Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Schulte JJ, Lastra RR. Serous carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusserous.html. Accessed April 19th, 2024.
Definition / general
- High grade estrogen independent carcinoma of the endometrium showing marked cytologic atypia
- Complex papillary, solid or glandular architecture; similar to ovarian / tubal high grade serous carcinoma
Essential features
- High grade carcinoma arising in postmenopausal women
- Often arises within endometrial polyps; background endometrium often atrophic
- Immunohistochemistry shows mutational pattern of p53 expression (strong and diffuse or complete absence)
- Associated with worse prognosis than endometrioid carcinoma and can present at high stage
Terminology
- Endometrial serous carcinoma
- Historical: uterine papillary serous carcinoma
- Serous endometrial intraepithelial carcinoma: replacement of the surface epithelium or preformed endometrial glands with serous carcinoma without invasion of underlying stroma (Adv Anat Pathol 2004;11:117)
ICD coding
Epidemiology
- Accounts for approximately 5 - 10% of endometrial carcinomas (Adv Anat Pathol 2004;11:117; Br J Cancer 2006;94:642)
- Typically postmenopausal, nonobese women, estrogen independent (Adv Anat Pathol 2004;11:117)
- More often African American with a history of pelvic radiation or tamoxifen use (Int J Cancer 2018;142:1102; Gynecol Oncol 2013;129:277)
Sites
- Uterine corpus
- More likely to present at high stage (disease outside uterus) than endometrioid carcinomas, even when confined to a polyp or without evidence of invasive disease (Br J Cancer 2006;94:642)
Pathophysiology
- Frequently arises on the surface of an endometrial polyp in a background of atrophic endometrium (Adv Anat Pathol 2004;11:117)
- Often harbors mutations in TP53 but may also show alterations of PI3K / AKT / mTOR and MAPK pathways (J Surg Oncol 2015;112:188)
Etiology
- Mutations in TP53
