Table of Contents
Definition / general | Essential features | Terminology | Diagrams / tables | Sonographic features of thyroid nodules and lymph nodes | Reporting systems | Advanced imaging approaches | Clinical features | Radiology description | Radiology images | Case reports | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jug R, Jiang X. Ultrasound. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidultrasound.html. Accessed April 25th, 2024.
Definition / general
- Ultrasound is an imaging modality based upon sound waves that has several modes that are helpful to visualize thyroid anatomy and blood flow
- Basic physics principles:
- Ultrasound probe both emits and receives sound waves
- Medical ultrasound: 2 - 20 MHz
- Lower frequencies: better penetration, lower resolution
- Higher frequencies: lower penetration, higher resolution
- B mode (brightness mode):
- 2D black and white image in < 1 mm slice
- Emitted waves are reflected back from the target material relative to the degree of the material's acoustic impedance, which is dependent on density
- Higher density materials generally reflect more and look brighter
- For example, bone is more reflective than soft tissue; thus, bony structures appear brighter on ultrasound images in contrast to darker surrounding tissue
- Doppler mode:
- Measures direction and speed of tissue / blood motion
- M mode (motion mode):
- Pulses are emitted in quick succession and each time, an image is taken; over time, this is analogous to recording a video in ultrasound (used for heart valves)
- References: Arch Pathol Lab Med 2010;134:1541, Radiol Clin North Am 2011;49:417
Essential features
- Ultrasound is an imaging modality based upon sound waves that has several modes that are helpful to visualize thyroid anatomy and blood flow
- Benign thyroid nodules appear small or large with predominant cystic change, fluid filled (as opposed to solid), hyperechoic or honeycomb morphology
- Thyroid nodules suspicious for malignancy are solid, are taller than they are wide, contain microcalcifications and are hypoechoic, with thin capsules or irregular borders and intramodular vascularity
Terminology
- Anechoic: black (e.g., blood, cystic fluid)
- Azimuthal plane: midsagittal plane of transducer; beam used to guide needle in ultrasound guided fine needle aspiration (UGFNA)
- Hyperechoic: brighter than surrounding tissue (e.g., bone)
- Hypoechoic: darker than surrounding tissue (e.g., soft tissue versus bone)
- Isoechoic: same intensity as surrounding tissue
- Ultrasound artifacts:
- Posterior (acoustic) shadowing: strong reflectors (air) or absorbers (stones, bones) block visualization of structures beyond them in relation to the beam
- Posterior (acoustic) enhancement: anechoic structures (cysts) show brighter signals from areas beyond them in relation to the beam
- Eggshell calcification: nodules surrounded by a layer of calcium have bright anterior and posterior walls due to a reflection from the surface but posteriorly there is acoustic shadowing; this phenomenon also leads to edge artifact in which parallel dark lines extend posteriorly from the sides of nodules
- Reverberation artifact: sound waves reflect off a very reflective surface and are re-reflected from the skin, resulting in phantom images behind the target image
- Comet tail artifact: reverberation artifact from front and back of a very strong reflector / absorber (air bubble, metal fragment) - can also happen with dense colloid
- Bayonet sign:
- Due to speed propagation artifact, machines use average speed of sound to calculate depth
- If sound actually travels faster in the tissue (anechoic or hypoechoic structures), a reflector will appear closer to the transducer than its actual depth and vice versa
- Needle with its tip in a cyst or nodule with differing echogenicity from surrounding tissue will appear to have its tip bent due to this artifact, looking like a bayonet
- References: Arch Pathol Lab Med 2010;134:1541, Radiol Clin North Am 2011;49:417, Korean J Radiol 2014;15:267, Endotext: Ultrasonography of the Thyroid [Accessed 12 October 2022], Radiol Clin North Am 2020;58:1033, Radiol Clin North Am 2020;58:1041, Milas: Advanced Thyroid and Parathyroid Ultrasound, 1st Edition, 2017, Halenka: Atlas of Thyroid Ultrasonography, 1st Edition, 2017
Diagrams / tables
Contributed by Rachel Jug, M.B.B.Ch.
