Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Bychkov A. Parasitic nodule. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidparasiticnodule.html. Accessed April 26th, 2024.
Definition / general
- Peripheral nodule of goiter that is anatomically separate from the main thyroid gland (Arch Otolaryngol Head Neck Surg 1996;122:1409)
- Spontaneous detachment of thyroid tissue with subsequent implant in the lateral neck may occur in nodular goiter or Hashimoto thyroiditis
- Diagnostic criteria (Histopathology 2006;49:107):
- Parasitic nodule should be in same fascial plane as thyroid gland and exhibit a similar histologic appearance as the main gland
- No evidence of lymph node structures
- Similar separated nodules are described in uterine myoma (Obstet Gynecol 2009;114:611)
Terminology
- Also called sequestered (i.e. sequestered goiter), detached or accessory thyroid nodule
- Recommended to use "parasitic nodule" for separated thyroid nodules in lateral neck, as opposed to midline ectopic thyroid tissue along the thyrothymic tract, which is mainly a developmental abnormality (Virchows Arch 1999;434:241)
- Lateral aberrant thyroid often represents parasitic thyroid nodule
Epidemiology
- F:M = 4:1, median age is 51 years (range 15 to 83 years)
- ~100 cases have been reported; the largest series was from Dr. Rosai (Lab Invest 2006;86:96A)
Sites
- Perithyroidal, close to the gland (< 1 cm)
- Can be located in the lateral neck from the submandibular to the retroclavicular area, the sternocleidomastoid and sternohyoid muscles (Lab Invest 2006;86:96A)
- Rarely found in the mediastinum as part of a substernal nodular goiter (Arch Intern Med 1983;143:1015)
Pathophysiology / etiology
- Portion of goitrous thyroid extending through the fascia may be separated by the mechanical action of neck muscles, and remains connected to the main gland by a thin fibrous strand of vascular tissue (Boston Med Surg J 1903;149:616)
- Split from thyroid gland is due to ablation of pre-existing connection or lack of identification of connection to the main gland (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
- Alternatively, parasitic nodule may represent concurrent hyperplastic changes in accessory thyroid tissue (N Engl J Med 1964;270:927)
- Blood supply may be obtained from thyroid via fibrovascular pedicle, or be autonomous, acquired from the surrounding tissues (ISRN Surg 2011;2011:313626)
Clinical features