- Possible association with BRCA1/2 mutations (JAMA Oncol 2016;2:1434, Clin Cancer Res 2019;25:7517)
Clinical features
- Postmenopausal bleeding is common
Diagnosis
- Diagnosis can be made on endometrial biopsy, curettage or polypectomy upon workup for postmenopausal bleeding
- Incidental carcinomas can be found, usually in association with endometrial polyps, within uteri removed for benign conditions
Laboratory
- Can show elevated tumor marker CA-125
Prognostic factors
- Typically regarded as an aggressive subtype of endometrial cancer
- More recent data suggests survival up to 80% for small low stage tumors (Adv Anat Pathol 2004;11:117)
- Higher stage, age > 60, race (African American) associated with increased mortality (Int J Gynecol Cancer 2017;27:85)
Case reports
- 50 - 61 year old women with serous carcinoma arising in endometrial polyps (Ann Diagn Pathol 2013;17:256)
- 55 and 64 year old Chinese women with serous carcinoma arising from adenomyosis / adenomyotic cyst (Diagn Pathol 2016;11:46)
- 60 year old woman with adrenal metastasis from uterine serous carcinoma (Am J Case Rep 2016;17:289)
- 71 year old woman with uterine serous carcinoma with renal and para-aortic metastases (Gynecol Oncol Rep 2019;28:12)
- Case report and literature review linking uterine serous carcinoma and BRCA mutation (Eur J Cancer 2017;72:215)
Treatment
- Treatment is primarily surgical + / - platinum based chemotherapy / radiotherapy
- Recent studies suggest a role for treatment with trastuzumab in patients with tumors showing overexpression of HER2 (J Clin Oncol 2018;36:2044)
- Pembrolizumab if tumor is microsatellite instability-high (MSI-H) or MMR-deficient (Clin Cancer Res 2019;25:3753)
Gross description
- No unique gross findings which would separate serous from nonserous carcinoma
- Endometrial polyp may be present
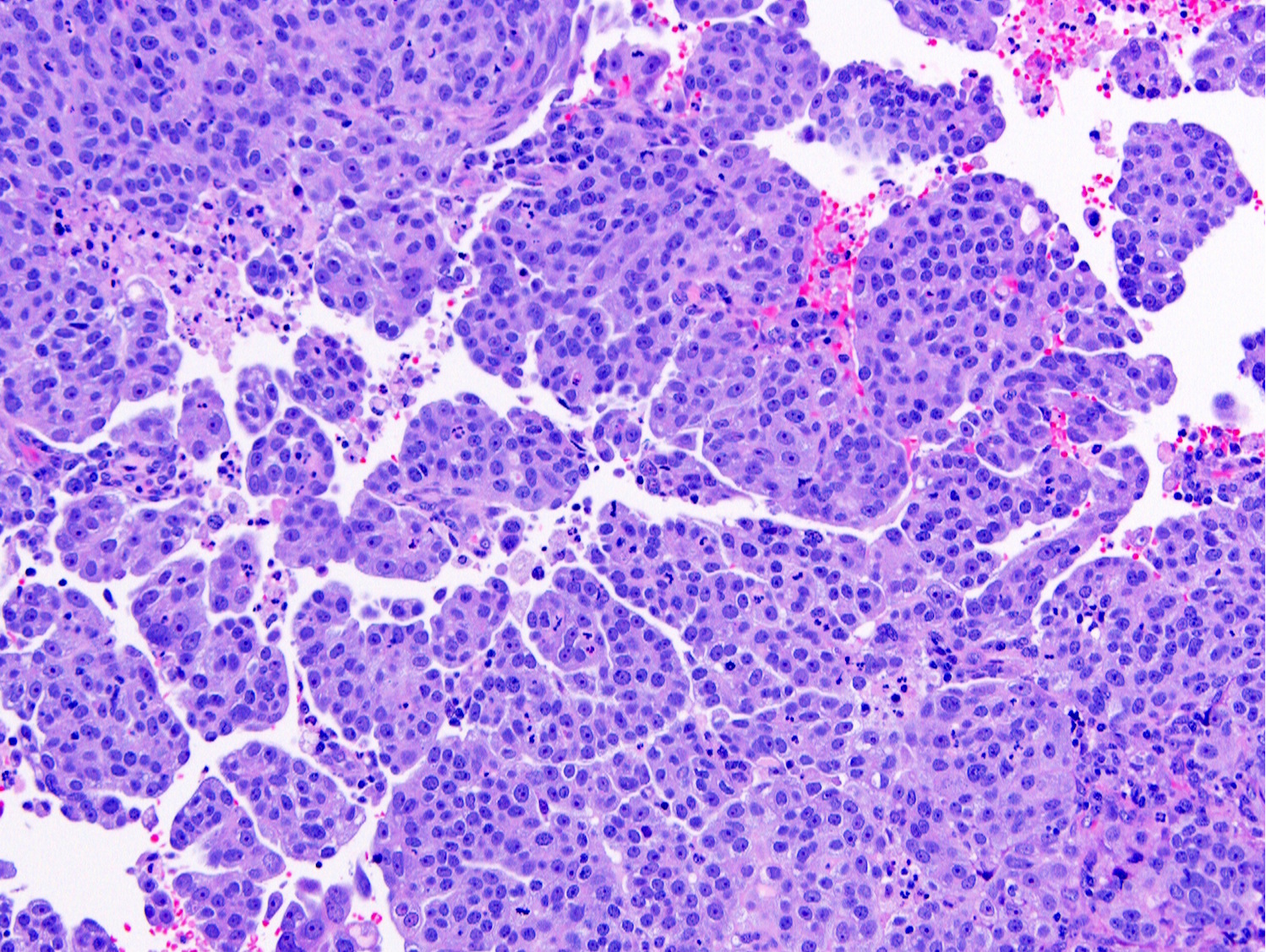
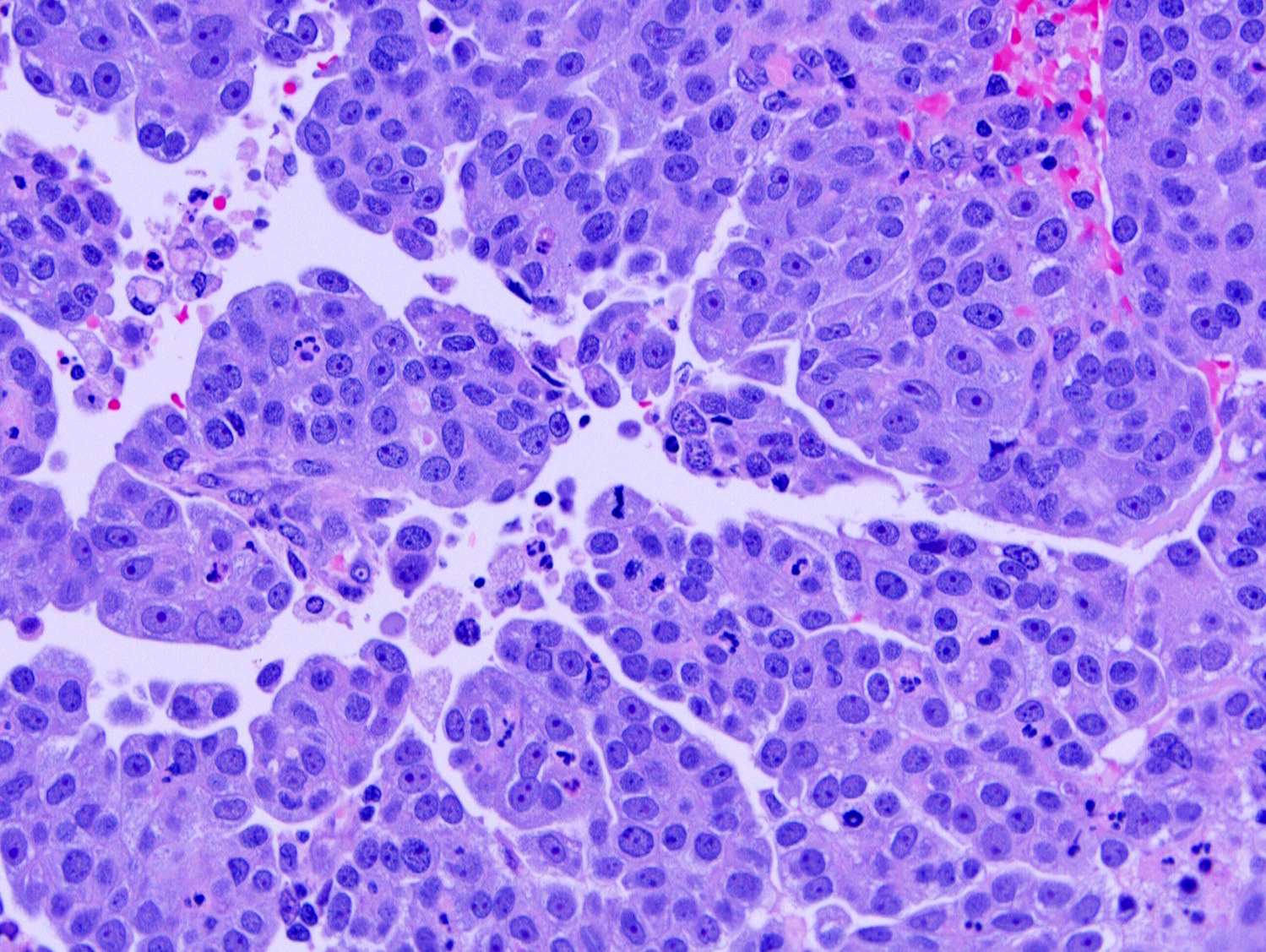
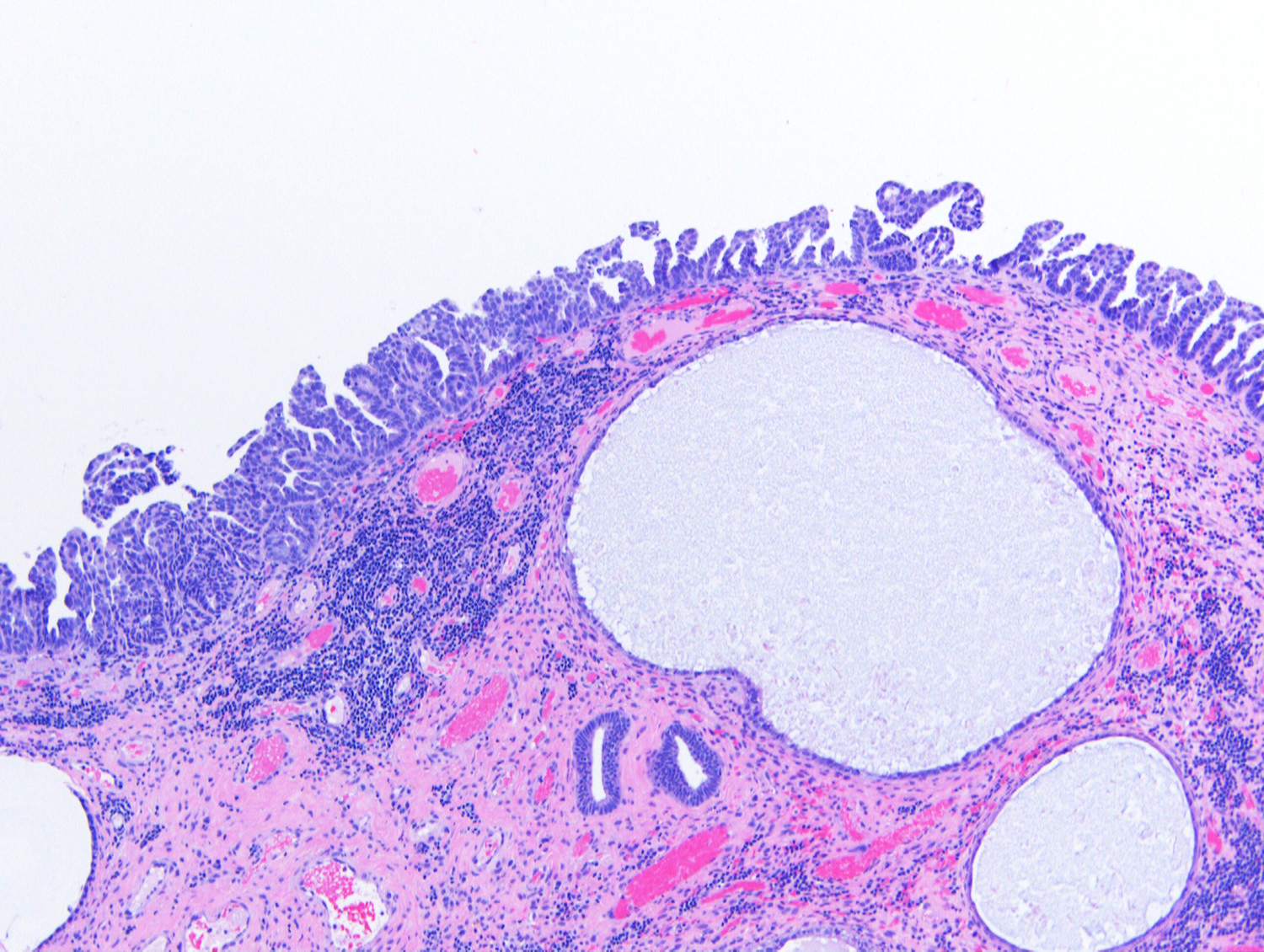