Images hosted on other servers:
Typical appearances of diffuse thyroid diseases
| Thyroid disorder | Grayscale ultrasound | Color Doppler | Key features |
|---|---|---|---|
| Graves thyroiditis | Enlarged, mildly hypoechoic, heterogeneous | Markedly ↑ | Markedly hyperemic; proptosis; hyperthyroid; + antithyroid antibodies |
| Hashimoto thyroiditis | Enlarged, heterogeneous with lobular margins; hypoechoic and micronodular, septal lines | Highly variable: both ↑ and ↓ flow possible | + Antithyroid antibodies, hypothyroidism; cervical adenopathy |
| Subacute lymphocytic thyroiditis (painless) | Hypoechoic | Insufficient data | + Antithyroid antibodies; postpartum; transient |
| De Quervain thyroiditis (subacute granulomatous) | Painful patchy areas of hypoechogenicity | ↓ in the hypoechoic patch | Thyroid pain over area of hypoechogenicity; ↑ erythrocyte sedimentation rate (ESR) |
| Acute suppurative thyroiditis | Abscess or infected linear tract in the thyroid | Normal background; no flow within an abscess | Acute presentation with signs of infection and pain; ↑ ESR; possible pyriform sinus fistula |
| Riedel thyroiditis | Large hypoechoic thyroid with coarse parenchyma | Insufficient data | Large, rock hard gland; encases adjacent structures |
| Medication induced (i.e., amiodarone induced thyrotoxicosis [AIT]) | Type 1: abnormal thyroid; type 2: normal thyroid | Type 1: ↑; type 2: absent | History of current or recent amiodarone use; hyperthyroid |
| Atrophic thyroiditis | Small, hypoechoic thyroid | ↓ | + Antithyroid antibodies; usually hypothyroid |
| Radiation thyroiditis | Small, hypoechoic thyroid | Variable | Known external beam or I131 administration |
| Thyroid lymphoma | Large, ill defined, markedly hypoechoic nodules or masses with ↑ through transmission on background of Hashimoto thyroiditis | ↓ in the hypoechoic mass | Rapidly enlarging neck mass in patient with history of Hashimoto, with or without adenopathy |
| Multinodular goiter | Closely opposed or interspersed, similar appearing nodules replace parenchyma, coarse calcifications, variable cystic changes in nodules | Variable | Confluent nodules in a normal or enlarged thyroid; with or without abnormal thyroid function tests |
Sonographic features of thyroid nodules and lymph nodes
- Sonographic features of benign thyroid nodules:
- Small size (< 1 cm)
- Fluid filled
- Honeycomb morphology
- Hyperechoic (colloid nodule or focal nodular Hashimoto thyroiditis)
- Large nodules if they are predominantly cystic (cystic change accounts for > 50% of nodule)
- Sonographic features of thyroid nodules suspicious for malignancy (Diagn Cytopathol 2008;36:390, Eur J Endocrinol 2009;161:103):
- Solid oval nodules (anterior - posterior dimension: transverse dimension ratio is > 1)
- Presence of discrete coarse echogenic foci or microcalcifications
- Hypoechoic (medullary and papillary thyroid cancers)
- Thin capsules or irregular borders (suggestive of extracapsular spread)
- Intranodular vascularity
- Nodal metastases
- Sonographic features of benign lymph nodes:
- Oval shape (short axis:long axis ratio ≤ 0.5)
- Hypoechoic cortex and echoic hilum (due to adipose tissue)
- Clearly demarcated margin from surrounding tissue
- Central vascularization
- Sonographic features of lymph nodes suspicious for malignancy (Eur J Endocrinol 2009;161:103):
- Round shape (short axis:long axis ratio > 0.5)
- Echogenic heterogeneity of cortex and absent fatty hilum
- Irregular margin with surrounding tissue