- Palpated in the lateral neck (N Engl J Med 1964;270:927)
- The nodule is usually an expression of nodular hyperplasia or nodular Hashimoto thyroiditis, less commonly of Graves disease (Histopathology 2006;49:107)
- Benign condition. but some cases of metastatic thyroid carcinoma from occult primary may be initially misdiagnosed as parasitic nodules
- Rodriguez found malignancy without evidence of tumor in the main gland in 10% of studied parasitic nodules, and suggested that parasitic nodule can originate in a primary tumor (Lab Invest 2006;86:96A), but microcarcinoma in the main thyroid cannot be excluded
Diagnosis
- On histopathology, after exclusion of metastatic cancer
Radiology description
- RAI uptake in a nodule separate from thyroid (N Engl J Med 1964;270:927)
- Sonography: the main gland is multinodular, but parasitic nodules imitate enlarged cervical lymph nodes (Endocrinol Diabetes Metab Case Rep 2014;2014:140027)
Radiology images
Case reports
- 40 year old man with parasitic thyroid nodules and nontoxic multinodular goiter (J Med Case Rep 2014;8:66)
- 53 year old woman with parasitic thyroid nodule and Hashimoto chronic thyroiditis (Rev Hosp Clin Fac Med Sao Paulo 2000;55:65)