Microscopic (histologic) description
- Architecture:
- Papillary with or without appreciable fibrovascular cores; micropapillary pattern can be seen
- Slit-like spaces
- Gland-like spaces may be observed (but luminal borders are not sharp as seen in endometrioid carcinoma)
- Solid growth
- Psammoma bodies may be present in up to 33% of cases
- Cytoplasm usually scant but can be abundant with eosinophilia or clearing
- Tumor cells can colonize existing endometrial glands
- Tumor cells can appear discohesive
- Nuclei are typically high grade with pleomorphism, hyperchromasia, prominent nucleoli and frequent mitotic figures (including atypical mitotic figures)
- Can be confined to an endometrial polyp as a small surface proliferation or completely effacing the polyp
- Background endometrium, if present, is often atrophic
- Not graded into low and high grade as done in the ovary but by default is a high grade carcinoma
- Select references / reviews: Adv Anat Pathol 2011;18:415, Adv Anat Pathol 2004;11:117
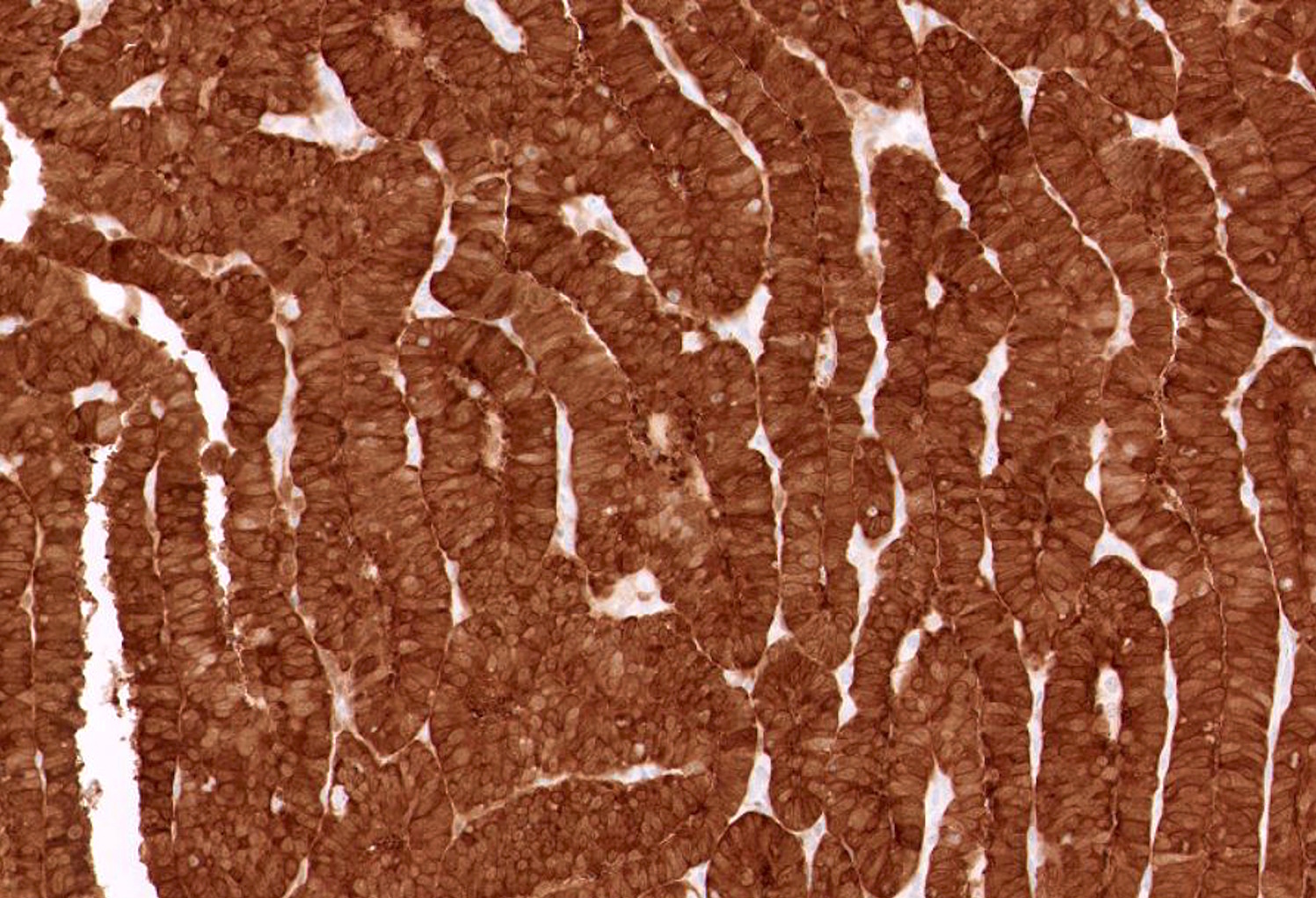
Microscopic (histologic) images
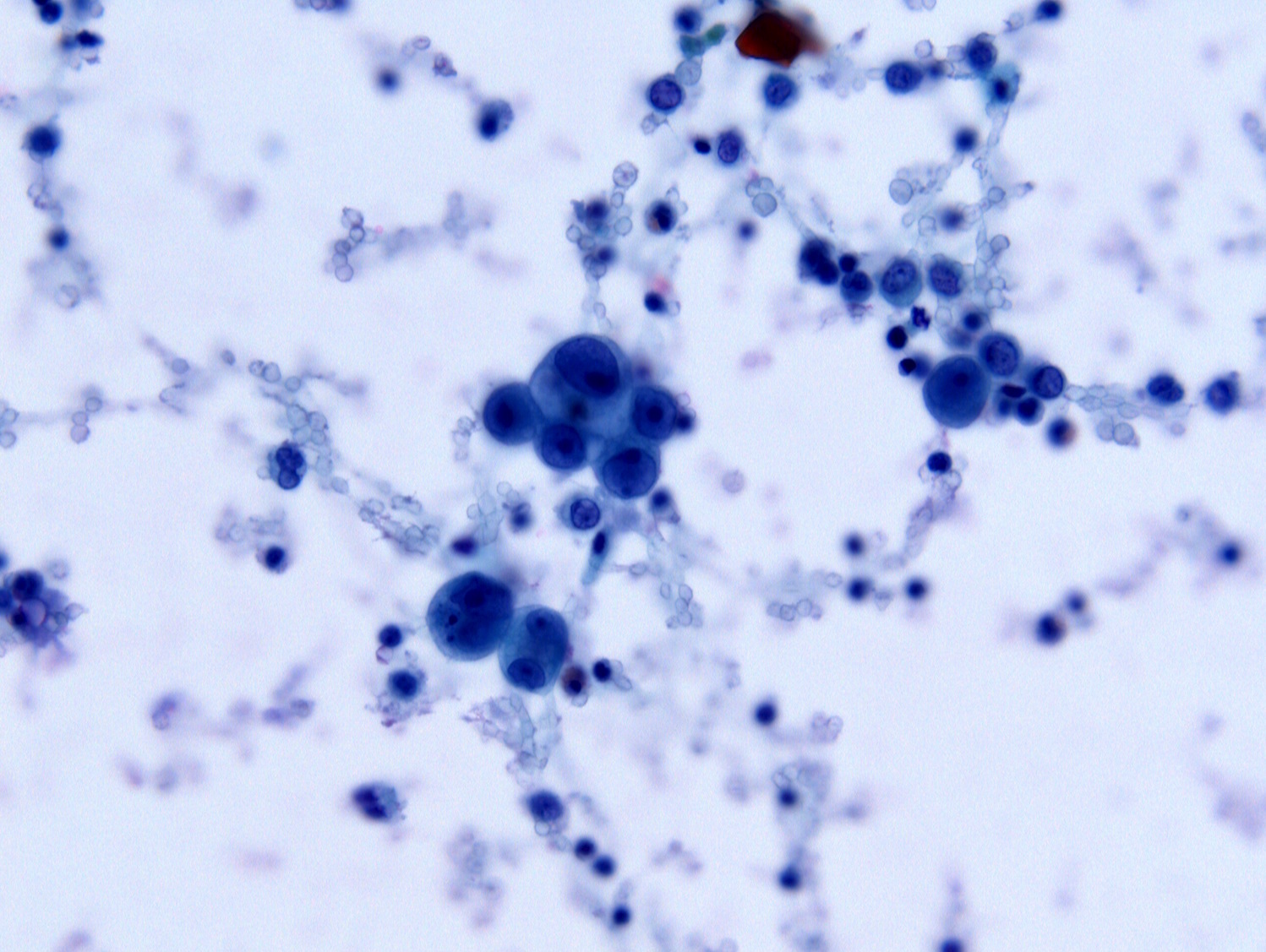
Cytology description
- Cytologic findings are similar to ovarian high grade serous carcinoma
- Tumor cells should look frankly malignant and pleomorphic:
- Nuclear hyperchromasia
- Irregular nuclear contours
- Irregular coarse chromatin
- Prominent cherry-red nucleoli
- Cytoplasmic vacuoles may be present
- Reference: Diagn Cytopathol 2016;44:1039
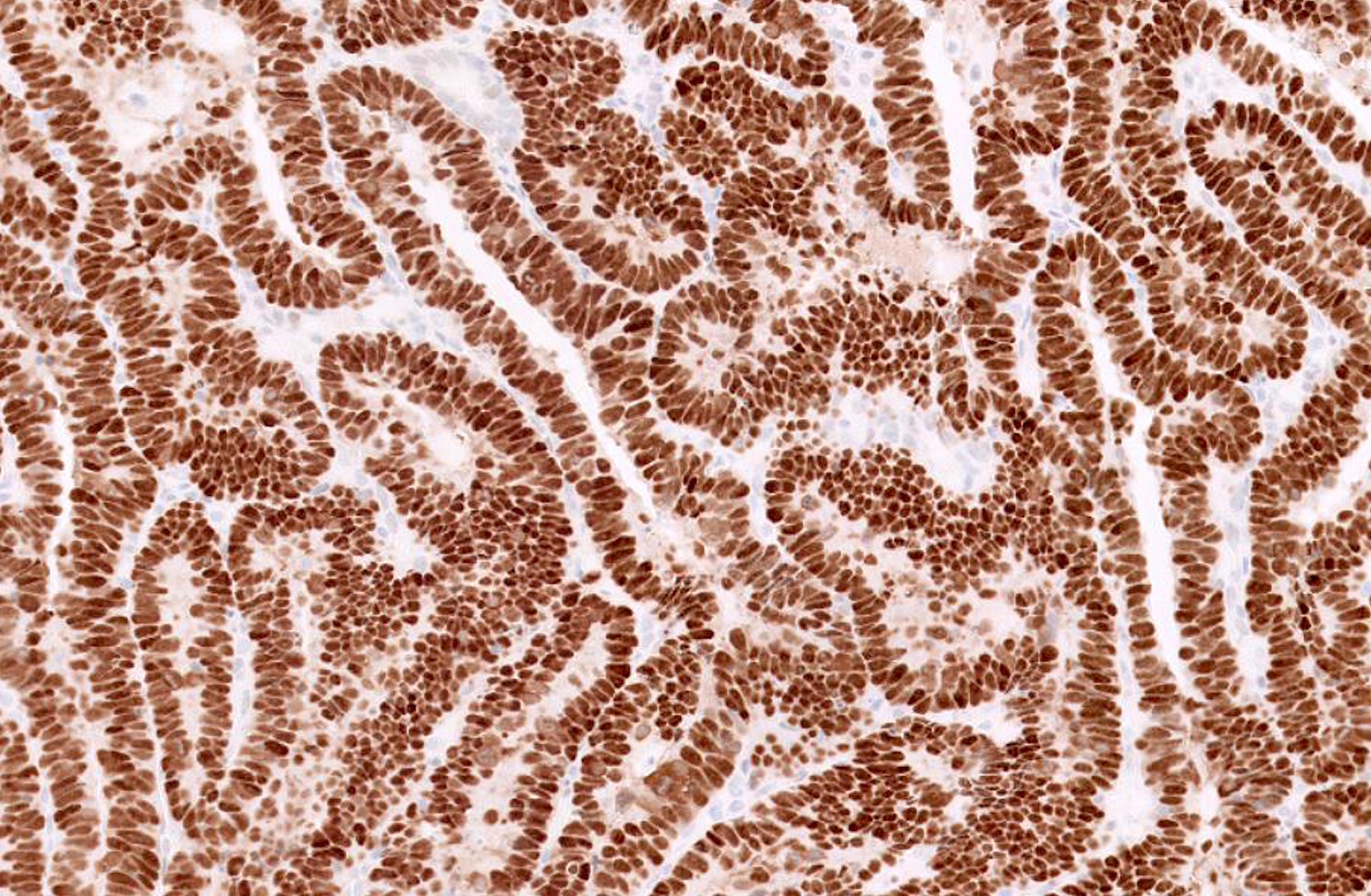
Positive stains
- p53: mutation type staining either strong and diffuse, complete absence of staining (“null type” pattern) or abnormal cytoplasmic localization
- p16: often strong and diffuse (not related to HPV infection)
- AE1 / AE3 and CK7: strong membranous staining
- PAX8: strong nuclear staining
- MLH1, MSH1, MSH2 and MSH6: typically retained but can show loss of at least one marker in 10% of cases (Int J Gynecol Pathol 2019;38 Suppl 1:S40)