- Increased or abnormally located vascularity
- Features suggestive of metastatic thyroid cancer: cystic appearance, hyperechoic punctations / calcifications
- 2015 American Thyroid Association (ATA) Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer (Thyroid 2016;26:1):
- Strongly recommends ultrasonic examination of thyroid and cervical lymph nodes if thyroid nodules; fine needle aspiration (FNA) for sampling is recommended if > 1 cm in greatest dimension and high suspicion sonographic pattern (estimates a 70 - 90% risk of malignancy), including:
- Solid hypoechoic nodule or nodule that is partially solid and hypoechoic and partially cystic with 1 or more of the following features:
- Irregular margins (infiltrative, microlobulated)
- Microcalcifications
- Oval (taller than wide) shape
- Rim calcifications with an extrusive soft tissue component
- Evidence of extrathyroidal extension
- Solid hypoechoic nodule or nodule that is partially solid and hypoechoic and partially cystic with 1 or more of the following features:
- Strongly recommends ultrasonic examination of thyroid and cervical lymph nodes if thyroid nodules; fine needle aspiration (FNA) for sampling is recommended if > 1 cm in greatest dimension and high suspicion sonographic pattern (estimates a 70 - 90% risk of malignancy), including:
Reporting systems
- American College of Radiology (ACR) Thyroid Imaging, Reporting and Data System (TI-RADS) categorizes lesions based on ultrasound features and provides recommendations for whether or not to FNA the lesion:
- Benign (TR1): no FNA
- Not suspicious (TR2): no FNA
- Mildly suspicious (TR3): FNA if ≥ 2.5 cm; follow if ≥ 1.5 cm
- Moderately suspicious (TR4): FNA if ≥ 1.5 cm; follow if ≥ 1 cm
- Highly suspicious (TR5): FNA if ≥ 1 cm; follow if ≥ 0.5 cm
- See ACR TI-RADS chart
- Modifications of TI-RADS:
- European: EU TI-RADS (Eur Thyroid J 2017;6:225)
- Korean: K TI-RADS (Korean J Radiol 2021;22:1569)
- Chinese: C TI-RADS (Endocrine 2020;70:256)
Advanced imaging approaches
- Thyroid elastography: characterizes thyroid nodules by determining hardness / stiffness; can be integrated into the conventional thyroid ultrasound (Ultraschall Med 2009;30:175)
- Stiffness measured in kPa and elasticity ratios comparing cancerous to benign tissue
- Lesions with low stiffness are considered to be benign, while stiff lesions are considered to be malignant (Diagn Interv Imaging 2013;94:535, Ultraschall Med 2009;30:175)
- Contrast enhanced ultrasound (CEUS): qualitative and quantitative approach to analyze the microvascular patterns of thyroid nodules and lymph nodes to characterize them as benign or malignant
- Method increases diagnostic accuracy of ultrasonography (J Clin Med 2021;10:4559)
Clinical features
- Indications for UGFNA:
- Nonpalpable or difficult to palpate nodules, most commonly of the thyroid
- Targeting specific areas in complex and cystic nodules, such as solid areas
- Repeat FNA, when a prior palpation guided FNA sample was insufficient (Diagn Cytopathol 2008;36:390)
- Follow up for patients postpartial or total thyroidectomy for malignancy, e.g., to sample thyroid bed (J Ultrasound Med 2013;32:1319)
- Benefits of UGFNA compared to conventional FNA alone:
- Higher rates of successful biopsy (J Clin Ultrasound 1994;22:535, Thyroid 1998;8:15, Thyroid 1998;8:283)
- Potentially lowers risk of damage to surrounding structures, which can be visualized
