Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Haque M, Mneimneh WS. Endometrial polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusendopolyp.html. Accessed December 3rd, 2024.
Definition / general
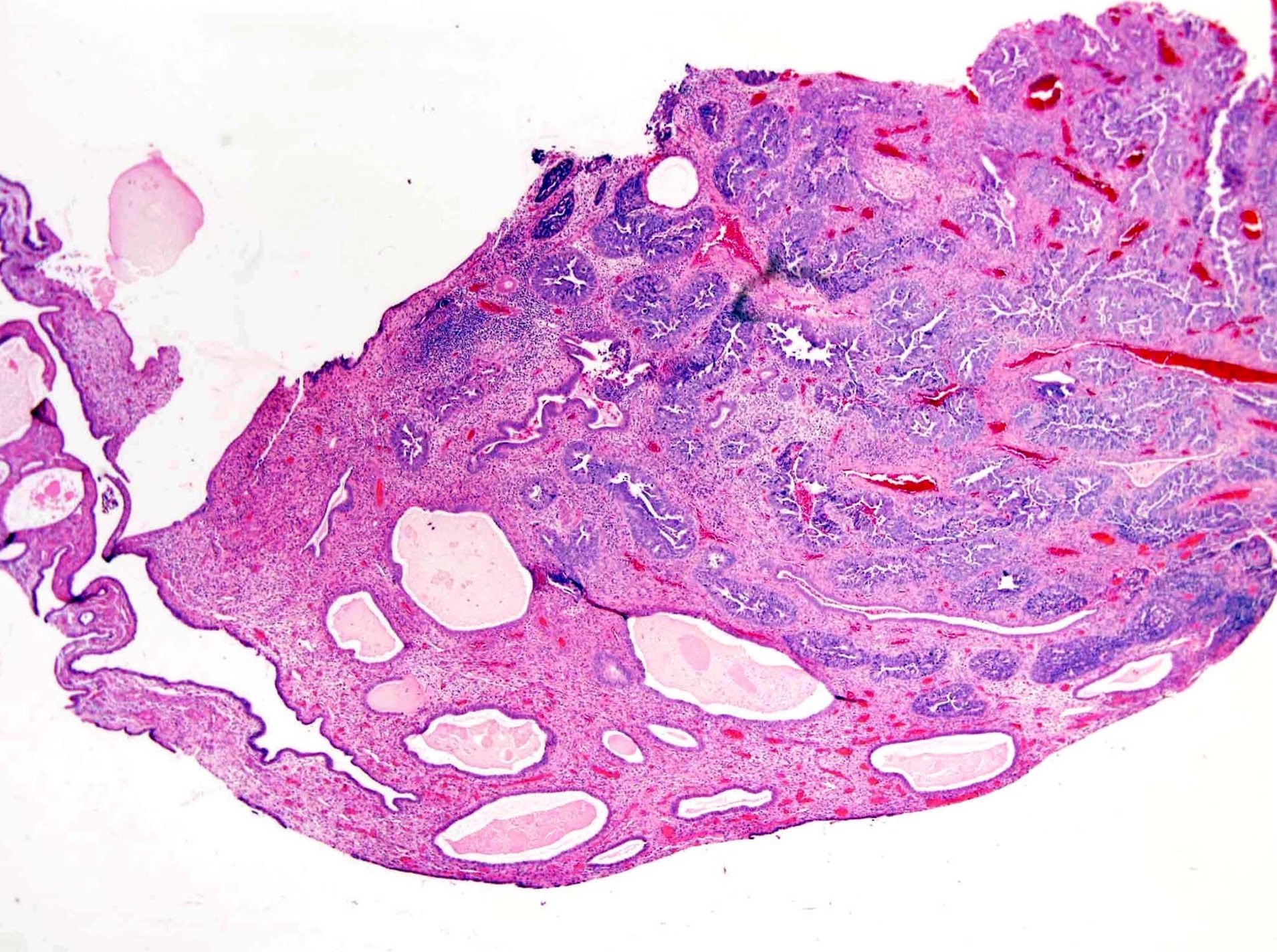
- Benign hyperplastic overgrowth of endometrial tissue that forms a localized projection into the endometrial cavity and is composed of a variable amount of glands and stroma
- Polypoid / pedunculated mass composed of cystically dilated glands with fibrous stroma that contains thick walled blood vessels
- May be related to hyperestrogenism, possibly originating as a localized hyperplasia of the endometrial basalis, secondary to hormonal influences
Essential features
- Polypoid shape, attenuated surface endometrium on 3 sides
- Large, thick walled blood vessels
- Fibrous stroma with spindled fibroblast-like cells, sometimes hyalinized
- Glandular architectural abnormality different from the surrounding endometrium, with cystic change, sometimes glandular crowding
Terminology
- Uterine polyp
ICD coding
- ICD-10: N84.0 - polyp of corpus uteri
Epidemiology
- Can affect up to 25% of females presenting with abnormal uterine bleeding (Case Rep Obstet Gynecol 2014;2014:518398)
- Prevalence in asymptomatic females: 10 - 15%
- Peak incidence in fifth decade
- Incidence in asymptomatic females with infertility: 10 - 32%
- Increased incidence with hormone replacement therapy, either estrogen only or combined preparations (Am J Obstet Gynecol 2011;205:535.e1)
Sites
- Can arise anywhere in the uterine cavity including lower uterine segment
- Most common in the posterior wall of the uterine cavity, followed by anterior, lateral and uterotubal junction (Fertil Steril 2008;90:180)
- Can be multiple
- Rare incidence of endometrial polyps embedded in the fetal membranes have been reported (Int J Gynecol Pathol 2020;39:e13)
Etiology
- Thought to represent a hyperplastic response of normal endometrial tissue, possibly originating as a localized hyperplasia of the endometrial basalis, secondary to unopposed estrogen
- Monoclonal stromal overgrowth with secondary induction of polyclonal benign glands
- Overexpression of endometrial aromatase suggests a role of this enzyme in pathogenesis
- Associated with tamoxifen therapy (Am J Obstet Gynecol 2011;205:535.e1)