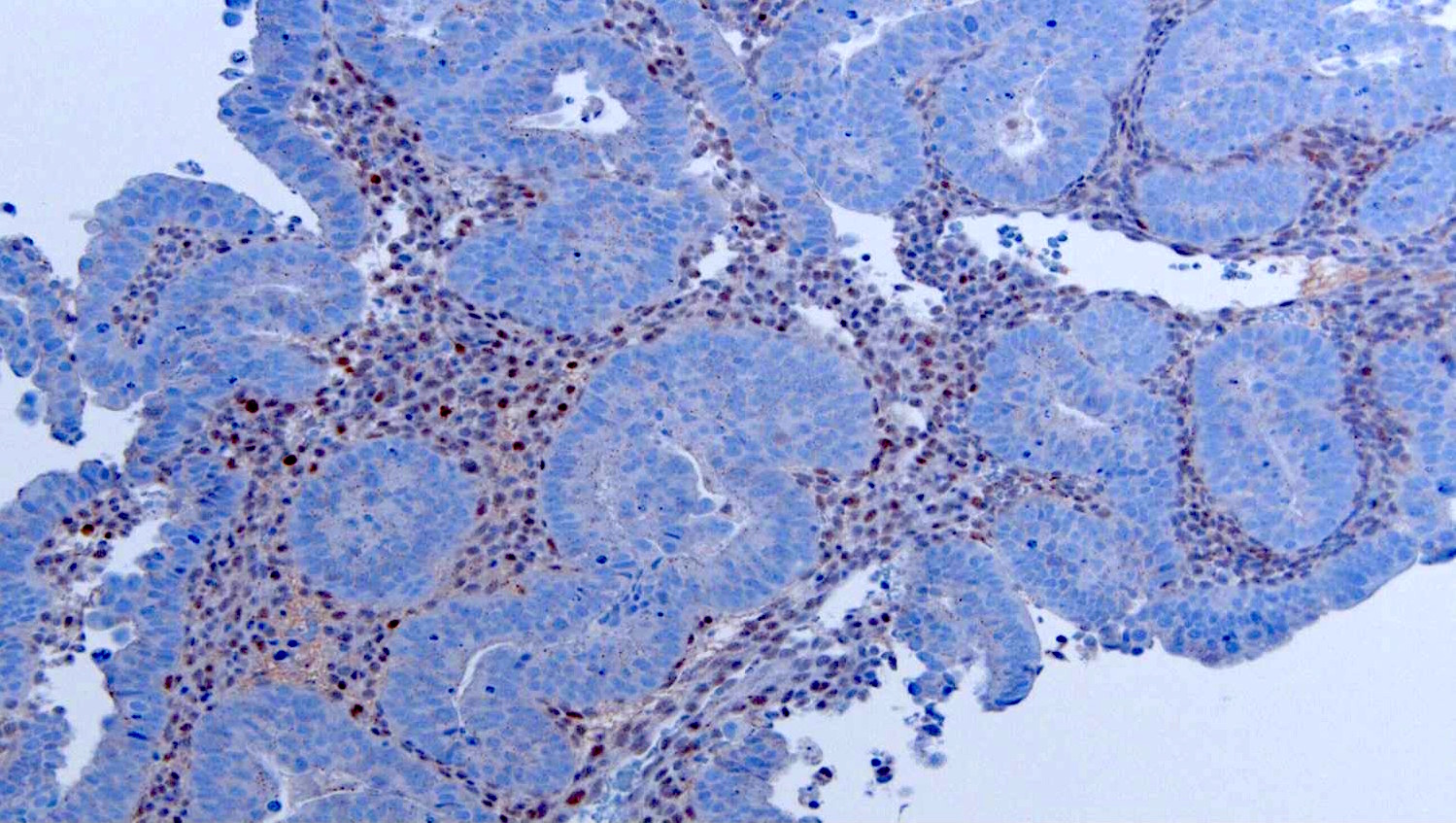
Negative stains
- CK20: no expression
- ER / PR: decreased expression; often negative or focally positive in approximately 50% of cases
- WT-1: maybe focally positive in 30% of cases; if strong and diffuse, extrauterine serous carcinoma enters the differential
- See review: Int J Gynecol Pathol 2019;38 Suppl 1:S40
Molecular / cytogenetics description
- Mutations in TP53 (80 - 90%) and PIK3CA (24 - 40%) common
- Mutations in PTEN and ARIDA1A uncommon
- Serous carcinomas show high somatic copy number abnormalities (Nature 2013;497:67)
Sample pathology report
- Endometrial polyps, curettage / polypectomy:
- Endometrial serous carcinoma involving endometrial polyp (see comment)
- Background atrophic endometrium
- Comment: Immunohistochemical stains show that the tumor is positive for p53 (strong and diffuse, mutated) and p16 (strong and diffuse), focally positive for ER and negative for PR. This immunoprofile supports the above diagnosis.