- 58 year old woman with parasitic thyroid nodules (Endocrinol Diabetes Metab Case Rep 2014;2014:140027)
- 67 year old woman with parasitic nodule of the thyroid and Graves disease (Virchows Arch 1999;434:241)
- 80 year old woman with ectopic sequestered thyroid tissue (ISRN Surg 2011;2011:313626)
- Young woman with sequestered substernal goiter (Arch Intern Med 1983;143:1015)
- Parasitic nodule of thyroid in neck of patient with family history of papillary thyroid carcinoma (Endocr Pathol 2015;26:273)
- Scintigraphic demonstration of sequestered nodular goiter (Clin Nucl Med 1992;17:402)
- Parasitic nodule of the right carotid triangle (Arch Otolaryngol Head Neck Surg 1996;122:1409)
Treatment
- Usually removed surgically to rule out metastasis
Gross description
- 0.5 - 6.5 cm nodule, separate from thyroid gland, usually single (> 80%)
- Fibrovascular pedicle connecting to the main thyroid can be discovered after careful dissection at surgery
- Often nodular or shows changes similar to the main thyroid
Gross images
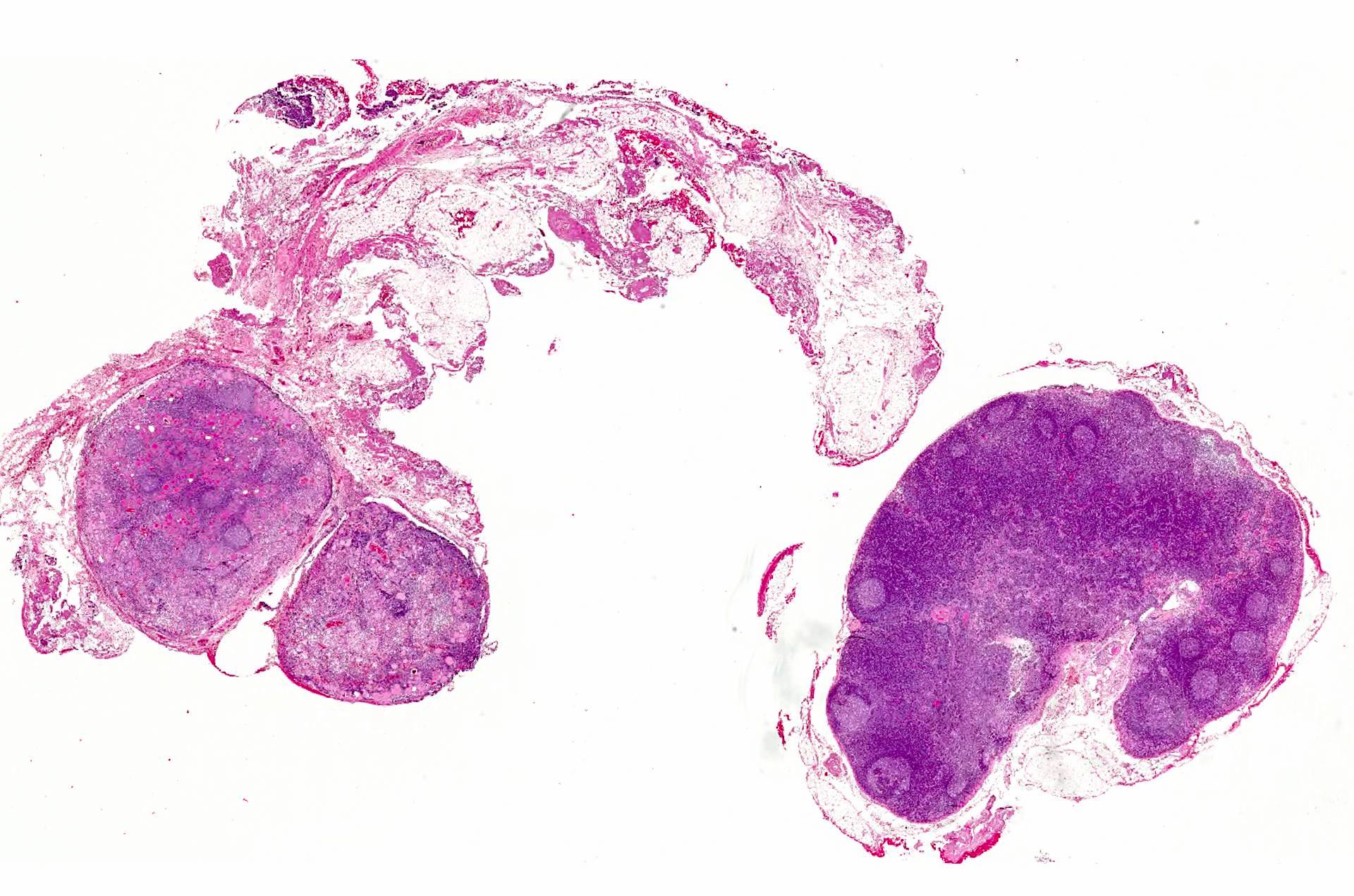
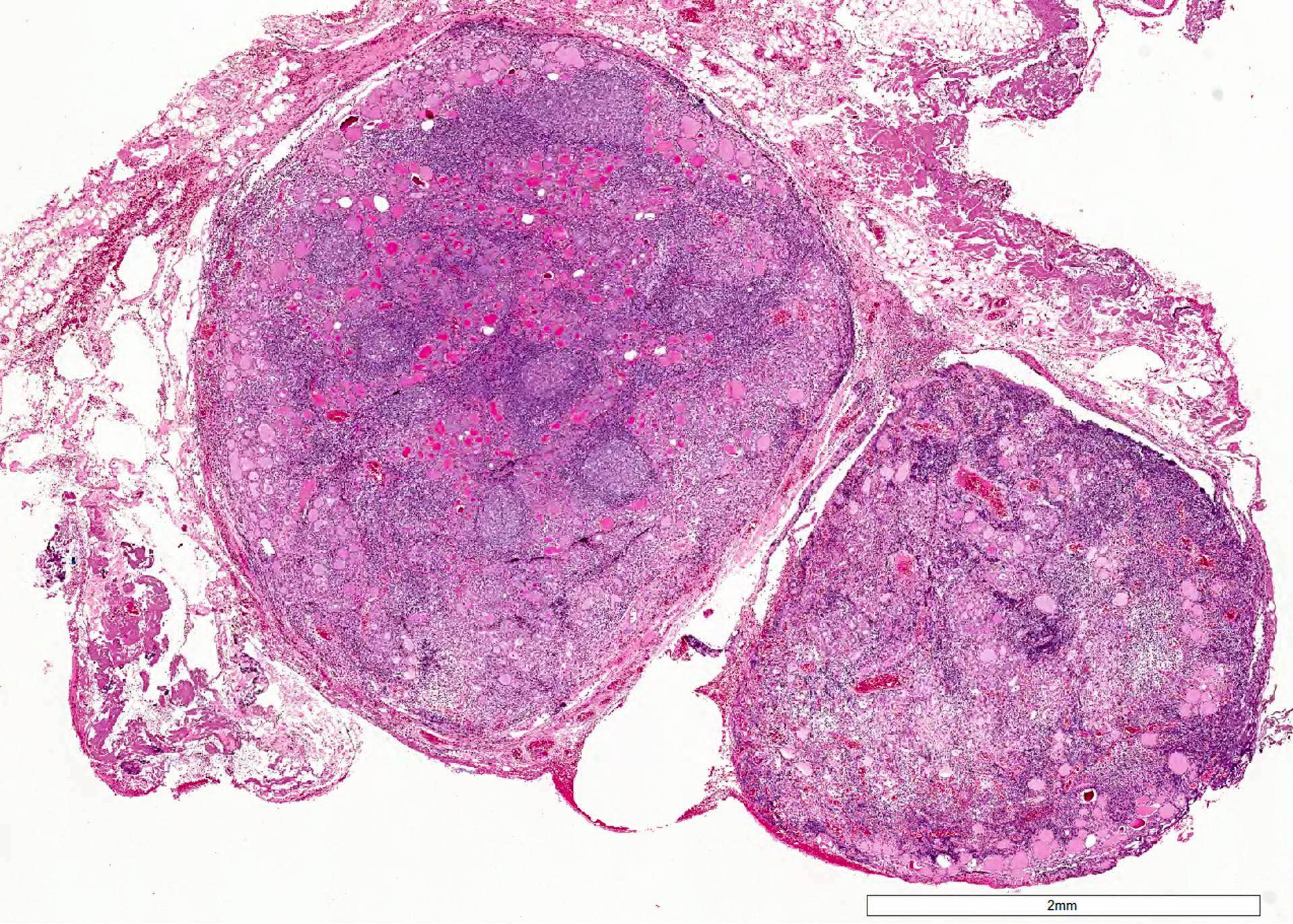
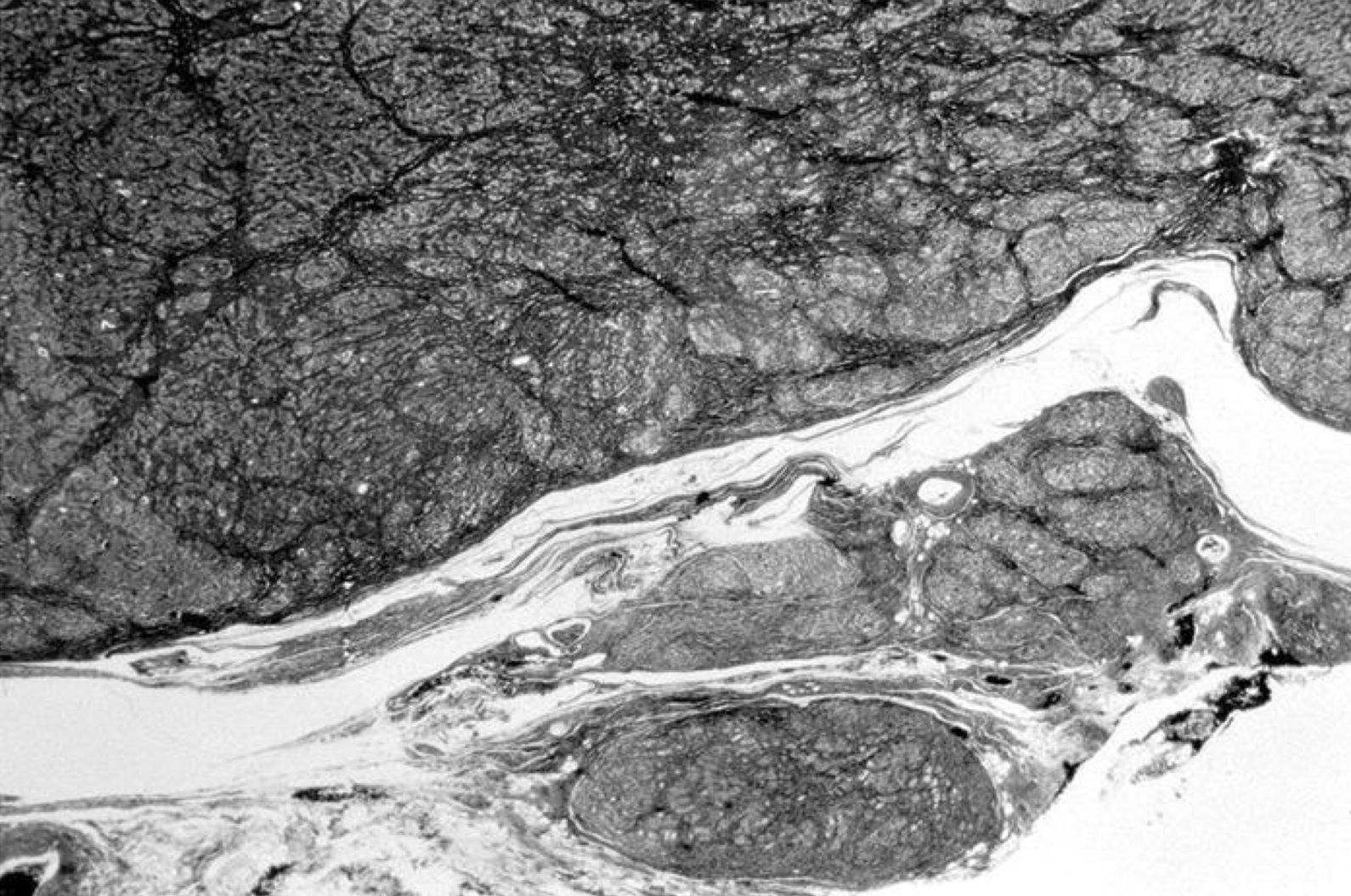
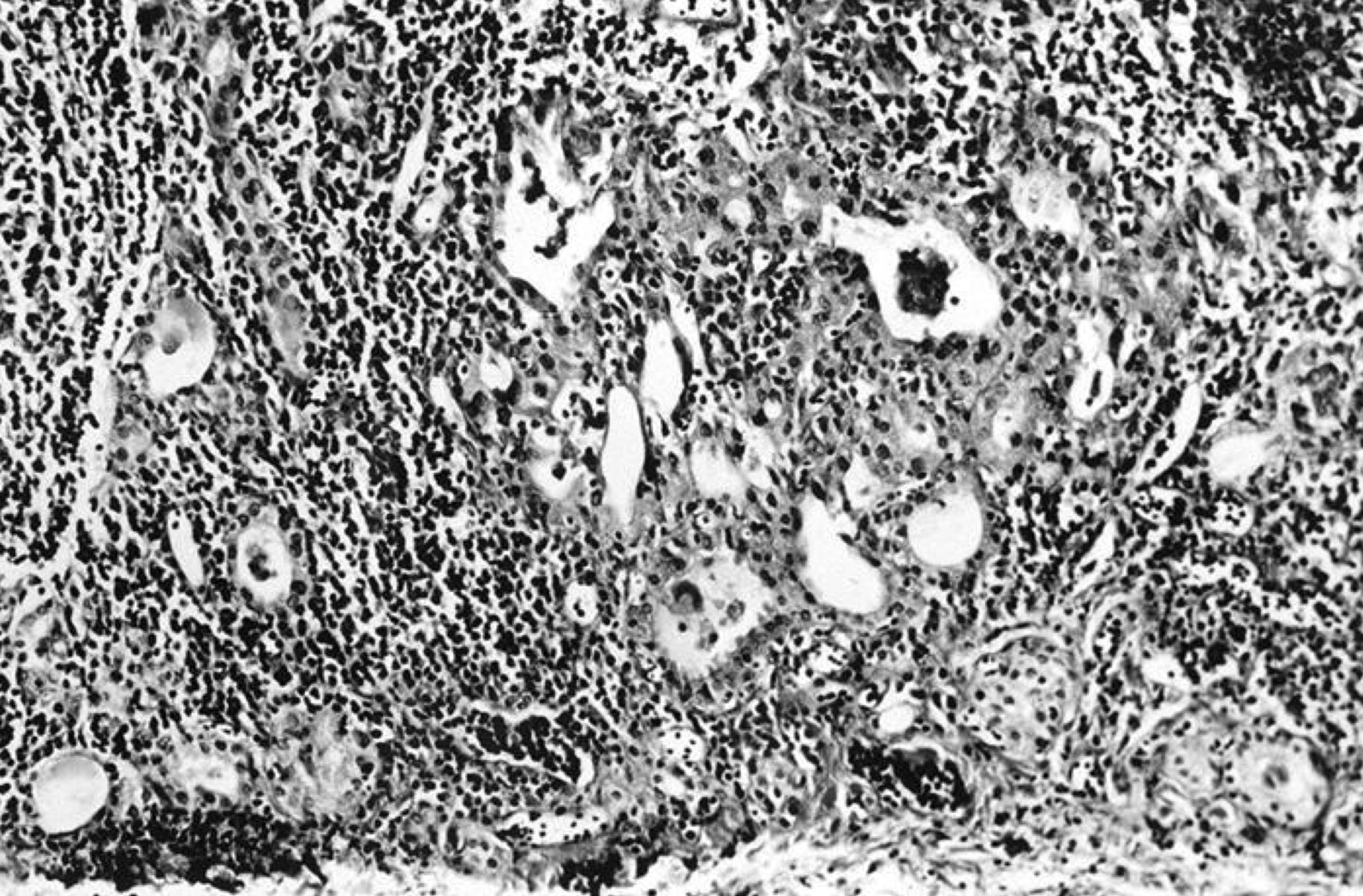
Microscopic (histologic) description