- Long term consumption of phytoestrogens, produced by plants and found in abundance in spice, herbs and food, can lead to endometrial polyps (Cureus 2021;13:e12789)
- Late menopause, hormone replacement therapy and obesity all increase risk (Maturitas 2005;50:231)
- In postmenopausal females, the presence of metabolic syndrome is a predictor (Menopause 2016;23:759)
Clinical features
- Small polyps are usually asymptomatic
- Larger polyps are associated with abnormal vaginal bleeding in 13 - 50% of cases and occasionally infertility
- Rarely, giant polyps may fill the uterine cavity and extend into the endocervical canal
- Generally unresponsive to progesterone stimulation
- Polyps associated with tamoxifen therapy for breast cancer are characteristically multiple, large and fibrotic (J Cases Obstet Gynecol 2017;4:55)
- Most polyps persist if left untreated; however, a small percentage may spontaneously regress (Best Pract Res Clin Obstet Gynaecol 2017;40:89)
Diagnosis
- Transvaginal pelvic ultrasonography is the imaging modality of choice in women of fertile age (Eur J Obstet Gynecol Reprod Biol 2021;260:70)
- Saline infusion sonohysterography is accurate in asymptomatic postmenopausal females (Eur J Obstet Gynecol Reprod Biol 2021;260:70)
- Hysteroscopy
- Confirmation by histopathology of the resected specimen
- Blind dilatation and curettage should be avoided due to inaccuracy for the diagnosis
Prognostic factors
- Prevalence of endometrial hyperplasia without atypia is 0.2 - 24%
- Prevalence of atypical endometrial hyperplasia is 1 - 3%
- Risk of malignancy is 1 - 3% (Case Rep Obstet Gynecol 2014;2014:518398)
- Risk factors for malignancy: increasing age, obesity, hypertension, postmenopausal status, diabetes, large size of polyps and tamoxifen therapy (Am J Obstet Gynecol 2006;194:718, Am J Obstet Gynecol 2009;201:462.e1, Eur J Obstet Gynecol Reprod Biol 2004;115:206, Lancet 1971;1:413)
- Serous adenocarcinoma, clear cell adenocarcinoma or endometrial intraepithelial neoplasia can occur in the polyp
- Endometrial polyp with atypical stromal cells appears to be indolent with no recurrences or progression to malignancy reported, even in cases treated only with curettage / polypectomy
Case reports
- 28 year old woman with intravascular large B cell lymphoma in a benign appearing endometrial polyp (Blood 2019;133:1920)
- 37 year old woman with endometrial polyp of the placental fetal membranes (Int J Gynecol Pathol 2020;39:e13)
