Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Pathophysiology / etiology | Clinical features | Diagrams / tables | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Bychkov A. Thyroid inclusions. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidlymphnodes.html. Accessed November 30th, 2024.
Definition / general
- Thyroid tissue incidentally discovered in cervical lymph nodes during histological examination of neck dissections performed for non thyroid disease, e.g. head and neck cancer (Eur Arch Otorhinolaryngol 2016;273:2867)
- May represent metastatic carcinoma or benign thyroid tissue; evaluate with extreme caution (Laryngoscope 2005;115:470)
- Metastatic carcinoma accounts for most of the cases: main primary is papillary thyroid carcinoma, often occult
- Much rarer sources of primary tumor mimicking thyroid follicles in cervical metastasis can be salivary gland, lung, thymus and struma ovarii (Rosai: Rosai and Ackerman's Surgical Pathology, 10th Edition, 2011)
- Heterotopic thyroid: true benign thyroid inclusions due to developmental abnormalities or benign lymphatic transport (Cancer 1967;20:103)
- Some authors suggested all thyroid tissue within lymph nodes was metastatic thyroid cancer (Cancer 1967;20:103); however the possibility of benign inclusions is widely accepted today (Eur Arch Otorhinolaryngol 2016;273:2867)
- Benign nodal thyroid inclusions are not unique; similar benign foci of parathyroid, salivary gland tissue and nevus cells are described in cervical lymph nodes (Diag Histopath 2010;16:265)
- Benign epithelial inclusions are found in axillary (breast) and pelvic (endometrium) lymph nodes (Miranda: Atlas of Lymph Node Pathology, 2013)
- Metastatic carcinoma accounts for most of the cases: main primary is papillary thyroid carcinoma, often occult
Terminology
- Ectopic thyroid tissue in cervical lymph nodes; benign thyroid inclusions in cervical lymph nodes
- Lateral aberrant thyroid: usually due to metastatic thyroid carcinoma in cervical lymph nodes
Epidemiology
- Incidence of unsuspected benign thyroid tissue in lymph nodes of patients with head and neck carcinoma treated with neck dissection is 0.6% - 1.5% (Clin Endocrinol Metab 1981;10:337, Laryngoscope 2005;115:470)
- Meticulous study of cervical lymph nodes found benign thyroid inclusions in 4.7% of unselected autopsies (Cancer 1969;24:302)
- Total number of well proven cases of benign nodal thyroid inclusions is < 30
Sites
- Benign thyroid inclusions involve medial inferior neck lymph nodes, whereas any thyroid tissue found lateral to large neck vessels (carotid artery or jugular vein) should be considered metastatic tumor rather than a developmental anomaly (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
- However, there are occasional cases of benign inclusions in lateral (up to level II) lymph nodes (Eur Arch Otorhinolaryngol 2016;273:2867)
Pathophysiology / etiology
- Aberrations during migration of embryonic thyroid may result in entrapment of structures that terminally differentiate to thyroid follicles and remain quiescent in lymph nodes (heterotopia)