- Varying reports on cost effectiveness (BMC Endocr Disord 2009;9:14, Thyroid 2006;16:555)
- Efficacy of UGFNA is improved by the presence of a cytopathologist onsite, decreasing the overall inadequacy rate from 9.3% to 6% (Br J Radiol 2014;87:20130571)
- Complications and contraindications: same as conventional FNA
- Overview of procedure - focused thyroid ultrasound and biopsy:
- Image each thyroid lobe in the transverse and longitudinal planes to determine the overall appearance and locate nodules
- After completing ultrasonic assessment of the thyroid, relocate the position and measure size of the suspicious nodules
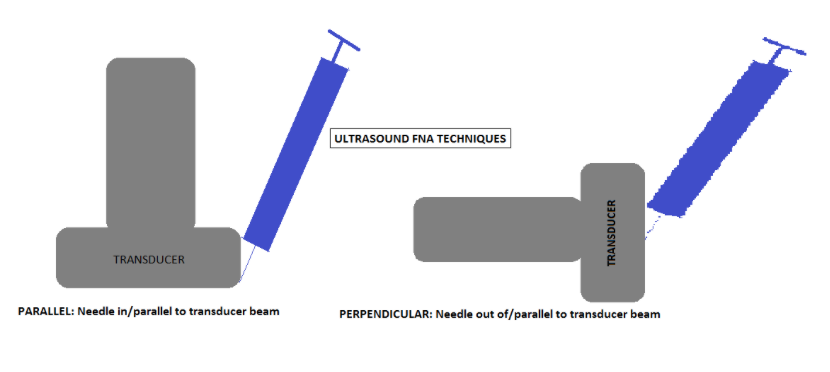
- Approaches to UGFNA relative to the transducer beam (azimuthal plane):
- For each approach, orient the needle with the bevel tip up to create the greatest reflection
- Parallel approach (in beam):
- Point the needle down, along the plane of the beam, toward the nodule
- Maintain needle and transducer in the same plane, parallel to the plane of the transducer, then advance the needle into the nodule
- Advantage: entire length of needle can be seen
- Perpendicular approach (out of beam):
- Point the needle toward the midpoint of the transducer's side (long axis)
- Perpendicular approach will result in visualization of the needle as it transversely crosses the plane of the beam at 90 degrees
- Nodule and needle point will be centered in the midpoint of the transducer's long axis
- Advantage: desirable, due to anatomy in some locations
- Disadvantage: entire length of needle is not visualized
- Needle based sample collection techniques:
- With aspiration / suction:
- 27 or 25G needle attached to a 10 cc syringe (with or without extension tubing) withdrawn so that 1 - 2 cc of negative pressure induces aspiration
- Without aspiration / nonsuction:
- 27 or 25G needle (with or without stylet; may attach open syringe) is introduced into nodule and capillary action causes uptake of cellular material into the needle
- With aspiration / suction:
- Sample preparation: same as for palpation guided FNA
Radiology description
Radiology images
Images hosted on other servers:
Case reports
- 18 year old woman with a mass in her left neck with stiffness and normal thyroid function (Medicine (Baltimore) 2021;100:e25517)
- 24 year old woman with a palpable painless mass in the left thyroid lobe (J Int Med Res 2020;48:300060520954718)
- 71 year old woman with swelling of the anterior neck and history of airway obstruction (J Ultrasound 2018;21:165)
Videos
Fine needle aspiration (FNA) biopsy techniques - Dr. Britt Marie Ljung playlist
Neck ultrasonography basics
Thyroid ultrasound course
Additional references
Board review style question #1
Board review style answer #1
E. Presence of discrete coarse echogenic foci or microcalcifications
Comment Here
Reference: Ultrasound guided FNA
Comment Here
Reference: Ultrasound guided FNA
Board review style question #2
What is the typical appearance of chronic lymphocytic (Hashimoto) thyroiditis on a grayscale ultrasound?
- Abscess or infected linear tract in the thyroid
- Enlarged, heterogeneous with lobular margins; hypoechoic and micronodular, septal lines
- Enlarged, mildly hypoechoic, heterogeneous
- Large, ill defined, markedly hypoechoic nodules or masses
- Small, hypoechoic thyroid
Board review style answer #2
B. Enlarged, heterogeneous with lobular margins; hypoechoic and micronodular, septal lines
Comment Here
Reference: Ultrasound guided FNA
Comment Here
Reference: Ultrasound guided FNA