- 57 year old woman with synchronous endometrial adenocarcinoma and carcinosarcoma in endometrial polyp (SAGE Open Med Case Rep 2018;6:2050313X18777164)
- 66 and 70 year old women with intermittent vaginal spotting (Case Rep Obstet Gynecol 2018;2018:8753463)
- 67 year old postmenopausal woman with giant endometrial polyp (Cureus 2021;13:e12789)
Treatment
- Premenopausal: polypectomy for symptomatic polyps, multiple polyps, polyps > 1.5 cm, prolapsed polyps or those associated with infertility
- Postmenopausal: polypectomy or hysterectomy (Eur J Obstet Gynecol Reprod Biol 2021;260:70)
- Hysteroscopic removal or morcellation (Gynecol Obstet Fertil 2015;43:104)
- Excision is curative if the circumscribed foci of endometrial hyperplasia are in polyp with no background hyperplasia
Gross description
- Usually solitary; multiple polyps seen in 10 - 20% of cases
- Size: 0.3 - 12 cm (Clement: Atlas of Gynecologic Surgical Pathology, 3rd Edition, 2014)
- Smooth bosselated surface
- May be sessile or broad based, pedunculated or attached to the endometrium by slender stalk (Kurman: Blaustein's Pathology of the Female Genital Tract, 6th Edition, 2011)
- Soft and cystic or firm and fibrous cut section; multicystic cut surface may be present
Gross images
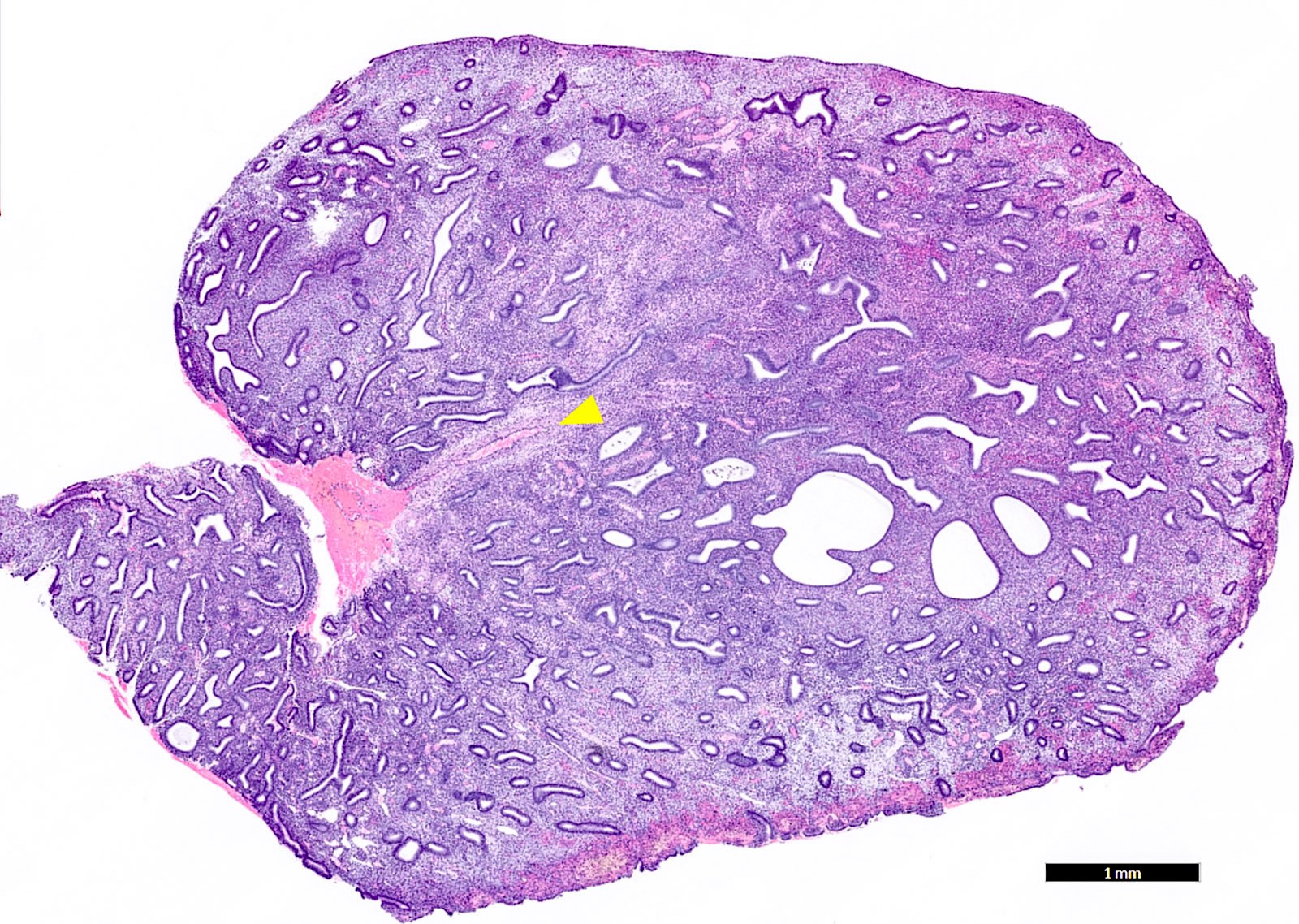
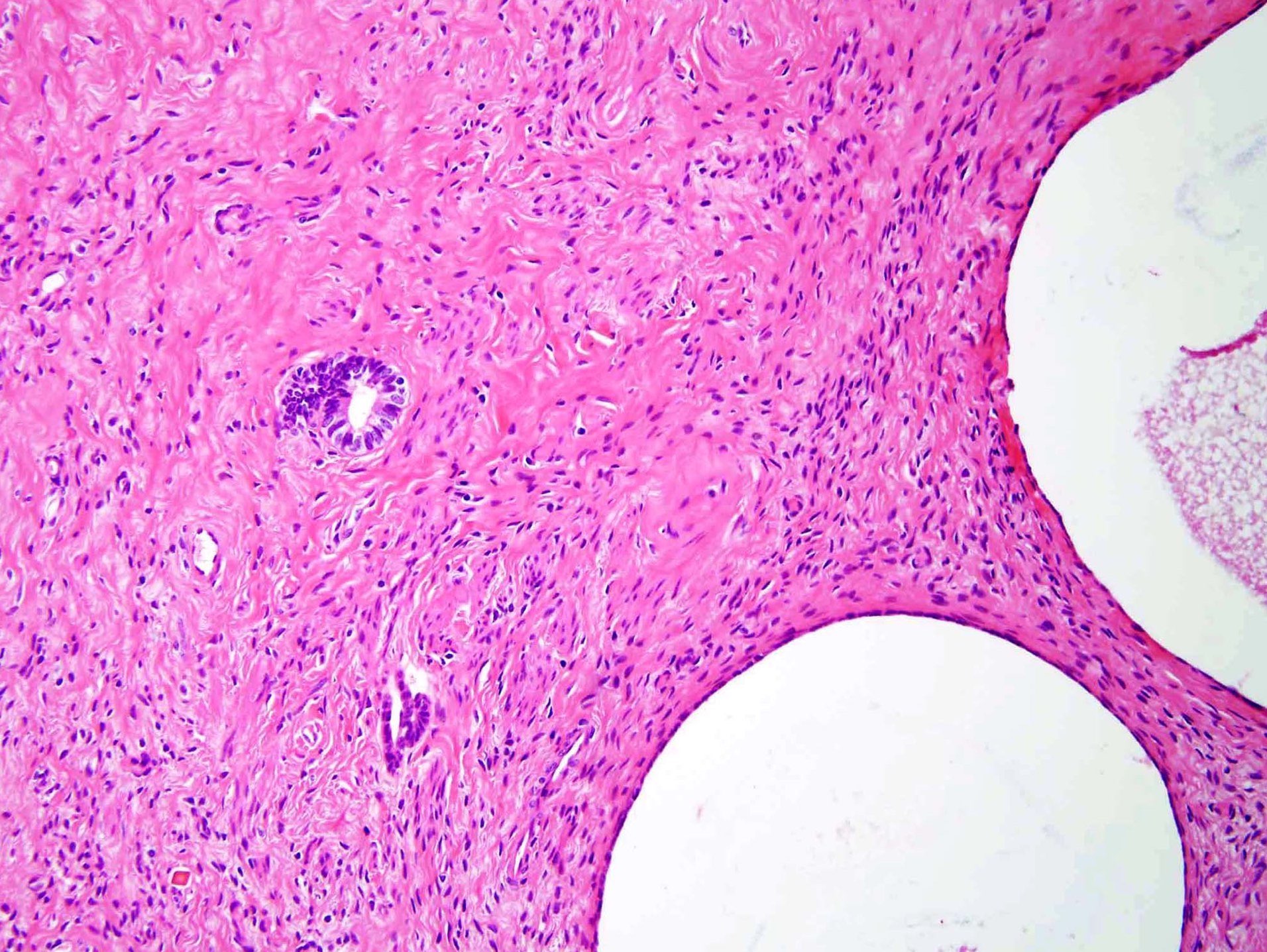
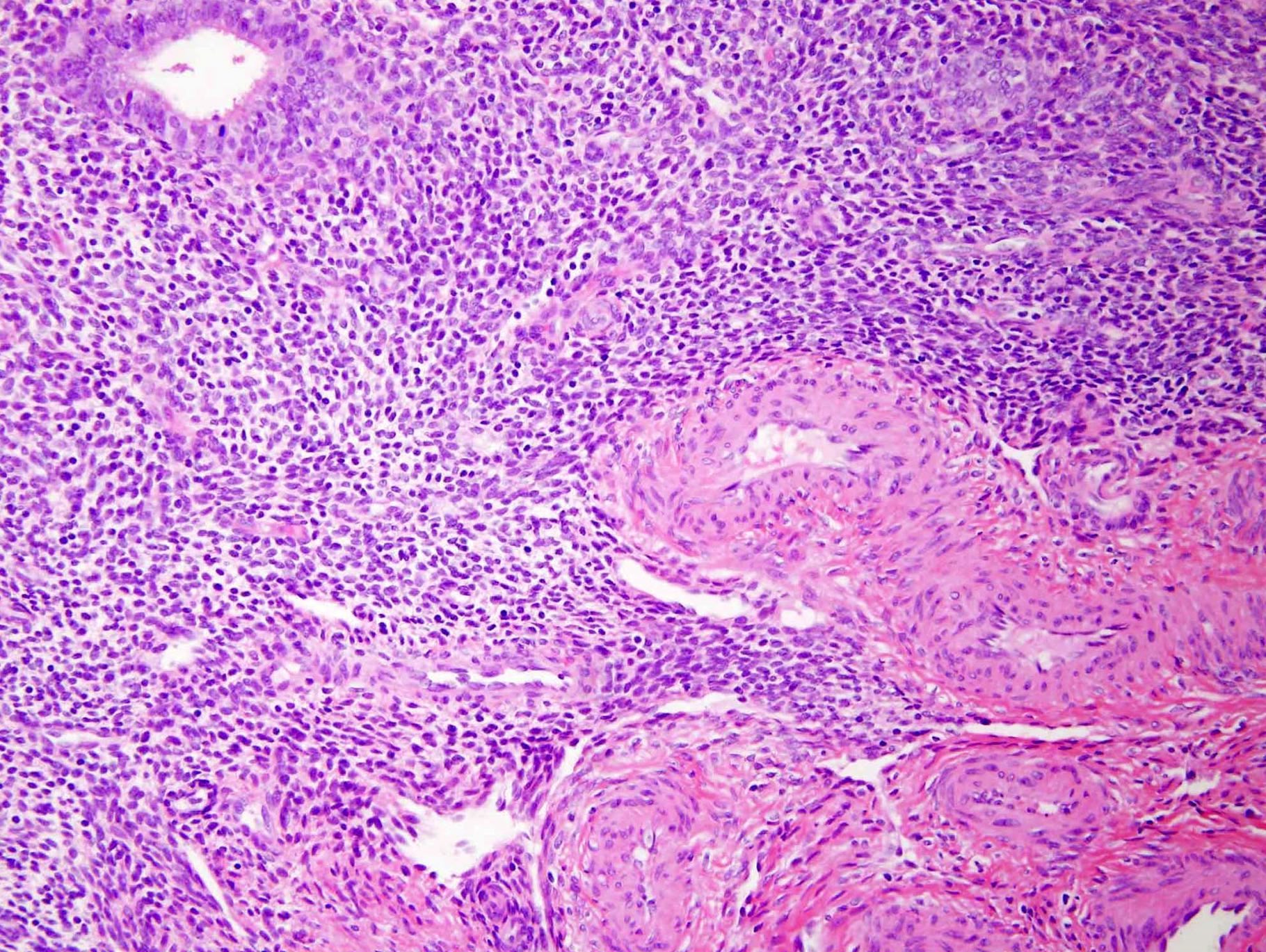
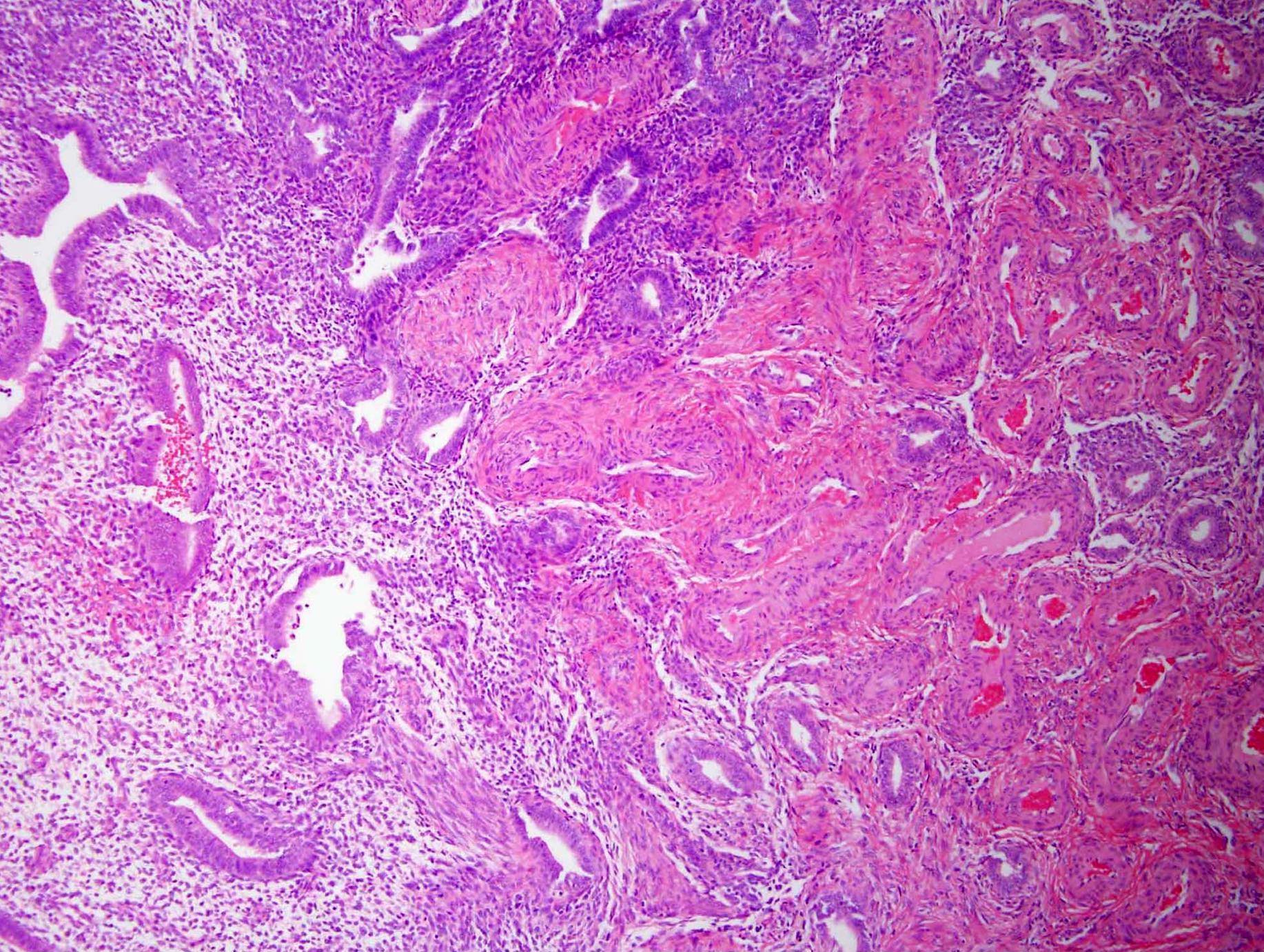
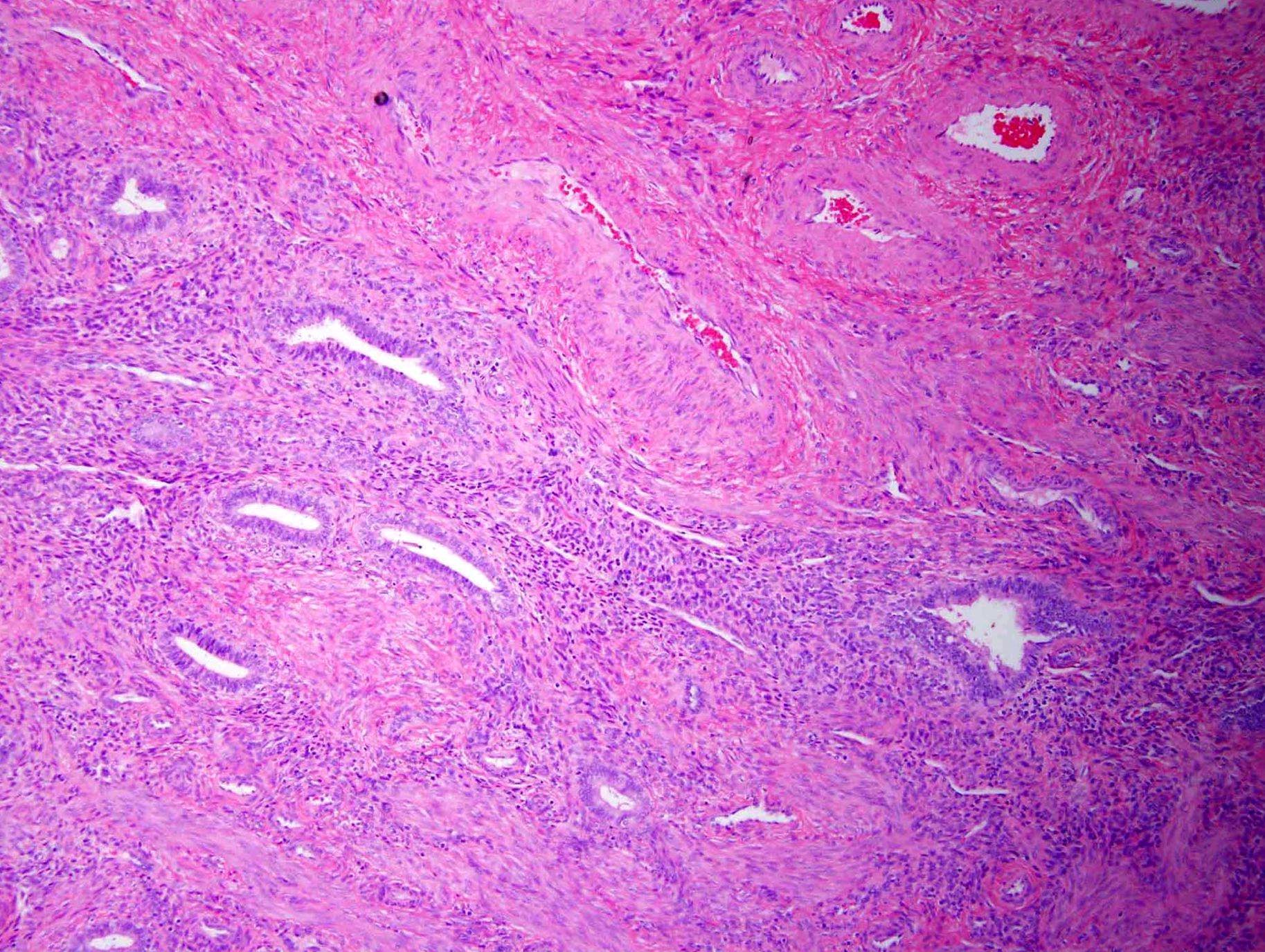
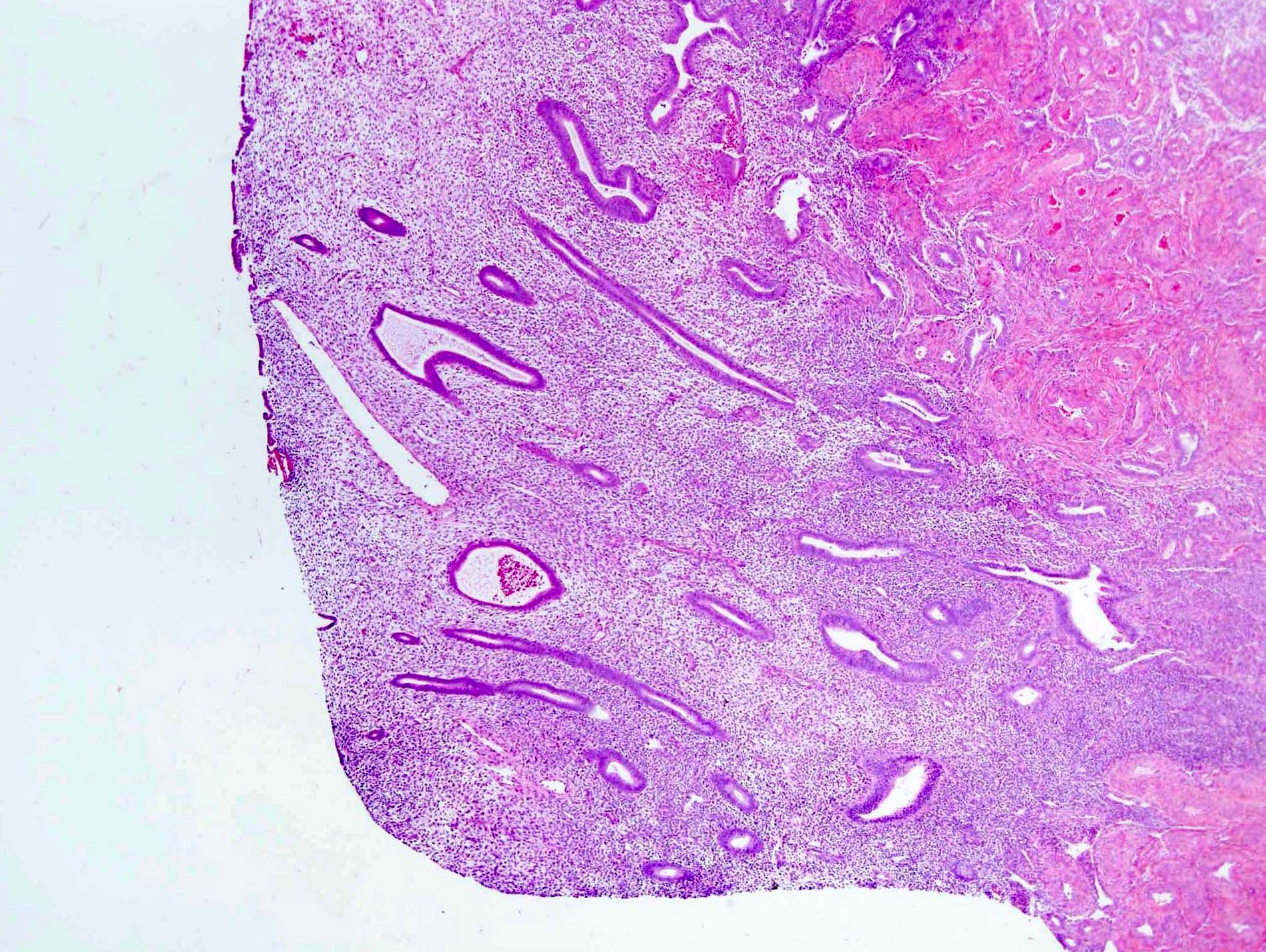
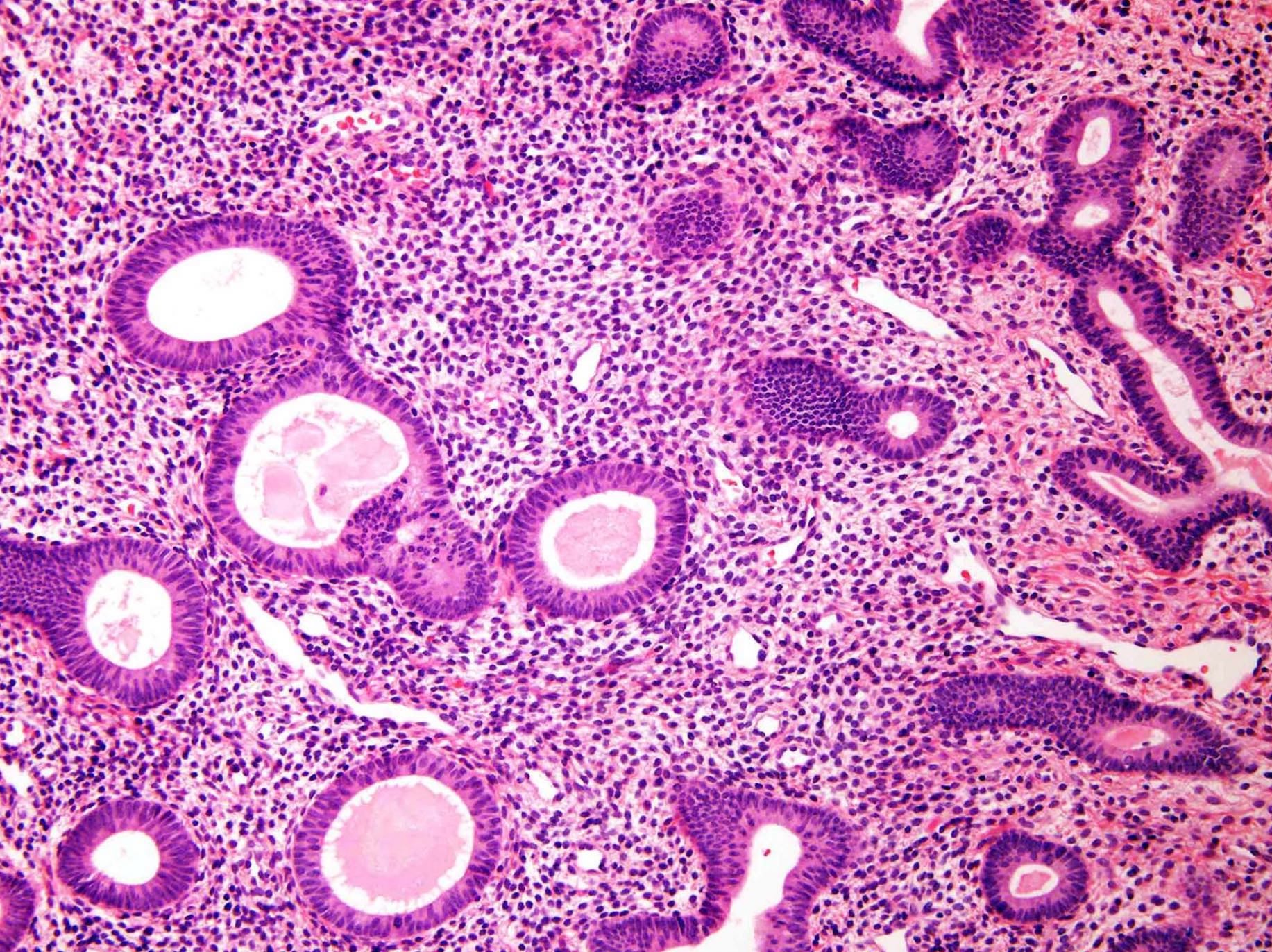
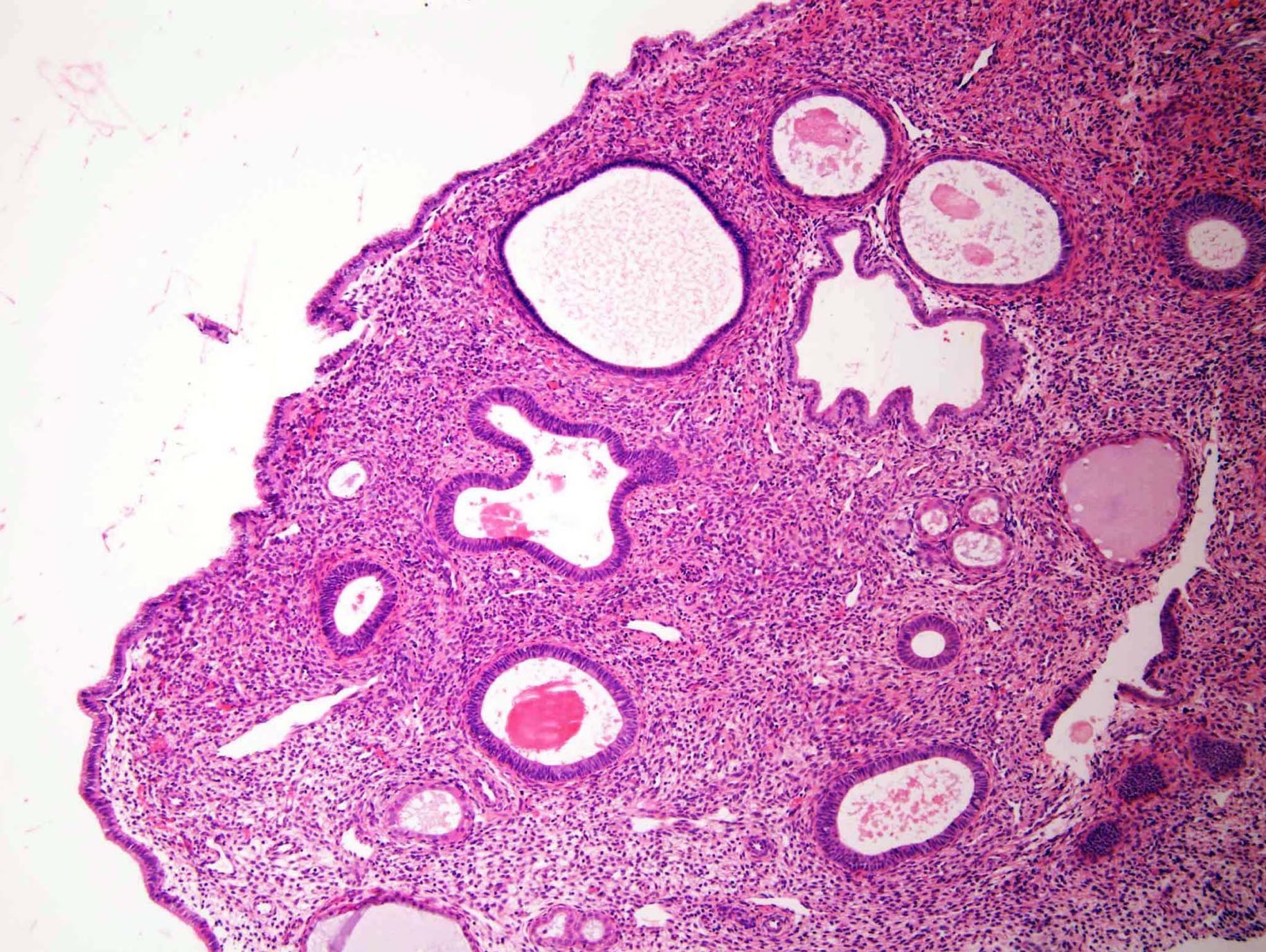
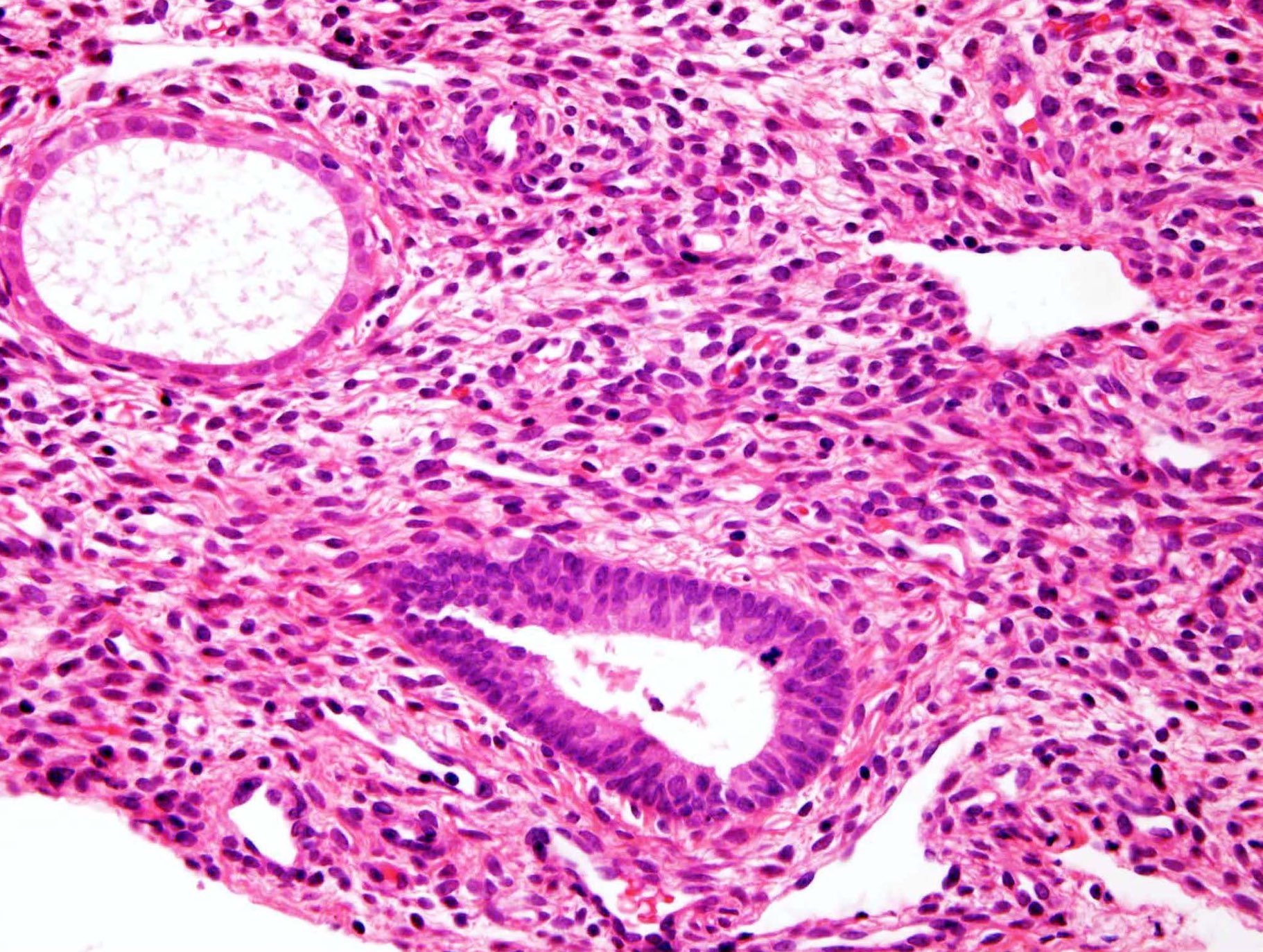
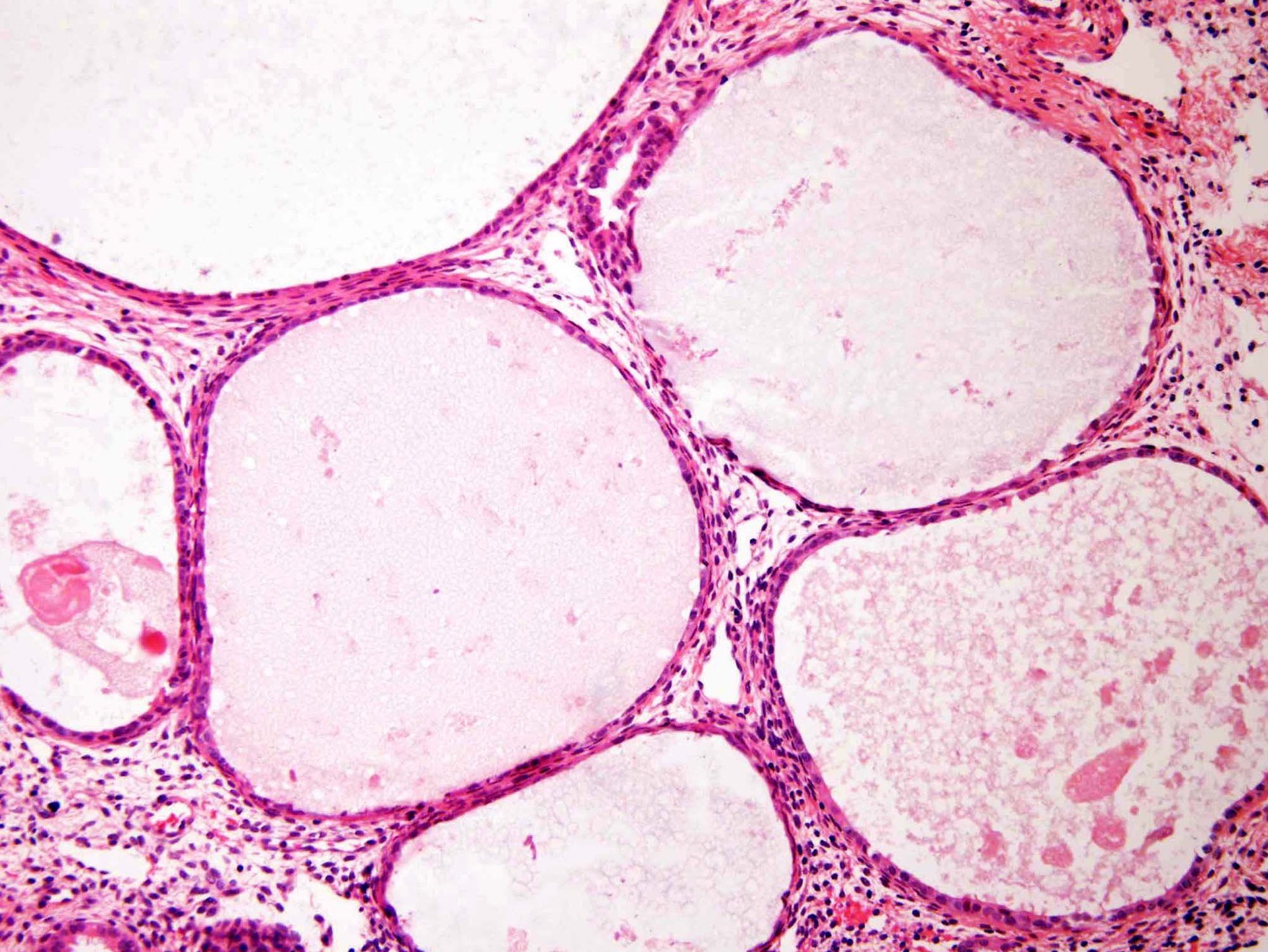
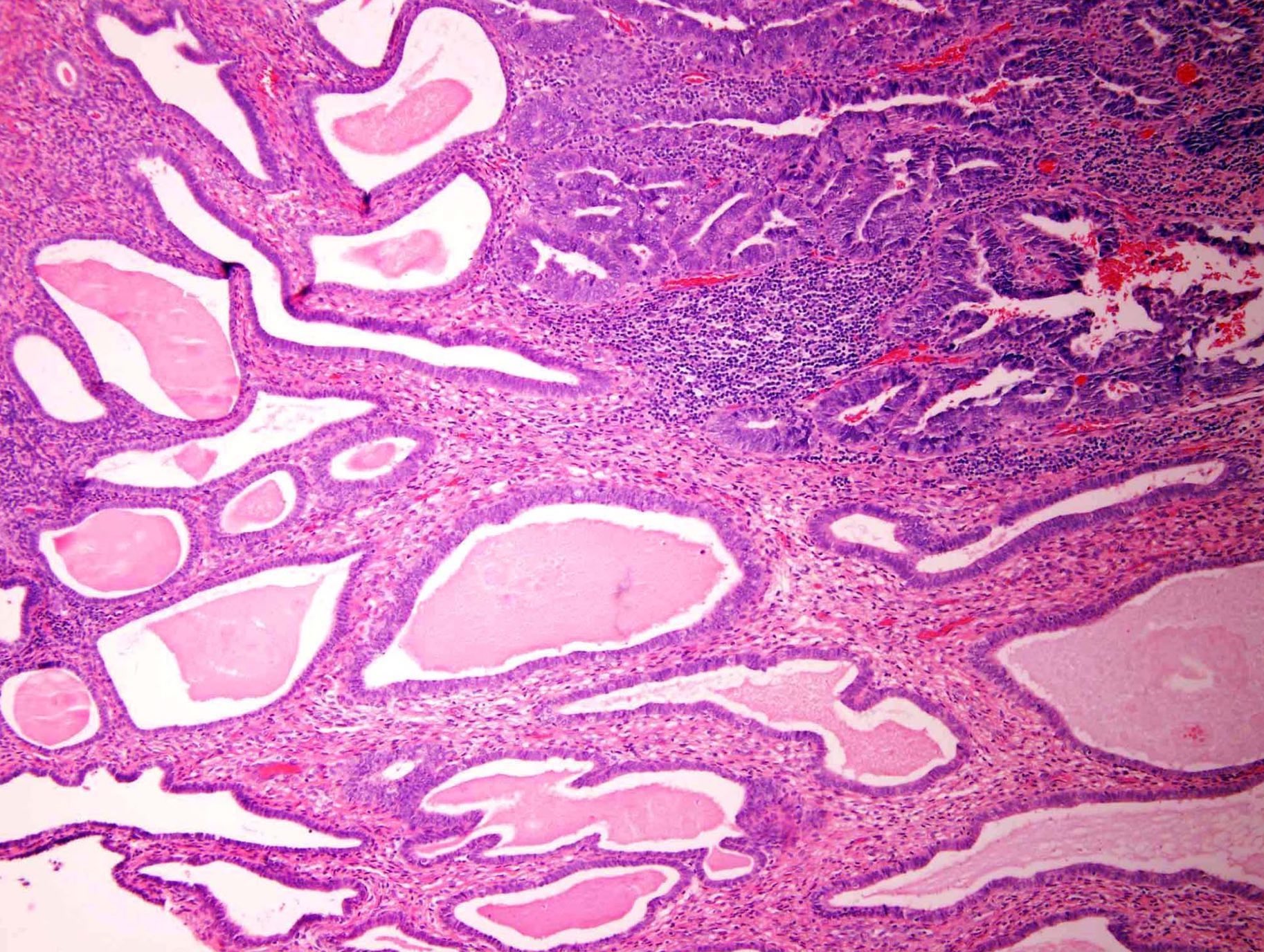
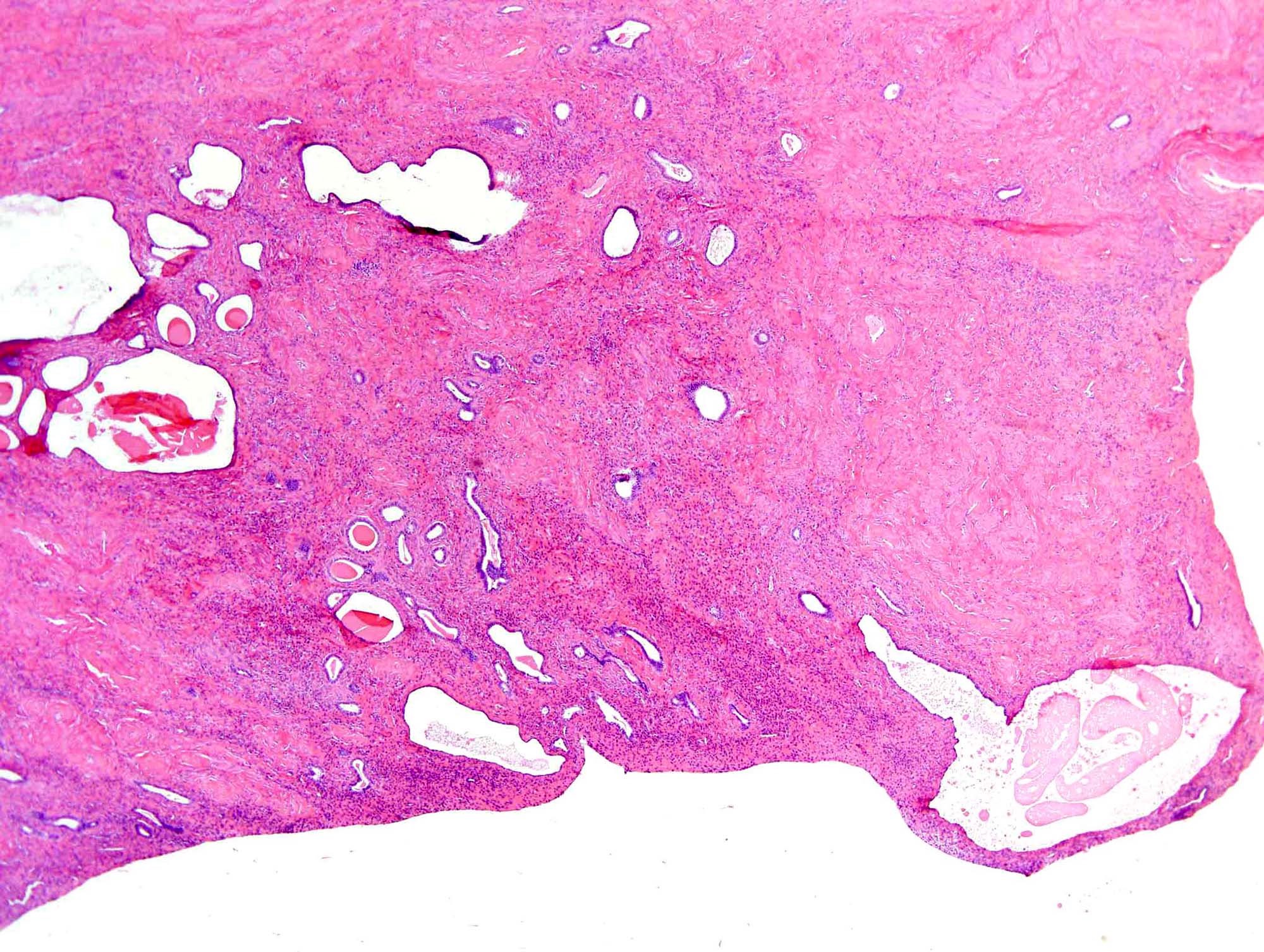
Microscopic (histologic) description
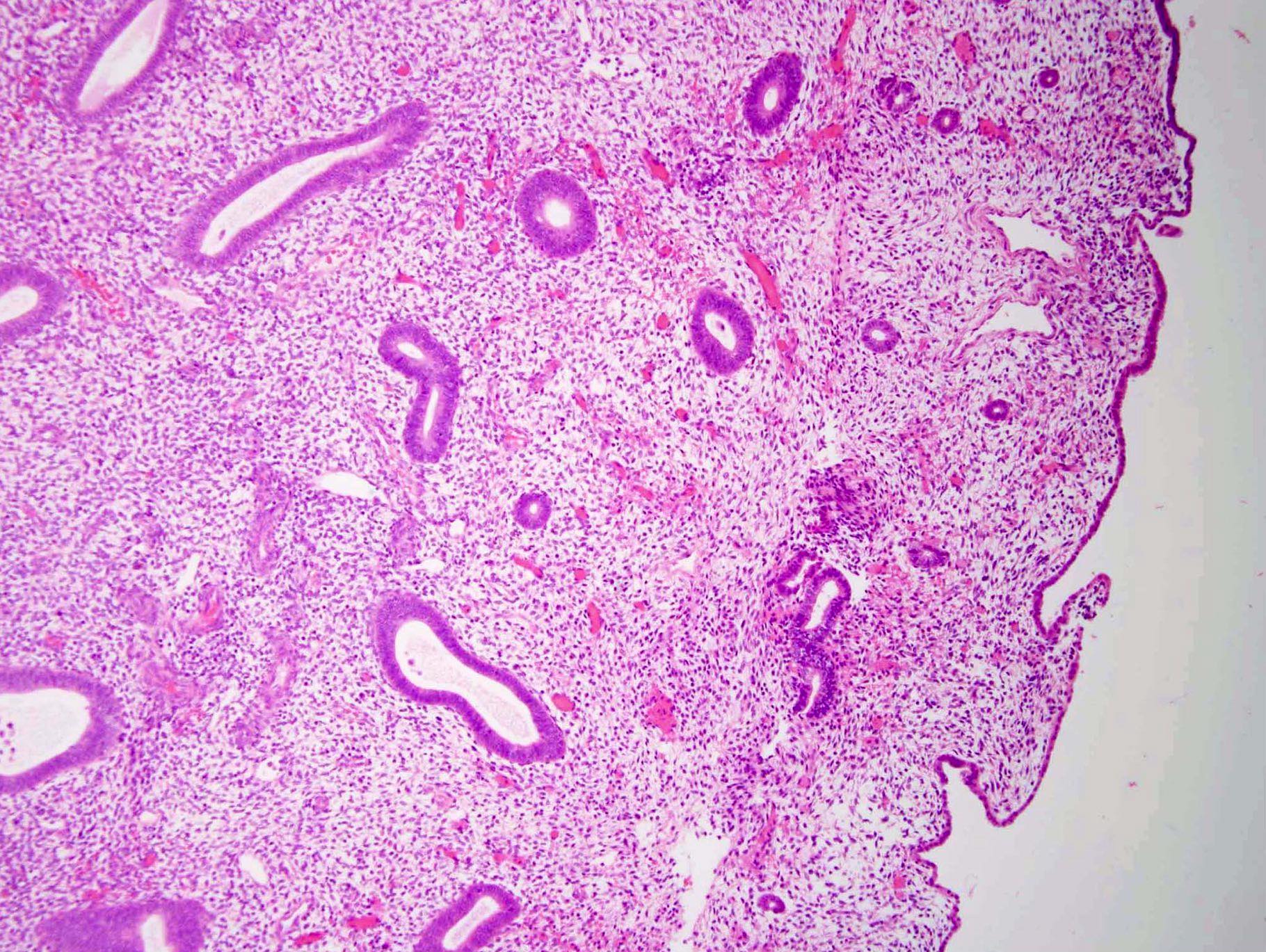
- Polypoid fragments of endometrial tissue lined by epithelium on 3 sides
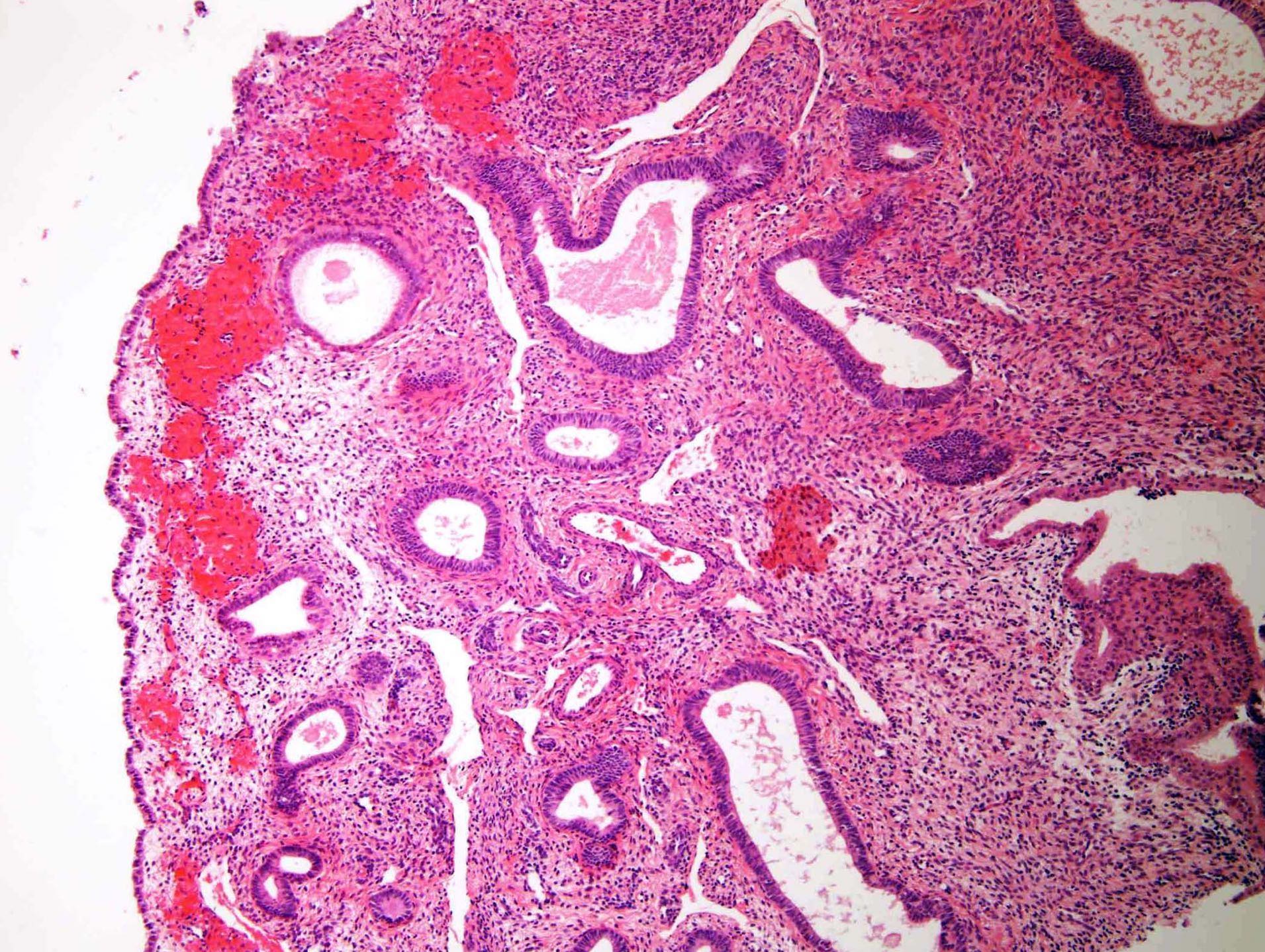
- Surface epithelium:
- May be atrophic but often is proliferative even in postmenopausal women
- Papillary proliferations with fibrovascular cores occasionally occur on the surface of an endometrial polyp or within cystically dilated glands
- May exhibit a degree of atypia, often with degenerated appearing nuclei and sometimes, hobnail cell change
- Reactive surface changes can be seen, including breakdown (shedding) and hemorrhage
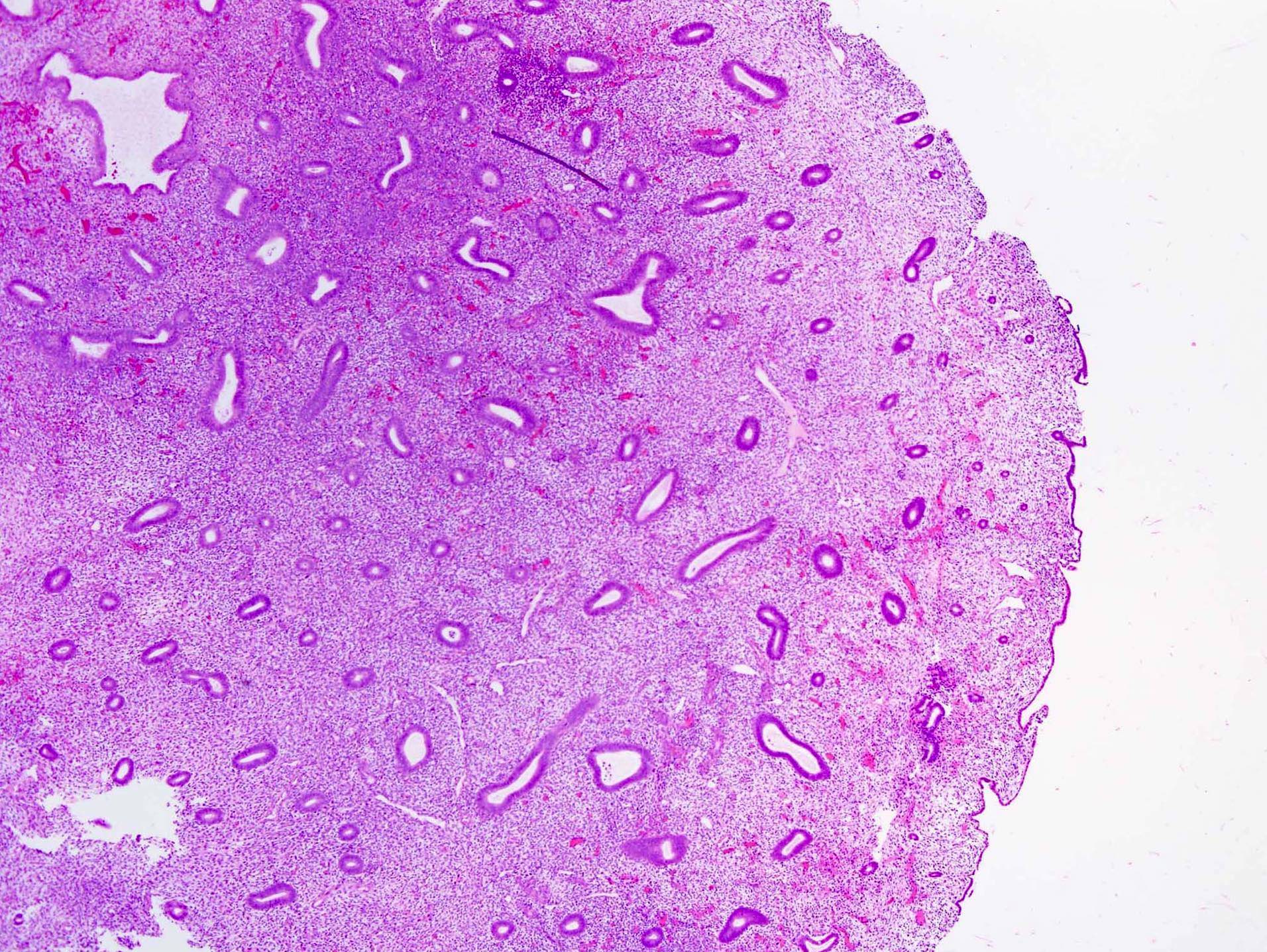