- In addition, hypothetically, enlarging lymph node may enclose neighboring ectopic islet of thyroid tissue
- May be explained by benign lymphatic transport ("benign metastasis"), when tiny fragments of ruptured thyroid tissue float into sentinel lymph nodes (JAMA 1965;194:1); similar to proposed mechanism for endometriosis
- Theoretically, may represent nodal metastasis of occult thyroid carcinoma with further complete regression of the primary (Head Neck 2001;23:885, J Oral Maxillofac Surg 2008;66:2566)
Clinical features
- Asymptomatic and incidental by definition
- Some authors propose that primary papillary carcinoma can arise in ectopic intranodal thyroid tissue, regardless of the main thyroid (J Oral Maxillofac Surg Med Pathol 2015;27:240)
- Potentially may mimic thyroid cancer in thyroglobuin+ washouts of cervical lymph nodes (J Clin Endocrinol Metab 2013;98:1061)
Diagnosis
- Only after exclusion of suspected primary thyroid carcinoma on extensive workup (imaging and even surgery)
Radiology description
- It is believed that current imaging modalities are unable to detect true benign nodal thyroid inclusions (Eur Arch Otorhinolaryngol 2016;273:2867)
- Features suggestive of metastatic lymph nodes from papillary thyroid carcinoma (Head Neck 2015;37:E106):
- US: focally or diffusely increased nodal echogenicity, intranodal calcifications, intranodal cystic component(s) and an abnormal vascular pattern (a chaotic or peripheral vascular pattern)
- CT: strong enhancement without hilar vessel enhancement, heterogeneous enhancement, intranodal calcifications and intranodal cystic component
Prognostic factors
- The prognosis for benign nodal thyroid inclusions is excellent
- Similarly, occult papillary thyroid carcinoma with incidental nodal micrometastasis usually does not progress
Case reports
- 13 year old boy with ectopic thyroid in lateral lymph nodes (J Pediatr Endocrinol Metab 2015;28:227)
- 41 year old man with apparent primary papillary thyroid carcinoma in lateral cervical lymph node (Exp Mol Pathol 2007;82:91)
- 50 year old woman with primary papillary carcinoma arising from ectopic thyroid tissue in the cervical lymph node (J Oral Maxillofac Surg Med Pathol 2015;27:240)
- 51 year old woman with benign intranodal thyroid tissue mimicking nodal metastasis in a patient with papillary thyroid carcinoma (Head Neck 2015;37:E106)
Treatment
- Thyroid imaging is mandatory for all cases with thyroid inclusions in cervical lymph nodes
- If primary thyroid carcinoma is detected, the extent of further thyroid surgery depends on age, comorbidities, control of primary upper aerodigestive cancer and patient preference
- "Wait and watch" is recommended if imaging is negative
- Option of further surgery can be considered as well
- Unequivocally benign inclusions confirmed by morphology and negative thyroid imaging may require no further action but clinical correlation and follow up is advisable (Eur Arch Otorhinolaryngol 2016;273:2867)