- Uterus, hysterectomy:
- Endometrial serous carcinoma (0.8 cm) with superficial myometrial invasion (see synoptic report and comment)
- Comment: Immunohistochemical stains show that the tumor is positive for p16 (strong and diffuse), focally positive for ER and PR and has no expression for p53 (null mutation). This immunoprofile supports the above diagnosis.
Differential diagnosis
- Endometrial endometrioid adenocarcinoma
- Most important differential is villoglandular pattern
- Areas with well developed, readily identifiable glands with sharp luminal borders should be present
- Squamous or mucinous metaplasia often seen in endometrioid carcinomas (and not present in serous carcinomas)
- Cytologically bland in comparison to serous carcinoma
- ER / PR strongly positive
- p53 and p16 weak and patchy
- Endometrial clear cell adenocarcinoma
- Typical papillary, tubulocystic and solid architecture
- Papillae are typically small with hyalinized cores lined by a single layer of polygonal hobnailed cells
- Uniform nuclear atypia but overt nuclear pleomorphism at a lesser degree than what can be seen in serous and high grade endometrioid carcinoma
- Clear to eosinophilic (oxyphilic) cytoplasm; often shows prominent nucleoli
- More likely to be positive for HNF-1β and Napsin A
- Mixed carcinoma
- Defined by WHO as a tumor composed of at least two components (with each component encompassing at least 10% of the tumor volume), with one of the two components being high grade
- Endometrioid adenocarcinoma and serous carcinoma are the typical tumor types identified
- Secondary involvement of the endometrium by tubo-ovarian carcinoma
- Clinical findings should indicate adnexal mass
- WT-1 often strong and diffuse in extrauterine primary serous carcinoma
- Metaplastic changes
- Morphologic clues can help differentiate
- Cilia present in tubal metaplasia
- Hobnail metaplasia shows only mild nuclear atypia and infrequent mitoses
- Papillary syncytial metaplasia is often associated with endometrial stromal breakdown and often demonstrates neutrophilic microabscesses
- Metaplastic processes, in general, should show low Ki67 proliferation indices and wild type (non-mutated) p53 expression
- Morphologic clues can help differentiate
Board review style question #1
- The carcinoma shown in the image above, which involves the surface of an endometrial polyp, shows strong and diffuse positivity for p53 and p16. Which of the follow is true regarding the above carcinoma?
- Likely arose in a patient less than 30 years of age
- Considered an estrogen dependent endometrial carcinoma
- Even without definitive invasion, can present at high stage with tumor dissemination in the peritoneal cavity
- Often shows monotonous nuclei with little pleomorphism and low proliferation index
Board review style answer #1
C. This is a serous endometrial intraepithelial carcinoma in an endometrial polyp. Even without definitive invasion, can present at high stage with tumor dissemination in the peritoneal cavity.
Comment Here
Reference: Serous carcinoma
Comment Here
Reference: Serous carcinoma
Board review style question #2
- Which of the following is true regarding serous carcinomas of the endometrium?
- Mutations in p53 are the most common driving molecular event
- WT-1 is often strong and diffusely positive
- Show well formed glands with sharp luminal borders
- p16 overexpression indicates a role for HPV infection in the etiology
Board review style answer #2
A. Mutations in p53 are the most common driving molecular event.
Comment Here
Reference: Serous carcinoma
Comment Here
Reference: Serous carcinoma