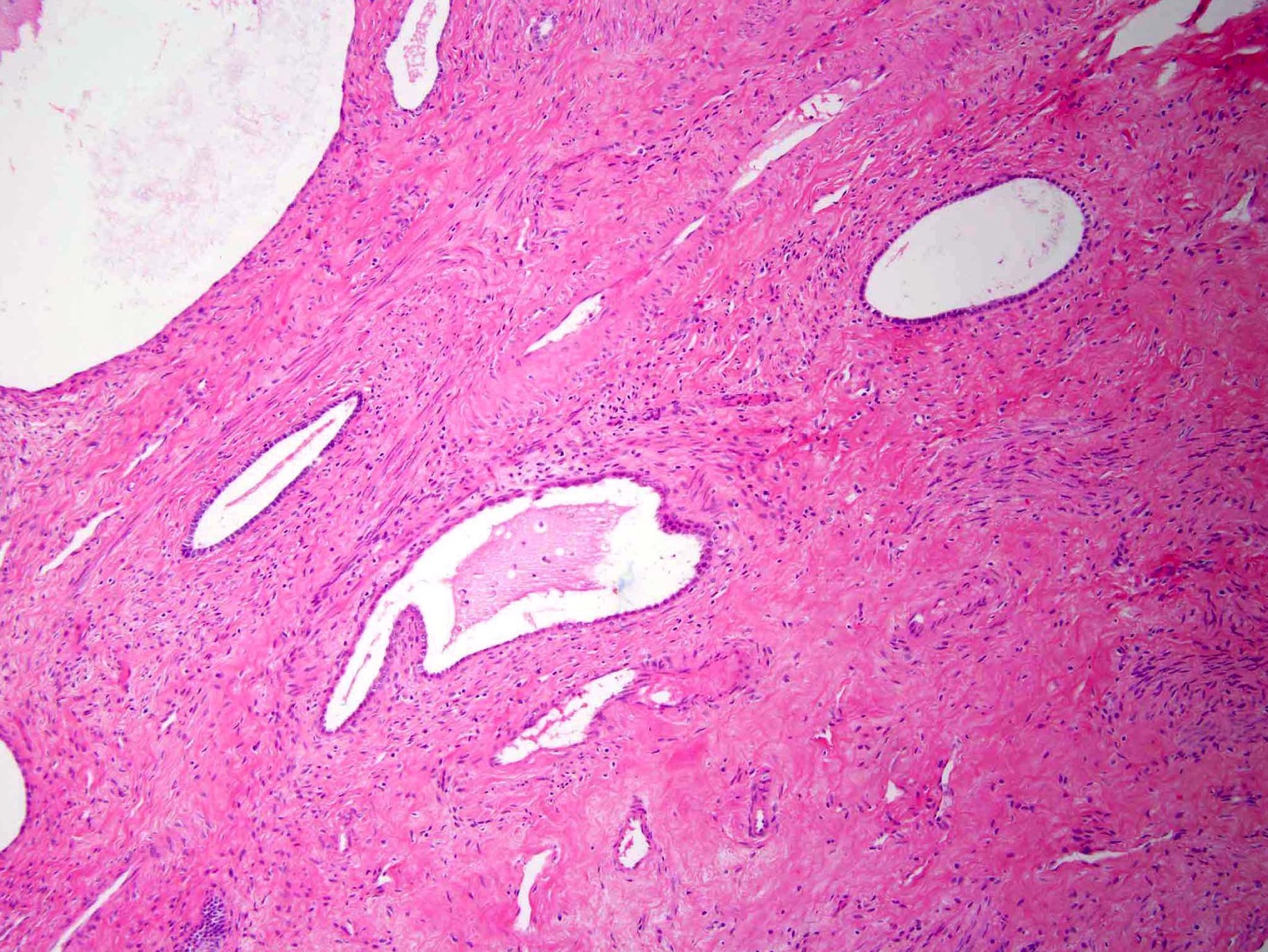
- Stroma:
- Fibrous stroma, rich in collagen with abundant extracellular connective tissue
- Can contain a variable amount of edema, occasional myxoid change and hemosiderin pigment laden macrophages
- Collections of thick walled blood vessels are common; ectatic thin walled vessels may be seen
- Bundles of smooth muscle within the stroma may be present, often in close proximity to thick walled blood vessels
- More prominent smooth muscle component may be seen (Int J Gynecol Pathol 2000;19:195)
- See also myomatous variant (below) and adenomyoma in the Differential diagnosis
- Foci of decidua may be present (usually reflecting exogenous progestin use or pregnancy)
- Mitotic figures in the stromal cells may be present
- Rarely, sex cord-like areas have been described (Int J Gynecol Pathol 2006;25:170)
- Conventional endometrial, endocervical, or adenomyomatous pedunculated, or sessile lesion with histologic features diagnostic of polyp
- Glands:
- Glandular architecture out of phase with the background endometrium
- Angulated, tubular or cystically dilated
- Usually endometrioid in type: inactive, proliferative or functional
- May exhibit metaplastic changes, including ciliated, eosinophilic, mucinous and squamous metaplasia
- Proliferative activity in a polyp in a postmenopausal woman is of no clinical importance (if present in the nonpolypoid endometrium, it is useful to comment on)
- Polyps originating at the junction of the upper endocervix / lower uterine segment contain both endocervical and ciliated lower uterine segment type glands
- If present, the parallel arrangement of the long axis of the endometrial glands to the surface epithelium is a useful diagnostic finding; this feature is especially helpful in premenopausal women (Am J Surg Pathol 2004;28:1057)
- Tamoxifen associated endometrial polyps:
- Show fibrotic, sparsely cellular stroma, metaplastic glands including mucinous metaplasia, edema, decidualization or myxoid change, periglandular stromal epithelial metaplasia and shedding
- Staghorn shaped glands (dilated glands with stromal projections within their luminal spaces) polarized along the long axis of the polyps and periglandular stromal condensations in the absence of conspicuous mitotic activity have been also reported
- May be multiple and can recur (Int J Gynecol Pathol 1999;18:130, Int Urogynecol J Pelvic Floor Dysfunct 2000;11:120, Int J Gynecol Pathol 1998;17:302, Obstet Gynecol 1992;79:111)
