mitoses including atypical ones and infiltrative margins.
References: Arch Pathol Lab Med 2007;131:311, Am J Surg Pathol 1985;9:177, eMedicine: Leydig Cell Tumors [Accessed 6 May 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. R. F. Chinoy, Tata Memorial Hospital, Parel, Mumbai (India).

Annual Summer Update in Clinical Immunology,
Microbiology and Infectious Diseases
July 14-18, 2008
Snow King Resort
Jackson, Wyoming (USA)
This 25.75-hour review and update in clinical immunology, microbiology and infectious diseases is intended to improve knowledge about the pathogenesis and clinical manifestations of infectious diseases, immunological mechanisms of disease and disease prevention, appropriate approaches to the diagnosis of infections and immunologic disorders, and utilization of the clinical microbiology and immunology laboratory, including selection and interpretation of results.
This course will provide a forum for the exchange of ideas dealing with microbial infections as well as immunity to infectious diseases and immunologic disorders.
Website news:
(1) Visit and use our newly updated chapter - Soft Tissue Tumors-Part 1. It starts with approaches to diagnosis, syndromes, grading and molecular patterns. It then discusses all known fibroblastic / myofibroblastic, fibrohistiocytic and lipomatous tumors, include WHO and non-WHO entities (the remaining soft tissue tumors are discussed in the Soft Tissue Tumors-Part 2 chapter). Each entity contains an extensive discussion of clinical, gross, micro, stains and molecular features. Use the 1000+ high quality image links in this chapter to assist with signout, to educate other physicians or for preparing talks.
Visit and follow our Blog to see recent updates to the website.
(1) Visit and use our newly updated chapter - Soft Tissue Tumors-Part 1. It starts with approaches to diagnosis, syndromes, grading and molecular patterns. It then discusses all known fibroblastic / myofibroblastic, fibrohistiocytic and lipomatous tumors, include WHO and non-WHO entities (the remaining soft tissue tumors are discussed in the Soft Tissue Tumors-Part 2 chapter). Each entity contains an extensive discussion of clinical, gross, micro, stains and molecular features. Use the 1000+ high quality image links in this chapter to assist with signout, to educate other physicians or for preparing talks.
Visit and follow our Blog to see recent updates to the website.
Case #122
Clinical history:
A 43 year old man presented with a painless testicular mass and normal serum AFP and beta-hCG. Fine needle aspiration cytology was followed by orchiectomy.
The tumor was 2.5 cm, tan brown and soft. The mass was within the testicular parenchyma.
Cytology images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Leydig cell tumor of the testes
Immunostains:
Discussion:
An inhibin stain was diffusely and strongly positive.
Leydig cell tumors comprise 1 - 3% of testicular tumors. Although they arise at any age, most patients are 20 - 60 years old. They often secrete androgens, estrogens or corticosteriods and patients may present with gynecomastia or other feminizing symptoms or with precocious puberty without spermatocytic maturation (Hum Path 1977;8:621).
Grossly, the tumor is usually a solid, well circumscribed nodule 5 cm or less, with a distinct golden-brown homogenous cut surface. Up to 10% have extratesticular extension. Microscopically, there are sheets, nests, ribbons or cords of large, round or polygonal cells with defined cell borders, eosinophilic cytoplasm and round central nuclei. The cytoplasm may contain vacuoles, lipofuscin or Reinke crystals (35%). The tumor cells may display endocrine atypia. Occasionally, cells may have adipose differentiation, which should not be confused with extratesticular extension (Am J Surg Pathol 2002;26:1424). There is no / rare mitotic activity.
Positive immunostains include inhibin, MelanA and keratin, as well as vimentin and steroid hormones. Tumor cells are negative for S100.
The differential diagnosis includes nodular Leydig cell hyperplasia (associated with cryptorchidism, usually 1 cm or less, multifocal, does not destroy surrounding tubules), large cell calcifying Sertoli cell tumor (usually multifocal, often bilateral, more stroma, calcifications, intratubular growth, no Reinkes crystals, slightly different immunostaining pattern) and testicular tumors of adrenogenital syndrome (bilateral, multifocal, clinical symptoms, laboratory findings, shrink after corticosteroid therapy) (Pathol Int 2005;55:366).
Orchiectomy is usually curative for benign tumors, although testis sparing surgery has also been advocated for young men (Int J Clin Pract 2003;57:912). In adults, 10% of tumors have malignant behavior, with metastases to lymph nodes, lung and liver. These tumors are usually > 5 cm with necrosis, vascular invasion, nuclear atypia, numerous mitoses including atypical ones and infiltrative margins.
References: Arch Pathol Lab Med 2007;131:311, Am J Surg Pathol 1985;9:177, eMedicine: Leydig Cell Tumors [Accessed 6 May 2024]