- Benign appearing thyroid tissue with colloid filled or hyperplastic follicles
- Similar features are found in orthotopic gland
- Hashimoto thyroiditis in parasitic nodule may simulate lymph node tissue
- In addition, reactive atypia in Hashimoto follicular cells with ground glass nuclei mimics papillary thyroid carcinoma (Rev Hosp Clin Fac Med Sao Paulo 2000;55:65)
Microscopic (histologic) images
Cytology description
- Thyroid follicular cells (Endocr Pathol 2015;26:273)
Molecular / cytogenetics description
- No BRAF mutation (Endocrinol Diabetes Metab Case Rep 2014;2014:140027)
- Polyclonal on HUMARA assay (Hum Pathol 1998;29:187)
Differential diagnosis
- Papillary thyroid carcinoma (nodal metastais) vs. parasitic nodule with Hashimoto thyroiditis:
- Cytological and architectural features of carcinoma
- Primary tumor in the main thyroid
- Lymph node structures, subcapsular sinuses highlighted by reticulin stain (Virchows Arch 1999;434:241)
- Displaced / seeded thyroid tissue due to prior surgery or accidental trauma (Ann Diagn Pathol 2004;8:61, Endocrinol Diabetes Metab Case Rep 2014;2014:140027):
- Often multiple and superficial / subcutaneous
- May have suture material, talc crystals, reactive fibrosis
Additional references