- Extensively necrotic polyps can be seen, secondary to torsion or if polyps outgrow their blood supply; vascular thrombosis and surface atypia may be seen in such cases
- Variants:
- Endometrial polyp with atypical stromal cells:
- Presence of bizarre / atypical stromal cells in endometrial polyps and nonpolypoid endometrium has been documented in case reports and few series (Am J Surg Pathol 2015;39:116)
- Stromal cells show markedly atypical symplastic-like nuclei, resembling those seen elsewhere in the female genital tract (e.g., fibroepithelial stromal polyps of the vulva and vagina) (Int J Surg Pathol 2016;24:320, Am J Surg Pathol 2002;26:505)
- Mitotic figures are absent (useful feature to differentiate from adenosarcoma)
- No prominent nucleoli
- Chromatin distribution is uniform with a smudged appearance (instead of coarse)
- Multinucleate forms may be seen
- Atypical cells are usually focally scattered throughout the polyp, predominantly beneath the surface epithelium or at the base
- Immunohistochemically, the atypical cells express vimentin, estrogen, progesterone and androgen receptors and may express desmin, CD10 and muscle specific actin (Am J Surg Pathol 2002;26:505)
- Atrophic: usually seen in postmenopausal women; low columnar to cuboidal epithelial lining, cystic dilatation of the glands and fibrotic stroma
- Functional: if secretory features are present, they are underdeveloped features compared with the background endometrium
- Myomatous: abundant smooth muscle in the stroma (versus adenomyoma: see Differential diagnosis) (Int J Gynecol Pathol 2000;19:195)
- Mixed polyps or polyp of mixed endometrial endocervical type
- Endometrial polyp with atypical stromal cells:
- Other rare findings include:
- Tuberculosis (Case Rep Obstet Gynecol 2013;2013:176124)
- Placental site trophoblastic tumor (Eur J Gynaecol Oncol 2014;35:87)
- Primary diffuse large B cell lymphoma (Int J Gynecol Pathol 2005;24:347)
- Intravascular large B cell lymphomas (Blood 2019;133:1920)
- Metastatic malignant melanoma (Dermatol Online J 2021;27:13030)
- Sarcoidosis (Int J Surg Pathol 2017;25:246)
- Metastases of various carcinomas developing in endometrial polyps (e.g., cervical carcinoma) or rarer ones (e.g., breast lobular carcinoma or gallbladder adenocarcinoma) (Malays J Pathol 2008;30:125, APMIS 2008;116:538, Int J Gynecol Pathol 2009;28:343)