Gross description
- Lymph nodes are unremarkable, < 5 mm (range 2 - 15 mm)
Microscopic (histologic) description
- Inclusions are 0.1 to 2.3 mm and contain up to 100 (average 30) normal appearing thyroid follicles, usually arranged in a wedge shaped focus with the base adjacent to the nodal capsule and the apex directed towards the cortex (Eur Arch Otorhinolaryngol 2016;273:2867)
- Benign inclusion should be located within the nodal capsule or in the marginal sinus (subcapsular) and in not more than two cervical lymph nodes
- Metastatic papillary carcinoma is suspected by the large extent of thyroid tissue replacing lymph node (often cystic) and the presence of papillary structures, psammoma bodies, grooved nuclei, marginated chromatin, intranuclear pseudoinclusions
- The same features of papillary cancer can be found in the thyroidectomy specimen, which may require exhaustive sectioning, including multiple levels and "flipping" of paraffin blocks (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
Microscopic (histologic) images
Cytology description
- The probability of obtaining tiny benign thyroid inclusions during cervical lymph node aspiration is extremely low, with only one case reported (Head Neck 2015;37:E106)
- As such, the presence of thyroid follicles in cervical lymph node aspirate should be considered to be metastatic thyroid carcinoma or a technical error (if orthotopic or heterotopic thyroid/parasitic nodule is sampled instead of the lymph node)
- Metastases in lymph nodes are identified by papillary fragments, psammoma bodies and classic nuclear features of papillary thyroid carcinoma
Positive stains
- Thyroglobulin and TTF1, with these limitations:
- Macrophages in lymph nodes draining thyroid tumors may engulf thyroglobulin (J Clin Pathol 2001;54:314)
- TTF1 is not entirely thyroid specific, e.g. TTF1+ lung cancer can metastasize to cervical lymph nodes
Negative stains
- Immunomarkers of papillary thyroid carcinoma: CK19, galectin 3, HBME1 (APMIS 2001;109:875)
Molecular / cytogenetics description
- Benign inclusions are typically negative for molecular markers of thyroid cancer (BRAF and RAS mutations, RET / PTC rearrangements), although one study found BRAF mutation in "benign" inclusions (Endocr Pathol 2006;17:183)
- Benign inclusions, as with normal or ectopic thyroid, are polyclonal on HUMARA assay, but metastatic tumor is monoclonal (Hum Pathol 1998;29:187)
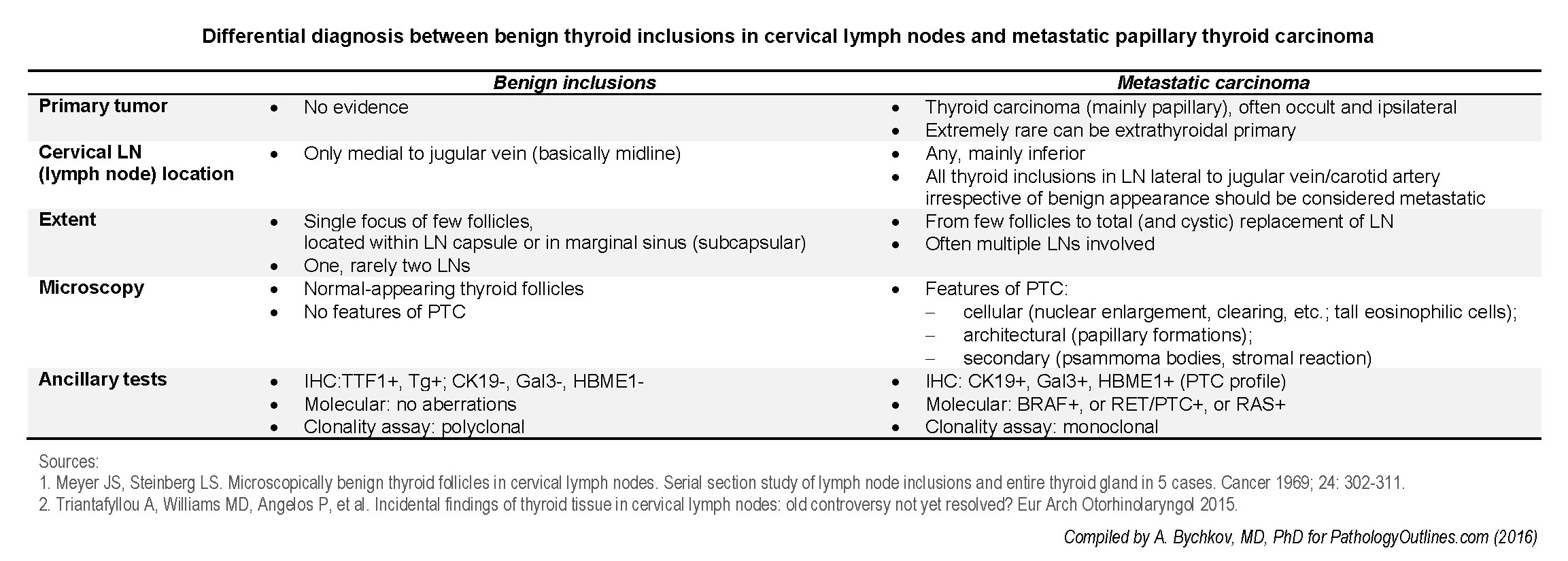
Differential diagnosis
- Metastatic carcinoma:
- Metastasis of conventional papillary thyroid carcinoma, often from occult primary, see table for details
- Other types of metastatic thyroid cancer: medullary, follicular and follicular variant of papillary carcinoma
- Metastasis from extrathyroid primary: salivary gland, lung, thymus and struma ovarii
- Conditions unrelated to lymph node that can be detected by the absence of typical nodal structures, e.g. subcapsular sinuses:
- Parasitic nodule with Hashimoto thyroiditis
- Heterotopic thyroid
- Branchial cleft cyst
Additional references