- Must be carefully examined for foci of endometrial hyperplasia and carcinoma:
- Diagnosis of nonatypical hyperplasia should not be made in a polyp, since proliferative activity with glandular dilatation is a feature
- Atypical hyperplasia:
- Diagnostic features similar to those in nonpolypoid endometrium
- If these are confined to the polyp, it should be specified in the diagnosis (may not require additional therapy)
- However, in women with atypical hyperplasia in polyps, atypical hyperplasia and carcinoma in the background surrounding endometrium is not uncommon (it is useful to comment on if present in the nonpolypoid endometrium) (Int J Gynecol Pathol 2008;27:45, BJOG 2007;114:944)
- Endometrial carcinoma:
- Most commonly serous and endometrioid
- Carcinomas found in polyps (tamoxifen related and unrelated) may be confined to the polyp or be part of a multifocal endometrial hyperplasia
- Stains may be helpful to diagnose serous carcinoma
- Recently, it has been reported that most minimal uterine serous carcinomas arise in an endometrial polyp (Hum Pathol 2021;118:1)
Microscopic (histologic) images
Contributed by Monira Haque, M.D. and Yuri Tachibana, M.D.
Positive stains
- In glands: pankeratin, cytokeratin 7, PAX8, ER, PR
- In stroma: ER, PR, smooth muscle actin (in smooth muscle), p16 (usually periglandular) (Oncotarget 2017;8:4826, Pathology 2015;47:112)
- Increased expression of TGFβ1 and VEGF (Eur J Obstet Gynecol Reprod Biol 2011;159:198)
- Atypical stromal cells: vimentin, ER, PR and androgen receptor and may express desmin, CD10 (38%) and muscle specific actin
- Can express p63, P450 arom and SF1 (Zhonghua Fu Chan Ke Za Zhi 2014;49:604)
Negative stains
- Cytokeratin 20, myogenin, WT1
- p16 in epithelium (except if tubal metaplasia or carcinoma present)
- p53 (wild type only, except if carcinoma present)
Molecular / cytogenetics description
- Clonal translocations involving 6p21-22, 12q13-15 or 7q22 (Cancer Genet Cytogenet 1993;68:32)
- 6p21 aberrations characteristically seen only in the stromal component, whereas the epithelial cells are diploid (Genes Chromosomes Cancer 1992;5:260)
Sample pathology report
- Endometrium, biopsy:
- Fragments of endometrial polyp
- Negative for carcinoma
Differential diagnosis
- Adenomyoma:
- Typically not polypoid
- Contains prominent stromal smooth muscle
- Distinction is somewhat arbitrary, based on the amount of smooth muscle present
- Adenosarcoma:
- Usually, bulky polypoid mass
- Leaf-like or club-like architecture, broad papillae lined by surface epithelium and intraglandular stromal projections and > 3 mitoses/10 high power fields with overall architecture resembling a phyllodes tumor of the breast
- Typically, no cystically dilated glands or thick walled blood vessels
- Stroma is more cellular with increased mitotic activity and a degree of nuclear atypia, especially immediately surrounding the glands
- With multiple recurrent endometrial polyps, adenosarcoma should be suspected since the morphological features may be subtle
- Atypical polypoid adenomyoma:
- Stroma exhibits more extensive smooth muscle differentiation
- More complex glandular architecture
- Often shows extensive squamous morular formation
- Endocervical polyp:
- Dilated glands are endocervical (mucous) in type
- Stroma is edematous, inflamed and usually fibrotic
- Polyps originating at the junction of the upper endocervix and lower uterine segment contain both endocervical and ciliated lower uterine segment type glands (the term polyp of mixed endometrial endocervical type may be used in such cases)
- Endometrial hyperplasia:
- Usually not polypoid
- Usually a diffuse process, involving the entire endometrium
- May be confused with hyperplasia arising in an endometrial polyp; will see background endometrial hyperplasia and lack of thick walled vessels
- Endometrial stromal tumor:
- Uniform oval small cells, enveloped by reticulin fibers
- Small vessels characteristically encircled by reticulin fibers
- Does not have dilated glands or thick walled blood vessels
- Endometritis:
- Typical morphological features of polyp are absent, such as polypoid shape and thick walled vessels
- Leiomyoma (intracavitary / submucosal):
- Smooth muscle with fascicular growth pattern
- Dilated glands and thick walled vessels are not seen
- On hysteroscopy, generally white and firm, with surface blood vessels
- Lower uterine segment endometrium:
- Polypoid shape and thick walled blood vessels are typically not present
- Secretory endometrium:
- Secretory endometrium corresponds to a cyclical endometrium (secretory in type) which can be seen in the background endometrium
- Endometrial polyp with atypical stromal cells may have to be differentiated from the following:
- Adenosarcoma:
- Extent of stromal atypia is greater (usually diffuse or multifocal)
- Atypia is uniformly severe
- Stromal hypercellularity with periglandular stromal cuffing and cambium layer underneath the glandular component
- Leaf-like projections into glandular lumina
- > 3 mitoses/10 high power fields
- Trophoblastic cells:
- Location is important (implantation site nodule or recent implantation site, instead of a polyp)
- Cells dispersed individually or in loose aggregates, surrounded by fibrinoid material
- Mononuclear trophoblast cells have polygonal shape, abundant pale eosinophilic cytoplasm and round uniform nuclei
- Syncytiotrophoblast is characteristically multinucleated
- Endometrial stromal sarcoma:
- Expansile proliferation of spindle cells resembling endometrial stroma (usually producing a mass effect, instead of atypical cells in polyps which are usually incidental)
- Tightly packed uniform spindled cells without significant glandular elements
- Smaller capillary type vessels distributed evenly
- Infiltration into myometrium
- Malignant mixed Müllerian tumor (MMMT):
- Malignant appearing epithelial component
- Stromal component shows diffuse severe atypia
- High mitotic activity in stroma
- Adenosarcoma:
Board review style question #1
Board review style answer #1
B. 6p21 aberrations. The histology is consistent with endometrial polyp. The most common cytologic abnormality associated with endometrial polyps are aberrations of chromosome 6p21. Aberrations of chromosome 1p, 9q34 and loss of 7q are associated with uterine leiomyoma.
Comment Here
Reference: Endometrial polyp
Comment Here
Reference: Endometrial polyp
Board review style question #2
Tamoxifen related endometrial polyps are frequently associated with which of the following?
- Epithelial and stromal metaplasia
- Hypercellular stroma
- Malignant transformation in up to 10%
- Unique cytogenetic profile
Board review style answer #2
A. Epithelial and stromal metaplasia. Tamoxifen related endometrial polyps are generally larger, sessile with bizarre stellate shapes and frequent epithelial and stromal metaplasia. They may show stromal fibrosis and periglandular stromal condensation. Malignant transformation can be seen in up to 3% of cases. Interestingly, their cytogenetic profile is similar to noniatrogenic lesions.
Comment Here
Reference: Endometrial polyp
Comment Here
Reference: Endometrial polyp